Who Are More Likely To Develop Parkinson’s Disease
Parkinson’s disease affects both men and women, though about 50% more men are affected than women. The reasons for this are unclear but there are theories that estrogen may cause women to develop the disease less frequently, and when they do, they seem to get a milder form of it. The National Institute of Neurological Disorders and Stroke estimates about 50,000 people are diagnosed with PD each year in the U.S. However, this number may be higher due to the fact that many people in the early stages of PD assume their symptoms are due to aging and do not seek medical attention. Complicating the diagnosis is that symptoms of Parkinson’s resemble other diseases and there is no one definitive test to diagnose it.
Physical Examination And Tests
A trip to the neurologists office often includes what seems like dozens of questions, along with multiple tests.
There currently are no diagnostic blood tests for Parkinson’s disease, but your doctor may do some routine blood and urine tests to assess your overall health. Your blood pressure will be taken sitting and standing to look for orthostatic hypotension.
A movement disorder specialist will do a variety of physical tests to assess you as well.
Passive Manipulation Of Limbs
To test for the presence of rigidity, we need to passively manipulate the limbs of the patient. However, If the disease is in its early stage or the symptoms are well controlled with medications, we may not be able to see rigidity. We will need to use some activation maneuvers, that basically consist in performing repetitive movements with the limb contralateral to the one that is being tested.
Also, there are two types of rigidity:
– Lead-pipe rigidity: where the tone is uniformly and smoothly increased throughout the entire range of movement
– Cogwheel rigidity: where a tremor is superimposed on the hypertonia, making the movement irregular due to intermittent increase and reduction of tone
Upper Extremity Testing
For the upper extremity the most sensitive joint where to check for rigidity is the wrist. To uncover rigidity, passively rotate the wrist and feel for a resistance to the movement. It is very important that the arm of the patient is fully relaxed when rotating the wrist. To do this, place your proximal hand under the patients forearm, while your distal hand grabs and rotates the wrist of the patient. When rigidity is present, the range of motion will be preserved but you will feel a resistance in performing the movement.
Wrist rotation with activation maneuver.
It is also possible to test for rigidity in the elbow by passively flexing and extending the forearm.
Elbow flexion-extension with activation maneuver.
Lower Extremity Testing
Also Check: Can A Person With Parkinson’s Disease Drive A Car
Referral To A Specialist
If your GP suspects Parkinson’s disease, you’ll be referred to a specialist.
This will usually be:
- a neurologist, a specialist in conditions affecting the brain and nervous system
- a geriatrician, a specialist in problems affecting elderly people
The specialist will most likely ask you to perform a number of physical exercises so they can assess whether you have any problems with movement.
A diagnosis of Parkinson’s disease is likely if you have at least 2 of the 3 following symptoms:
- shaking or tremor in a part of your body that usually only occurs at rest
- slowness of movement
- muscle stiffness
If your symptoms improve after taking a medication called levodopa, it’s more likely you have Parkinson’s disease.
Special brain scans, such as a single photon emission computed tomography scan, may also be carried out in some cases to try to rule out other causes of your symptoms.
Living Well With Parkinson’s
While medication and DBS surgery are the most effective treatments for PD, individuals often choose to delay these treatments because of their adverse side effects. Until a therapy is developed that can halt the progression of PD, there is a significant need for strategies that provide symptom relief without causing negative side effects.
Diet, Exercise, and Stress Reduction
Findings from several studies suggest that exercise has the potential to provide relief from certain PD symptoms. Anecdotally, people with Parkinsons disease who exercise typically do better. However, many questions remain. Among them is whether exercise provides a conditioning effect by strengthening muscles and improving flexibility or whether it has a direct effect on the brain.
In an NINDS-funded trial comparing the benefits of tai chi, resistance training, and stretching, tai chi was found to reduce balance impairments in people with mild-to-moderate PD. People in the tai chi group also experienced significantly fewer falls and greater improvements in their functional capacity.
Technologies that Improve Quality of Life
You May Like: Can Depakote Cause Parkinson’s Symptoms
When Should Genetic Testing Be Done
Your physician may suggest it if your Parkinsons diagnosis comes at a young age , if multiple relatives in your family history have also been diagnosed with the same, or if you are at high risk for familial Parkinsons based on your ethnicity .
However, what is the benefit of having the testing done at the present time? The information may be important for family planning for some individuals although as I said even if the gene is passed on it does not necessarily equal development of the disease. The risk, though, is higher in dominant genetic mutations versus recessive ones, on average if a person has a first-degree relative with Parkinsons their risk of developing the disease is 4 to 9 percent more than the general population.
Keep in mind that currently for the person being tested, there is no change in the treatment of their Parkinsons disease based on genetic findings. In the future, however, when there are treatments to slow down the onset of the disease or to prevent it from developing at all, then the identification of those people at risk will be very important.
How Is Parkinson’s Disease Diagnosed
Your doctor will ask questions about your symptoms and your past health and will do a neurological exam. This exam includes questions and tests that show how well your nerves are working. For example, your doctor will watch how you move. He or she will check your muscle strength and reflexes and will check your vision.
Your doctor also may check your sense of smell and ask you questions about your mood.
In some cases, your doctor will have you try a medicine for Parkinson’s disease. If that medicine helps your symptoms, it may help the doctor find out if you have the disease.
Tests
There are no lab or blood tests that can help your doctor know whether you have Parkinson’s. But you may have tests to help your doctor rule out other diseases that could be causing your symptoms. For example:
- An MRI or CT scan is used to look for signs of a stroke or brain tumor.
- Blood tests check for abnormal thyroid hormone levels or liver damage.
Another type of imaging test, called PET, sometimes may detect low levels of dopamine in the brain. These low levels are a key feature of Parkinson’s. But PET scanning isn’t commonly used to evaluate Parkinson’s. That’s because it’s very expensive, not available in many hospitals, and only used experimentally.
Recommended Reading: What Is The Difference Between Huntington’s Disease And Parkinson’s
Mri In Parkinson’s Testing
One of the more common tests done during a neurologic workup is an MRI scan and one may think that in the investigation of a disease that affects the brain such as Parkinsons, this imaging test would be a necessity. In the context of Parkinsons disease, however, an MRI is not particularly helpful. It looks at the structure of the brain which, for all intents and purposes, appears normal in this disease. An MRI may, however, be indicated when symptoms appear in younger people or if the clinical picture or the progression of symptoms is not typical for Parkinsons. In these situations, MRI can be used to rule out other disorders such as stroke, tumors, hydrocephalus , and Wilsons Disease .
What Causes Parkinson’s Disease
Parkinson’s disease is the result of the loss of the brain chemical dopamine. When nerve cells, called neurons, in an area of the brain that controls movement become impaired and/or die, the amount of dopamine they normally produce decreases. This loss of dopamine causes the movement problems seen in people with PD.
Don’t Miss: Is Restless Leg Syndrome Related To Parkinson’s Disease
Sidebar: Ninds Steps Up Pursuit Of Pd Biomarkers
In 2012, the NINDS dramatically accelerated efforts to identify biomarkers by establishing the Parkinsons Disease Biomarkers Program . This unprecedented program unites a range of stakeholders from basic and clinical researchers to healthcare professionals, the NINDS staff, information technology experts, and people living with PD and their families.
PDBP supports research and builds resources aimed at accelerating the discovery of biomarkers to ultimately slow the progression of PD. For example, the program has established a repository of biological specimens and a Data Management Resource system maintained by the NIH Center for Information Technology. The DMR allows researchers to access clinical, imaging, genetic, and biologic data, while a complementary PDBP-supported project develops statistical tools to analyze vast quantities of data so that patterns can be identified across these diverse sources of information.
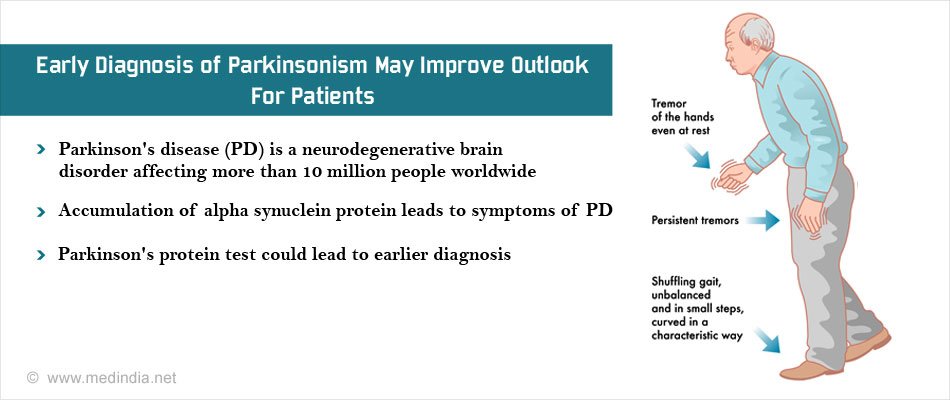
The Importance Of Early Diagnosis
Early detection and diagnosis is important because the treatments for PD are more effective in the early stages of the disease. In addition, physical therapy and exercise, which greatly improve symptoms and delay progression of the disease, are much easier to perform in the early stages.
Current diagnosis is made through the presence of motor symptoms however, researchers have found that by the time motor symptoms occur, over 60% of all dopamine neurons in the basal ganglia of the brain have been damaged. Non-motor symptoms become apparent in people with PD long before motor symptoms, including sleep disturbances and loss of the sense of smell.3
Active areas of research include looking for markers in the blood, urine, or cerebral spinal fluid that reliably detect PD, called biomarkers. In addition, brain imaging tests that have high sensitivity for detecting PD are also being actively researched.4
You May Like: When Was Parkinson’s Disease First Discovered
Definition And Differential Diagnosis
There are many manifestations of but the classical diagnostic symptoms are:
- slowness and poverty of movement
- stiffness
The physical signs of include:
- slowness of movement
- rest tremor.
At diagnosis, these signs are usually unilateral, but they become bilateral as the disease progresses. Later in the disease additional signs may be present including postural instability , cognitive impairment and orthostatic hypotension .
There is no single way to define Parkinsons disease or what is often called idiopathic Parkinsons disease in order to differentiate it from other causes of parkinsonism, such as multiple system atrophy and progressive supranuclear palsy .
is traditionally defined, pathologically, by the finding of Lewy bodies and degeneration of catecholaminergic neurones at post-mortem. Using a pathological definition of PD is problematic for a number of reasons:
- A pathological diagnosis is not practical in life.
- Lewy body inclusions in catecholaminergic neurones are seen in individuals without clinical evidence of it is presumed that these are pre-clinical cases.
- Lewy bodies have not been found in otherwise typical individuals with with Parkin mutations, although such rare young-onset genetic cases of PD might be said not to have idiopathic PD.
In recent years, attempts to define genetically have become possible with the discovery of monogenic forms of the disease. However, such families account for a very small proportion of cases.
Common causes of tremor.
How It All Fits Together
Diagnosing Parkinsons disease can be tricky. The process relies heavily on your doctors judgment. In addition, the causes and risk factors of Parkinsons are not entirely clear yet, which contributes to the difficulty in diagnosing this condition.
However, there have been efforts to try and detect this disease earlier. For instance, clinicians have started focusing more on prodromal symptoms, which are early symptoms that appear before movement-related difficulties begin.
These symptoms include:
- Loss of smell, which can sometimes occur years before other symptoms
- Chronic constipation, without any other explanation
- Rapid eye movement behavior disorder, which causes sleep disturbances
Recommended Reading: What Are The End Stages Of Parkinson’s
Severe Headaches Are A Main Symptom Of Parkinson’s Disease
There are several common symptoms of Parkinson’s disease, though severe headaches are not one of them. PD is diagnosed when a person has one or more of the four most common motor symptoms of the disease that include resting tremor, slow movement , rigidity, and difficulty balancing when standing . There are other secondary motor and non-motor symptoms that also occur with PD. Symptoms may be experienced differently by each person and the progression of the disease is different for everyone as well. For example, some people may have tremor as a primary symptom, while another may not have tremors but may have postural instability.
What Tests Diagnose Parkinson’s Disease
There currently are no tests that can definitively diagnose Parkinsons Disease. A diagnosis is based on the clinical findings of your physician in combination with your report on the symptoms you are experiencing.
In situations where an older person presents with the typical features of Parkinsons and they are responsive to dopamine replacement therapy, there is unlikely to be any benefit to further investigation or imaging.
Read Also: Does Sugar Affect Parkinson’s
There Are : : : : : Stages Of Parkinson’s Disease
There are five stages of Parkinson’s disease, described with the most commonly used Hoehn and Yahr scale: – Stage one: Symptoms such as tremors or shaking on one side of the body- Stage two: Tremors or shaking one or both sides of the body possible imbalance- Stage three: Noticeable balance impairment and slowing of motion- Stage four: Severe symptoms, disability patient likely needs assistance- Stage five: Patient may be bedridden or wheelchair bound needs constant care Another scale that may be used to describe symptoms of Parkinson’s disease is called the Movement Disorders Society-Unified Parkinson’s Disease Rating Scale . It is a four-part scale that measures motor movement in PD: non-motor experiences of daily living, motor experiences of daily living, motor examination, and motor complications.
How Is Parkinsons Diagnosed
Doctors use your medical history and physical examination to diagnose Parkinson’s disease . No blood test, brain scan or other test can be used to make a definitive diagnosis of PD.
Researchers believe that in most people, Parkinson’s is caused by a combination of environmental and genetic factors. Certain environmental exposures, such as pesticides and head injury, are associated with an increased risk of PD. Still, most people have no clear exposure that doctors can point to as a straightforward cause. The same goes for genetics. Certain genetic mutations are linked to an increased risk of PD. But in the vast majority of people, Parkinsons is not directly related to a single genetic mutation. Learning more about the genetics of Parkinsons is one of our best chances to understand more about the disease and discover how to slow or stop its progression.
Aging is the greatest risk factor for Parkinsons, and the average age at diagnosis is 60. Still, some people get PD at 40 or younger.
Men are diagnosed with Parkinsons at a higher rate than women and whites more than other races. Researchers are studying these disparities to understand more about the disease and health care access and to improve inclusivity across care and research.
Aging is the greatest risk factor for Parkinsons, and the average age at diagnosis is 60. Still, some people get PD at 40 or younger.
The Michael J. Fox Foundation has made finding a test for Parkinsons disease one of our top priorities.
Also Check: Is There A Test To See If You Have Parkinson’s
Molecular Imaging In Parkinson’s Disease
The diagnosis of PD relies on the clinical manifestation of cardinal motor symptoms, bradykinesia, and tremor at rest or rigidity . A positive response to dopaminergic drugs is supportive of the diagnosis. Single photon emission computed tomography or PET ligands that are specific for dopamine transporters indirectly enable the quantification of the deficit of dopaminergic nigrostriatal projections and can provide further support of diagnosis . Deficiencies of monoamine synthesis can be measured with dihydroxyphenylalanine which is a substrate for the enzyme aromatic amino acid decarboxylase in all monoaminergic neurons including noradrenergic neurons .
The role of deficits of noradrenaline in motor and non-motor symptoms is not clear and research on the noradrenergic system in PD patients has been hindered by lack of specific methods to visualize the noradrenergic neurons and projections in vivo. We have recently carried out PET studies to investigate the role of noradrenaline in non-motor symptoms in PD patients and these studies will form the basis of discussions in the paragraphs below.
Paul Johns BSc BM MSc FRCPath, in, 2014
What Does The Body’s Nervous System Control
The body’s central nervous system controls the five senses. The CNS is made up of your brain and spinal cord. The brain is what interprets our external environment, houses our thoughts and ideas, and controls our body movements. It acts like a central computer for our five senses, interpreting information from our eyes , ears , nose , tongue , and skin , as well as other sensations from internal organs such as the stomach. The spinal cord is the connection from the body to the brain, transmitting the signals our body receives to the brain, which then interprets them to make sense of our world. When the spinal cord is injured, this interrupts that communication.
You May Like: What Mattress Is Best For Parkinson Patients
People Who Already Have Pd: Should I Get Tested And What Do I Do With The Results
Up until recently, even people with PD with a very extensive family history of PD would not necessarily receive genetic testing because there were no clear uses for the results. There has been research directed at figuring out whether PD caused by or associated with certain mutations have particular clinical characteristics . However, there remains so much variability in clinical characteristics even among people with the same PD mutation, that there are still no clear practical implications in knowing whether a PD patient harbors a particular mutation. There is also, so far, no difference in treatment or management of PD whether or not the patient harbors one of the known mutations. That may change however, with the advent of clinical trials that target particular mutations.
There are two genes that have received particular attention recently because medications are being developed that target those with mutations of these genes.
GBAis a gene that increases the risk of developing PD. The gene encodes for the GBA enzyme, a protein used by the body to break down cellular products. Having two abnormal GBA genes causes Gauchers disease, which is characterized by the buildup of these cellular products resulting in fatigue, bone pain, easy bleeding and an enlarged spleen and liver. When a person inherits only one abnormal gene, he or she does not develop Gauchers disease, but does incur a small increased risk of PD. Most people with one mutated GBA gene do not develop PD.
