Risk Factors For Parkinson’s Disease
While the exact causes arent fully understood, researchers have identified characteristics that increase a persons risk of developing Parkinsons, including gender, age, race, and genetic factors. However, it is worth noting that the vast majority of cases of PD are considered idiopathic Parkinsons disease. Idiopathic means a condition that arises spontaneously or for which the cause is currently unknown. Major advances in research and science are continuing to reveal more underlying causes for PD.1,2
Characteristics Of The Study Population
After exclusion of individuals with missing data or outliers, 503,497 participants were available for the present analyses. Among these participants, 603 had an incident PD event. Analyses of the associations of CVD risk factors with PD were restricted to the 480,950 participants with no prior history of CVD and included 521 PD cases . The mean duration of follow-up was 9 years in all participants.
Overall, 59.2% of participants were women, 56.0% lived in rural regions, 57.3% had an income less than or equal to 19,999 yuan, and 50.8% had a primary school education or lower. Mean age of PD cases was older than that of the general population , and cases had a lower level of education . Likewise, a higher proportion of PD cases were agricultural workers or were retired compared with the general population .
Most participants were never regular drinkers or occasional drinkers . However, PD cases reported lower mean levels of physical activity than all participants . While 61.2% of men were current smokers, only 5% of women smoked, hence, analyses of smoking were restricted to men. At baseline 5.9% of all participants had diabetes, 32% were overweight or obese , and 33.5% had hypertension.
Sidebar: Ninds Steps Up Pursuit Of Pd Biomarkers
In 2012, the NINDS dramatically accelerated efforts to identify biomarkers by establishing the Parkinsons Disease Biomarkers Program . This unprecedented program unites a range of stakeholders from basic and clinical researchers to healthcare professionals, the NINDS staff, information technology experts, and people living with PD and their families.
PDBP supports research and builds resources aimed at accelerating the discovery of biomarkers to ultimately slow the progression of PD. For example, the program has established a repository of biological specimens and a Data Management Resource system maintained by the NIH Center for Information Technology. The DMR allows researchers to access clinical, imaging, genetic, and biologic data, while a complementary PDBP-supported project develops statistical tools to analyze vast quantities of data so that patterns can be identified across these diverse sources of information.
Don’t Miss: Parkinson’s And Lower Back Pain
Lewy Bodies And Alpha
In addition to the dopamine deficiency and neuronal loss, PD is also associated with a buildup of intracellular inclusions inside the neurons, called Lewy bodies. Studies have shown that the Lewy bodies are made mainly of a protein called alpha-synuclein.
They are not seen in brain imaging studies but have been detected in research studies that examine the brains of people who had PD and donated their own brains to science for the purpose of research. There is no known treatment or method of removing the Lewy bodies at this time.
In PD, Lewy bodies are found in the substantia nigra as well as other areas, including the amygdala and locus coeruleus , the raphe nucleus , and the olfactory nerve . The functions controlled by these regions can be impaired in PD, although the symptoms arent as noticeable as the tremors and muscle stiffness.
Lewy bodies are also present in the brains of people who have Alzheimers disease and other types of dementia, and they are considered a sign of neurodegeneration.
Dont Miss: Is Parkinsons Disease Considered A Disability
Intestinal Bacteria May Be An Important Piece In The Jigsaw Puzzle Of Multiple Sclerosis
Genome Medicine
Multiple sclerosis patients do not have the same bacteria in their intestines as healthy people. There are also differences in the composition and function of the bacteria in the intestines of multiple sclerosis patients, depending on whether their illness is active, and whether they are in treatment. This is the result of a major study of intestinal bacteria in multiple sclerosis patients and healthy control subjects, which was recently published in the journal Genome Medicine.
“Some groups of bacteria occur more frequently in people with multiple sclerosis and other bacteria groups are more frequent in people without multiple sclerosis. We also see that undergoing treatment for multiple sclerosis seems to be linked to a change in the composition of bacteria compared with patients who are not undergoing treatment,” says Professor Finn Sellebjerg, clinical professor at Rigshospitalet and University of Copenhagen, who is one of the researchers behind the study.
The study includes 148 Danish multiple sclerosis patients and just as many healthy control subjects, who gave blood and fecal samples at the start of the study and again two years later. Using genetic analyses, the researchers could identify which bacteria were in the intestines, and the effects of these bacteria.
“We can see that some of the changes in multiple sclerosis patients are also linked to the occurrence of inflammatory reactions in the body,” says Sellebjerg.
Also Check: Why Does Parkinson’s Cause Constipation
What Can I Expect If I Have This Condition
Parkinsons disease is a degenerative condition, meaning the effects on your brain get worse over time. However, this condition usually takes time to get worse. Most people have a normal life span with this condition.
You’ll need little to no help in the earlier stages and can keep living independently. As the effects worsen, youll need medication to limit how the symptoms affect you. Most medications, especially levodopa, are moderately or even very effective once your provider finds the minimum dose you need to treat your symptoms.
Most of the effects and symptoms are manageable with treatment, but the treatments become less effective and more complicated over time. Living independently will also become more and more difficult as the disease worsens.
How long does Parkinsons disease last?
Parkinsons disease isnt curable, which means its a permanent, life-long condition.
Whats the outlook for Parkinsons disease?
Parkinson’s disease isn’t fatal, but the symptoms and effects are often contributing factors to death. The average life expectancy for Parkinson’s disease in 1967 was a little under 10 years. Since then, the average life expectancy has increased by about 55%, rising to more than 14.5 years. That, combined with the fact that Parkinson’s diagnosis is much more likely after age 60, means this condition doesn’t often affect your life expectancy by more than a few years .
Living Well With Parkinson’s
While medication and DBS surgery are the most effective treatments for PD, individuals often choose to delay these treatments because of their adverse side effects. Until a therapy is developed that can halt the progression of PD, there is a significant need for strategies that provide symptom relief without causing negative side effects.
Diet, Exercise, and Stress Reduction
Findings from several studies suggest that exercise has the potential to provide relief from certain PD symptoms. Anecdotally, people with Parkinsons disease who exercise typically do better. However, many questions remain. Among them is whether exercise provides a conditioning effect by strengthening muscles and improving flexibility or whether it has a direct effect on the brain.
In an NINDS-funded trial comparing the benefits of tai chi, resistance training, and stretching, tai chi was found to reduce balance impairments in people with mild-to-moderate PD. People in the tai chi group also experienced significantly fewer falls and greater improvements in their functional capacity.
Technologies that Improve Quality of Life
Recommended Reading: How Do Doctors Test For Parkinson’s Disease
What Tests Will Be Done To Diagnose This Condition
When healthcare providers suspect Parkinsons disease or need to rule out other conditions, various imaging and diagnostic tests are possible. These include:
New lab tests are possible
Researchers have found possible ways to test for possible indicators or Parkinsons disease. Both of these new tests involve the alpha-synuclein protein but test for it in new, unusual ways. While these tests cant tell you what conditions you have because of misfolded alpha-synuclein proteins, that information can still help your provider make a diagnosis.
The two tests use the following methods.
- Spinal tap. One of these tests looks for misfolded alpha-synuclein proteins in cerebrospinal fluid, which is the fluid that surrounds your brain and spinal cord. This test involves a spinal tap , where a healthcare provider inserts a needle into your spinal canal to collect some cerebrospinal fluid for testing.
- Skin biopsy. Another possible test involves a biopsy of surface nerve tissue. A biopsy includes collecting a small sample of your skin, including the nerves in the skin. The samples come from a spot on your back and two spots on your leg. Analyzing the samples can help determine if your alpha-synuclein has a certain kind of malfunction that could increase the risk of developing Parkinsons disease.
Genetic And Environmental Interactions
Although several genetic mutations have been identified to be associated with a higher risk of developing Parkinson’s disease most people do not have these genetic variations.
On the other hand, even though pesticides and head traumas are associated with PD, most people do not have any obvious exposure to these environmental factors.
Parkinson’s is caused by a combination of genes, environmental and lifestyle influences. The interaction of all three components determines if someone will develop Parkinson’s. Parkinsons-specific research is critical to better understanding how these components interact to cause PD and how to prevent it.
Page reviewed by Dr. Lauren Fanty, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
You May Like: How Is Parkinson’s Detected
What Is Parkinsons Disease
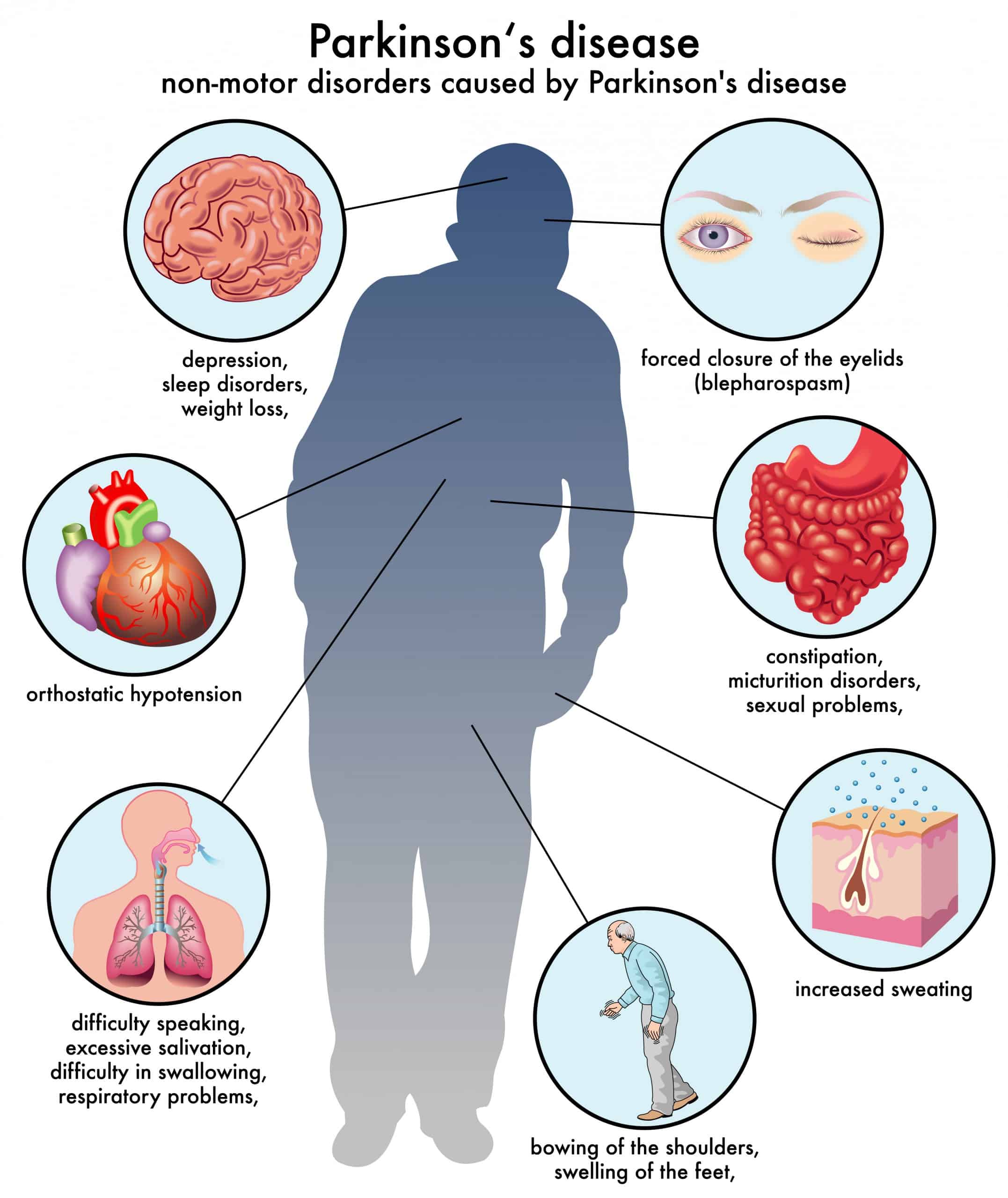
Parkinsons disease is a condition where a part of your brain deteriorates, causing more severe symptoms over time. While this condition is best known for how it affects muscle control, balance and movement, it can also cause a wide range of other effects on your senses, thinking ability, mental health and more.
Impact On Families And Carers
Informal carers spendmany hours dailyproviding care for people living with PD.This can be overwhelming. Physical, emotional and financial pressures can cause great stress to families and carers, and support is required from the health, social, financial and legal systems. Useful support resources from other conditions can be drawn upon, such as WHOs iSupport programme for dementia.
Don’t Miss: Best Physical Therapy Exercises For Parkinson’s Disease
How To Prevent Parkinsons Disease
Diet and exercise may play key roles
Parkinson’s disease results from the death of dopamine-producing nerve cells within an area of the brain called the substantia nigra.
Since dopamine regulates movement, depletion of it results in motor symptoms like shaking, stiffness, and walking problems. Non-motor symptoms, like depression, sleep problems, and loss of smell, also commonly occur.
While there is no definitive way yet to prevent Parkinson’s disease, eating a “brain-healthy” diet and incorporating physical activity into your daily routine might help reduce the risk or delay symptom onset. This article reviews the potential roles of diet and exercise in PD prevention.
Verywell / Jessica Olah
What Raises Someones Risk For Parkinsons
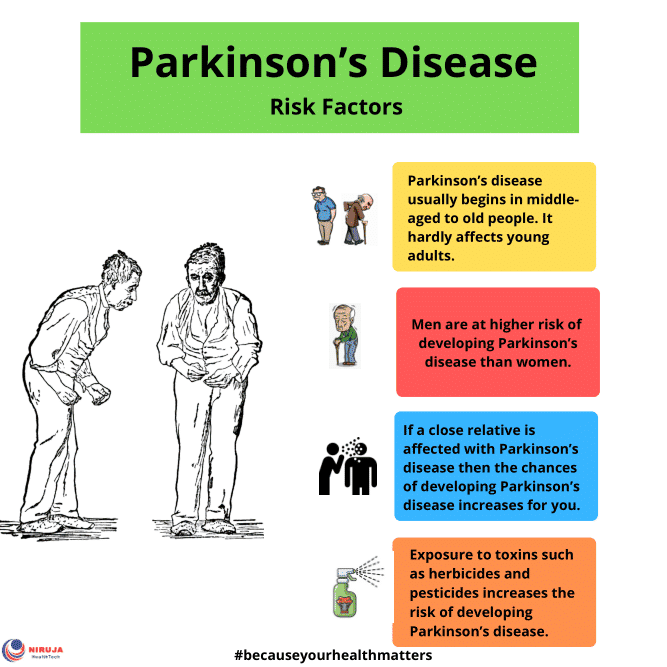
Its a complex picture, but you may be more likely to get Parkinsons based on:
Age. Since it mostly affects people 60 and older, your risk goes up as the years go by.
Family history. If your parent, brother, or sister has it, youre a little more likely to get it.
Job. Some types of work, like farming or factory jobs, can cause you to have contact with chemicals linked to Parkinsons.
Race. It shows up more often in white people than other groups.
Serious head injury. If you hit your head hard enough to lose consciousness or forget things as a result of it, you may be more likely to get Parkinsons later in life.
Gender. Men get it more than women. Doctors arent sure why.
Where you live. People in rural areas seem to get it more often, which may be tied to chemicals used in farming.
You May Like: What Is The Best Mucuna Pruriens For Parkinson’s
Neuropathology Of Parkinsons Disease
Macroscopically, the brain in idiopathic PD is often unremarkable with mild atrophy of the frontal cortex and ventricular dilation in some cases. The main distinctive morphological change in the PD brain is observed in transverse sections of the brainstem, where almost all cases present with loss of the darkly pigmented area in the substantia nigra pars compacta and locus coeruleus. This pigmentation loss directly correlates with the death of dopaminergic neuromelanin-containing neurons in the SNpc and noradrenergic neurons in the locus coeruleus . Cell death in the SNpc is mostly restricted to a specific group of neuromelanin-containing dopaminergic neurons, namely the A9 neurons, while other neuronal and glial cell types are largely spared .
Coronal section at the level of the substantia nigra pars compacta in a control and a PD brain stained by hematoxylin and eosin. In both sections, the dark brown cells are the neuromelanin-containing dopaminergic neurons.
You May Like: Ending Parkinsons Disease A Prescription For Action
Statins And Parkinsons Disease
In October 2016, a study abstract was presented at the American Neurological Association Conference that negated presumed beliefs about Parkinsons disease and statin use. The senior author, Dr. Xuemei Huang, MD, PhD, vice chair for research at Penn State College of Medicine, Hershey, had done multiple studies looking at the relationship between statin use and Parkinsons risk.1 Statins were thought be protective against neurodegenerative disease, but the study of 20,000 patients did not endorse this assumption. MarketScan Commercial Claims and Encounter databases from 2008 to 2012 were searched for patients between age 40 and 65 who were identified as having PD on diagnosis codes, anti-Parkinsons medication use, or having Deep Brain Stimulation surgery. These patients were then cross-referenced with cholesterol lowering medication use in the hopes to find evidence that supported prior smaller studies showing a protective effect. However, researchers found a statistically significant higher prevalence of Parkinsons disease after adjusting for confounders and comorbidities. To see if this was true for other neurodegenerative disease, data on Alzheimers patients was also pooled but this did not show any significant association.
Don’t Miss: How To Treat Hallucinations In Parkinson Disease
When Should I See My Healthcare Provider Or When Should I Seek Care
You should see your healthcare provider as recommended, or if you notice changes in your symptoms or the effectiveness of your medication. Adjustments to medications and dosages can make a huge difference in how Parkinsons affects your life.
When should I go to ER?
Your healthcare provider can give you guidance and information on signs or symptoms that mean you should go to the hospital or seek medical care. In general, you should seek care if you fall, especially when you lose consciousness or might have an injury to your head, neck, chest, back or abdomen.
How Soon After Treatment Will I Feel Better And How Long Will It Take To Recover
The time it takes to recover and see the effects of Parkinson’s disease treatments depends strongly on the type of treatments, the severity of the condition and other factors. Your healthcare provider is the best person to offer more information about what you can expect from treatment. The information they give you can consider any unique factors that might affect what you experience.
Read Also: Does Parkinson’s Make You Sleep A Lot
Can Parkinsons Disease Be Cured
No, Parkinsons disease is not curable. However, it is treatable, and many treatments are highly effective. It might also be possible to delay the progress and more severe symptoms of the disease.
A note from Cleveland Clinic
Parkinsons disease is a very common condition, and it is more likely to happen to people as they get older. While Parkinsons isnt curable, there are many different ways to treat this condition. They include several different classes of medications, surgery to implant brain-stimulation devices and more. Thanks to advances in treatment and care, many can live for years or even decades with this condition and can adapt to or receive treatment for the effects and symptoms.
Dont Miss: World Parkinsons Day 2022 Theme
How Does This Condition Affect My Body
Parkinsons disease causes a specific area of your brain, the basal ganglia, to deteriorate. As this area deteriorates, you lose the abilities those areas once controlled. Researchers have uncovered that Parkinsons disease causes a major shift in your brain chemistry.
Under normal circumstances, your brain uses chemicals known as neurotransmitters to control how your brain cells communicate with each other. When you have Parkinsons disease, you dont have enough dopamine, one of the most important neurotransmitters.
When your brain sends activation signals that tell your muscles to move, it fine-tunes your movements using cells that require dopamine. Thats why lack of dopamine causes the slowed movements and tremors symptoms of Parkinson’s disease.
As Parkinson’s disease progresses, the symptoms expand and intensify. Later stages of the disease often affect how your brain functions, causing dementia-like symptoms and depression.
Read Also: What Age Do You Get Parkinson’s
What Is The Family’s Experience With Parkinson’s Disease
Most Parkinson’s cases have no connection to a genetic cause, but scientists have found that some gene mutations can heighten an individual’s risk. Researchers believe that a better understanding of these genes may improve ways of identifying and treating the illness.
According to the National Institute of Neurological Disorders and Stroke, an estimated 15%-25% of Parkinson’s patients have a family history of Parkinson’s. Michael J. Fox Foundation for Parkinson’s Research estimates that about 10 percent of cases are linked with a genetic cause.
“Parkinson’s doesn’t stand out as a hereditary disease over and above any other chronic diseases that people deal with,” says Rebecca Gilbert, MD, PhD, chief scientific officer for the American Parkinson Disease Association in New York City. However, if you are a parent suffering from Parkinson’s disease you may be at four times the risk than those in the general population.
However, the risk of developing Parkinson’s disease is low. According to Michael J., Parkinson’s affects about 1 percent of people over 60. According to Dr. Gilbert, that figure rises to around 4% for people who are affected by the disease, as well as those who had a parent or grandparent with it. It is important to remember that just because your gene has been linked with Parkinson’s disease does not guarantee you will develop the illness.
