Freezing Of Gait & Interventions For Freezing Triggers Tips For People With Parkinson’s
Miriam “Mia” Boelen, PT, specialized in the treatment of those with PD from 1990 until her retirement in 2019. In this 27-minute video she demonstrates a 4-step method of specific maneuvers to break a freezing of gait episode. She also discusses common triggers and situational freezing, like crowded areas with tips for overcoming freezing in every case.
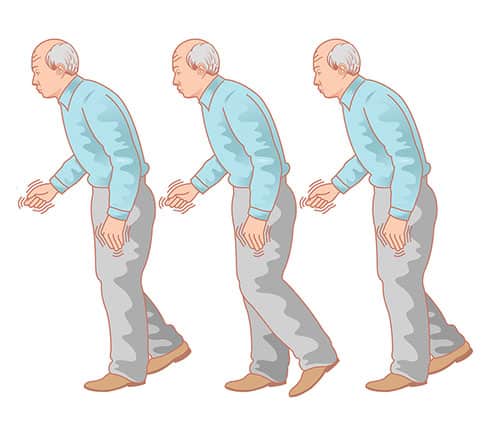
Types Of Secondary Movement Symptoms
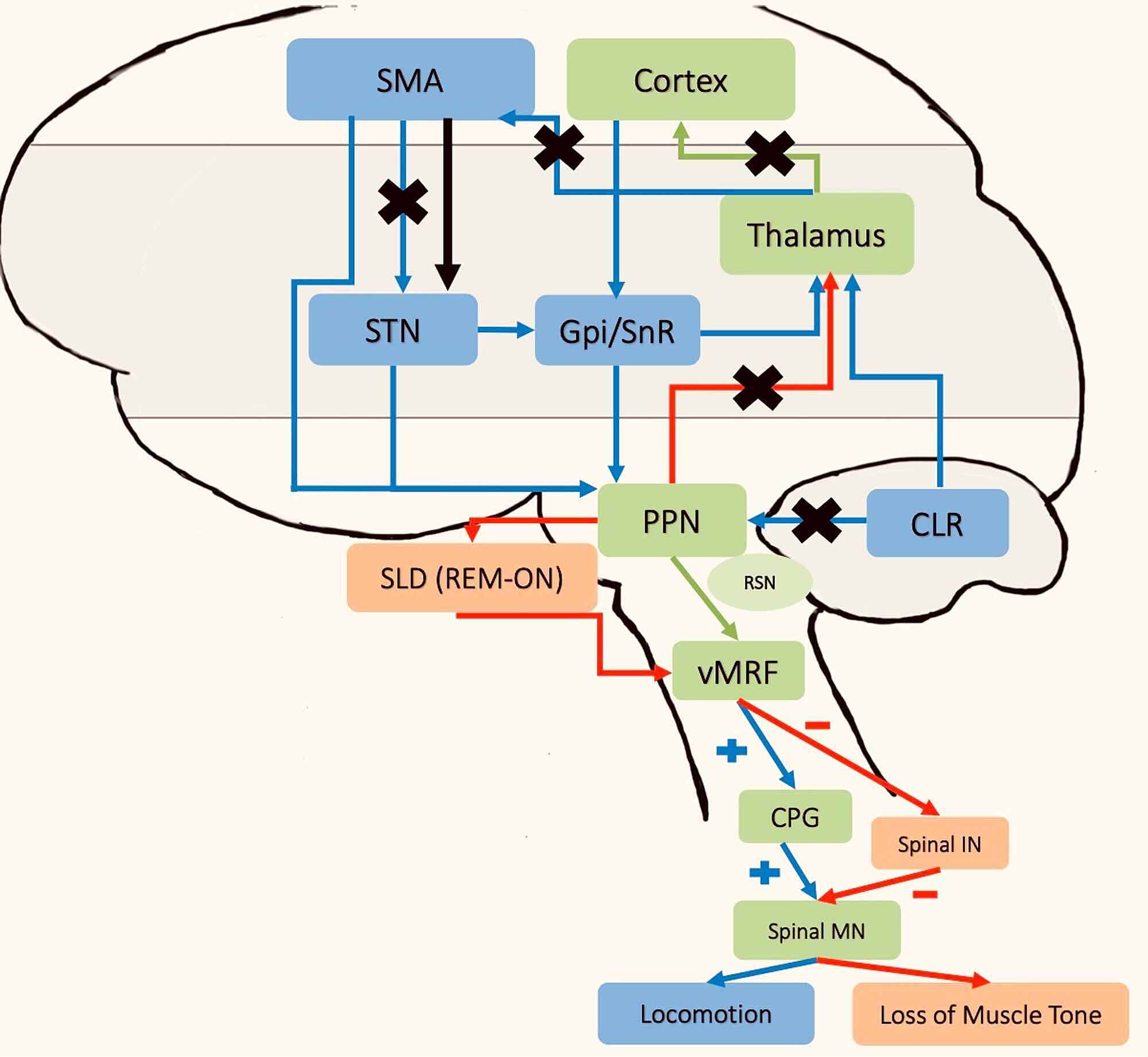
Imaging The Neural Underpinnings Of Freezing Of Gait In Parkinsons Disease
Review of recent imaging studies on Parkinsonian freezing of gait.
-
Virtual reality studies report functional decoupling of cortico-striatal circuits.
-
Motor imagery studies reveal increased recruitment of parieto-occipital regions.
-
fNIRS studies converge on reporting higher activity within prefrontal regions.
-
Imaging findings support pathophysiological models of freezing of gait.
Recommended Reading: Parkinson Association Of The Carolinas
Emergencies And Complications Of Device
Device-aided therapies include deep-brain stimulation, levodopa-carbidopa intestinal gel, and apomorphine subcutaneous injections and infusion. These are indicated to treat response fluctuations, such as recurrent disabling offs and dyskinesias refractory to standard therapy. Deep-brain stimulation is also used for drug-refractory tremor. Emergencies and complications related to device-aided therapies are not uncommon, and require prompt medical attention since they are generally associated with significant aggravation of Parkinsons disease symptoms .
An algorithm approach for DBS efficacy loss. DBS, deep-brain stimulation LD, levodopa.
Strategies To Combat Freezing In Parkinsons Patients
Freezing is when an individual suddenly feels like theyre glued to the ground. Parkinsons disease patients often experience freezing during the late stages of the disease. It can occur while the person is in motion or after theyve been stationary and then attempt to move. Its associated with complicated movements like dodging obstacles or getting up from a chair.
The loss of automatic motor skills affects ones sense of control and even their safety, as about 38 percent of Parkinsons patients fall each year. Tracking when your struggles occur can help you to manage them, allowing you to challenge how frequently freezing occurs.
Recommended Reading: What Age Is Parkinson’s Diagnosed
What Can You Do About Freezing
Many people have established their own ways of managing this symptom, as highlighted by one Parkinsons UK forum user:
My hubby walks backwards whilst holding my hands, I walk forwards and. now this is the best bit. I call one leg Tina and the other leg Turner. Off we go saying, Tina, Turner and repeat this until we reach our destination! We are usually in hysterics by the time we get to what ever room we are going to. But it does work!
Counting, chanting or singing in this way can help people to take that first step these are known as temporal cues as they tell people when to move. Imagining something to step over, or placing tape on the ground where freezing usually happens, can also help people to get moving again. These are spatial cues that inform people where to step.
How Do These Findings Fit Within Existing Models Of Freezing Of Gait
It is important to consider how some models of freezing of gait describe a downstream effect, without addressing the upstream cause. This might be why other models are not able to explain how anxiety or other processes might overload the basal ganglia, leading to increased freezing of gait. For example, the threshold model predicts that a motor deficit can accumulate to the point that reaches a threshold and freezing occurs . This model does not identify a root cause of the initial motor deficit. According to the current results, anxiety might be the key factor that initiates the motor deficit in the first place, and thus this model would be incomplete without the upstream cause having been identified. Similarly, the decoupling model does not identify the initial upstream event that leads to decoupling between preprogrammed and intended motor responses . Thus, in both cases identifying the upstream cause can elucidate why freezing of gait is the resultant behaviour.
Read Also: Parkinson’s Symptom Tracker App
Ten Tips To Put The Freeze On Freezing
While these methods can be helpful to get out of a freeze that is already underway, physical therapy techniques that incorporate these types of cueing strategies are utilized to reduce freezing of gait overall. Rhythmic auditory cueing is one such technique which utilizes rhythm and music to improve gait in PD and other neurologic diseases.
What Can Trigger A Freezing Episode
Freezing episodes can happen at any time but tend to happen more often when a person with Parkinsons is in transition. This can include starting to move transitioning from standing to walking or transitioning within a space, like walking through doorways, turning a corner, turning around or stepping from one type of surface to another. Freezing can increase in stressful situations or can be triggered by attempted multitasking.
Also Check: Best Balance Exercises For Parkinson’s Disease
So What Can You Do To Manage Freezing
- If you find yourself getting stuck in particular places, try changing the layout of your living space. Freezing can occur because you have to pivot around furniture.
- Exploring rhythm helps you to maintain momentum where you previously got stuck. Some Parkinsons patients explore strategies like dancing, counting, marching, and shifting their weight from side to side.
Thinking outside of the box can assist you in unfreezing yourself. Dad finds that his posture can affect whether or not hes able to unfreeze himself: When I freeze, I stand up straight. If I move away from gravity, I can unfreeze. But if Im hunching over, gravity pulls me toward the floor and it takes longer to get out of the freeze. And once I move my left foot forward, I can unfreeze. Freezings scary. Thats why a lot of Parkinsons patients fall.
Current Approaches And Hurdles In Parkinsons Disease Freezing Of Gait
In this 52-minute talk Lan Luo, MD, from the Parkinsons Disease and Movement Disorders Center at BIDMC explains freezing of gait , including how FOG manifests, FOG triggers, ‘on,’ vs. ‘off’ FOG, the brain pathways that are implicated in FOG, who gets FOG, several available treatments, and how to avoid falls.
Also Check: Is Parkinson’s A Form Of Cancer
Illustrative Case Of Acute Psychosis
An 80-year-old woman with Parkinsons disease was brought by her caregiver to the hospital emergency room because of marked agitation and paranoid ideation. She had physically attacked a staff member at the nursing home where she had been recently placed. One year earlier she developed visual hallucinations, initially well controlled with quetiapine . In the last 6 months she had developed frequent delusions with loss of insight. On admission to the Neurology ward she was taking 300mg per day of levodopa and quetiapine . Her cognitive state was normal. Other medical conditions known to cause acute psychosis were ruled out. Several treatment changes were tried. First, levodopa dose was halved without any significant motor worsening or improvement in hallucinations or delusions. In consequence, quetiapine was switched to clozapine , prompting improvement in psychiatric symptoms. In the end, levodopa was raised back to 300mg a day and clozapine was maintained. A few months later she had developed cognitive decline and rivastigmine was added.
-
Learning points: Psychosis exacerbation after nursing home placement loss of insight and delusions as severity markers before adding antipsychotic therapy for psychosis consider dopaminergic drug reduction, especially in advanced disease stages after acute episode resolution check cognitive status.
Freezing Of Gait In Parkinson’s Disease
This short webpage explains what freezing of gait is, why it occurs, and treatment. It also offers 10 tips to prevent freezing or get ‘unstuck.’ Finally, there is a discussion of walkers that can prevent injury due to falls when freezing episodes are severe and the future of treatments for freezing of gait.
Also Check: Best Place For Parkinson’s Treatment
Freezing Or Sweating Falls When Walking With Parkinson’s Disease
In this 1-hour webinar Fay B. Horak, PhD, PT, shares ways to improve brain function to minimize freezing and falls with Parkinson’s Disease. Viewers will understand how the brain controls walking and balance, discover what types of balance and gait impairments in Parkinsons disease result in freezing and falls and explore what can be done to minimize freezing and falls.
To Prevent Falls Exercise
Exercise is the only intervention that significantly reduces a persons risk of falling, among older people without PD as well as people with Parkinsons. Research is beginning to show how exercise changes the brain for the better and can help people with PD gain back some of their automatic balance reflex.
In a study, Dr. Horak and her team asked participants with PD to stand on a quickly moving treadmill, until they began walking. Participants initially took too-small steps, but with one hour of practicing, they improved, taking bigger steps to stay balanced while walking.
Many kinds of exercise can improve a persons balance. Consider trying:
- Tai Chi: a moving meditation where movements involve shifting the bodys center of mass back and forth over the feet. Studies found fewer falls among people with PD who practiced Tai Chi three times a week.
- Dance: to dance tango, a person has to walk backward and sideways, take big steps and both follow and lead good ways for people with PD to practice balance control.
- Boxing: the rapid arm movements provide good balance training.
- Agility boot camp: completing different tasks in a series of stations can improve balance.
Tip: People with PD may have other medical issues that affect their ability to exercise, such as arthritis or neuropathy. Work with a physical therapist to find an exercise that suits your needs.
Read Also: Can Parkinson’s Cause Droopy Eyelids
Balance And The Brain
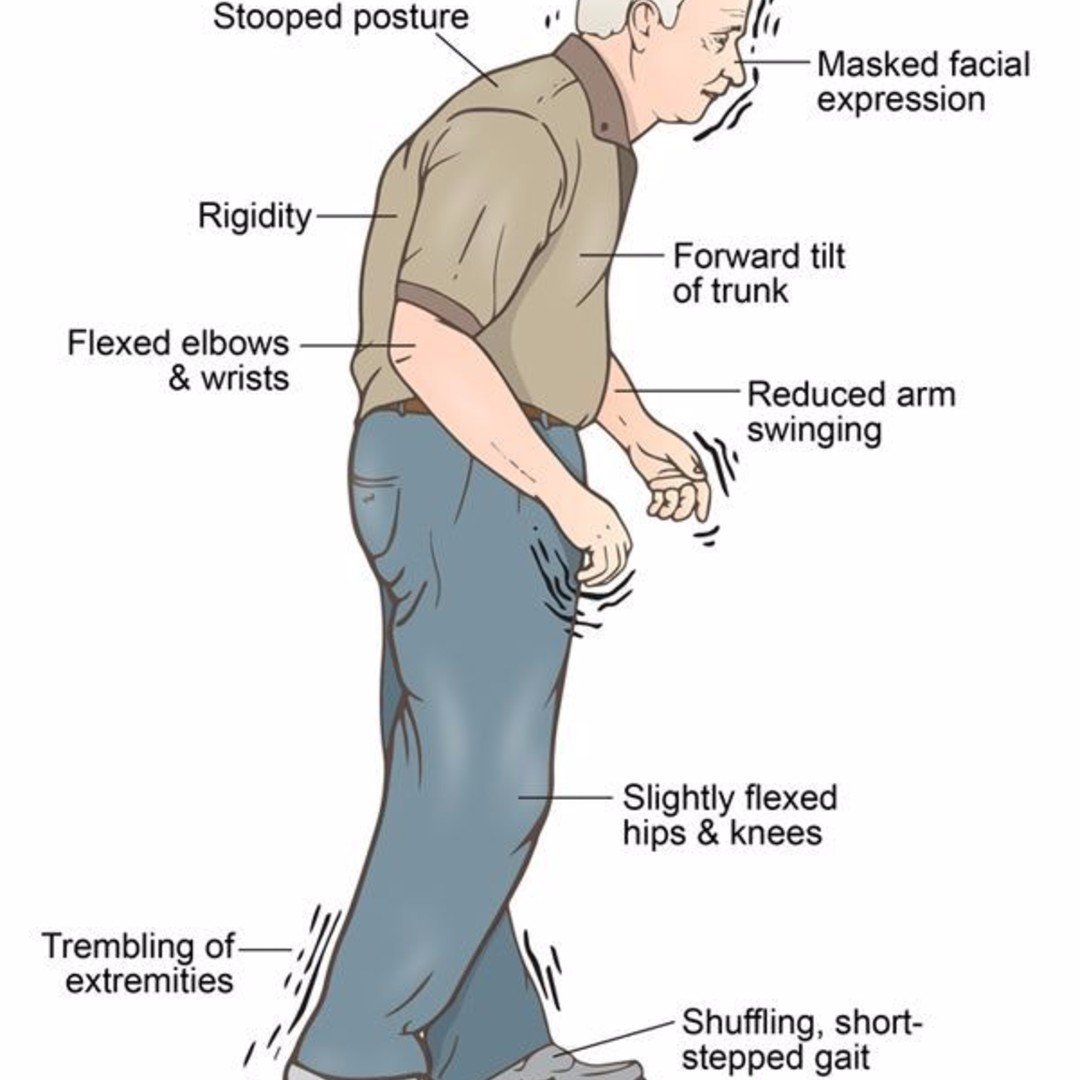
Difficulties with balance and walking are linked to the brain changes that take place with PD. For people who dont have PD, balance is automatic, a reflex. But Parkinsons affects the basal ganglia . To compensate, the brain assigns another brain area an area used for thinking to take over. The thinking part of the brain, mainly the frontal cortex, cant control balance automatically. The result: for many people with PD, balance becomes less automatic.
This means that when people experience freezing and fall, they cant adjust their balance automatically. Taking small steps to try and regain balance can make things worse, because it involves shifting weight with each step. The brain changes from PD inhibit their ability to take a big step to catch their balance and avoid a fall. For some, the drug levodopa can help prevent freezing, but does not improve balance.
A person whose balance is less automatic must pay more attention while walking. For everyone, walking slows down when were talking and thinking slows down when were walking. This is called the dual-task cost and its higher in people with PD. That tells us that people with PD are using more attention and more cognitive control for balance and gait.
What Freezing Is Like For My Dad
Like many Parkinsons patients, my dad notices that he usually only freezes when hes not on his medication. It usually happens while hes moving through doors: When you pivot youre worried about losing your balance. Thats why we shuffle our feet and take baby steps initially. Once Im moving Im fine, he says.
Since hes worried about maintaining balance while navigating, its possible that theres a connection between fear and freezing. Continuous motion seems to bypass the risk of freezing, while shifting motion types can present challenges.
Recommended Reading: Is Parkinson’s A Movement Disorder
What Are The Five Stages Of Parkinson’s Disease
Researchers may disagree on the number of stages of Parkinsons disease . However, they all agree the disease is a progressive disease with symptoms that usually occur in one stage and may overlap or occur in another stage. The stage increase in number value for all stage naming systems reflects the increasing severity of the disease. The five stages used by the Parkinsons Foundation are:
- Stage 1: mild symptoms do not interfere with daily activities and occur on one side of the body.
- Stage 2: Symptoms worsen with walking problems and both sides of the body are affected.
- Stage 3: Main symptoms worsen with loss of balance and slowness of movement.
- Stage 4: Severity of symptoms require help usually a person cannot live alone.
- Stage 5: Caregiver needed for all activities a patient may not be able to stand or walk and maybe bedridden and may also experience hallucinations and delusions.
A neurologist who specializes in movement disorders will be able to make the most accurate diagnosis. An initial assessment is made based on medical history, a neurological exam, and the symptoms present. For the medical history, it is important to know whether other family members have Parkinson’s disease, what types of medication have been or are being taken, and whether there was exposure to toxins or repeated head trauma previously. A neurological exam may include an evaluation of coordination, walking, and fine motor tasks involving the hands.
How Would We Confirm An Effective Treatment
Confirming any effective treatment would also require an accurate and objective measurement of FOG . This is surprisingly difficult as FOG is most commonly experienced unpredictably at home where gait is more automatic or natural. In the clinic, gait becomes more goal directed and it can become difficult to trigger episodes . Two questionnaires for the assessment of FOG have previously been developed, namely the Freezing of Gait Questionnaire and the New Freezing of Gait Questionnaire . Whilst these were both validated in sizeable cohorts against subjective carer and clinician ratings, there was no gold standard measure or definition of FOG at the time the instruments were constructed . Indeed, subsequent work has demonstrated that self-perceived ratings of FOG severity using the FOG-Q and NFOG-Q do not correlate well with the actual number or duration of objective freezing episodes when scored from video recordings of Timed Up and Go walking tasks . Furthermore, it is only recently that the authors of the NFOG-Q examined its test-retest reliability, as well as its ability to detect minimal change. This work found that the NFOG-Q is not sufficiently reliable or responsive to detect small effect sizes .
Table 1. Assessment methods in use for FOG measurement, and their advantages and disadvantages.
You May Like: What Are The Signs Symptoms Of Parkinson’s Disease
Does Anxiety Cause Freezing Of Gait In Parkinson’s Disease
-
Affiliations Sun Life Financial Movement Disorders Research and Rehabilitation Centre, Wilfrid Laurier University, Waterloo, Ontario, Canada, Cognitive Neuroscience, Department of Psychology, University of Waterloo, Waterloo, Ontario, Canada
-
Affiliation Cognitive Neuroscience, Department of Psychology, University of Waterloo, Waterloo, Ontario, Canada
-
Affiliation Sun Life Financial Movement Disorders Research and Rehabilitation Centre, Wilfrid Laurier University, Waterloo, Ontario, Canada
Ways To Manage Freezing
From treatments such as physiotherapy, to cueing techniques you can do yourself, there are different things that can help you manage freezing.
Speak to your GP, specialist or Parkinsons nurse about the best treatment for your freezing. They can also refer you for therapy that may help. Treatments include:
Read Also: Does Richard Blumenthal Have Parkinson’s
Medicine: Freezing: An Attack On Parkinson’s Disease
PARKINSON’S disease presents a distressing set of symptoms. The patient suffers from shaking palsy. His gait becomes abnormal, and eventually he cannot walk. Finally there is a boardlike rigidity to his entire body that renders him immobile.
Medical researchers have not yet found the cause of the disease, but surgeons have succeeded in treating its symptoms. New York’s Dr. Irving S. Cooper uses supercold liquid nitrogen to destroy an area of the brain that is responsible for the patient’s characteristic tremors.
After the patient’s head is shaved, he is given a local anesthetic at a…
Key Measures For The Prevention Of Complications
-
Parkinsons disease nurse specialists should support patients and caregivers by clarifying concerns and implementing a treatment plan.
-
Patients, caregivers and medical staff are responsible for bringing all the medication updated, and paying attention to medication timings.
-
If at all possible, avoid changing abruptly or changing more than one antiparkinsonian medication at a time.
-
Patients and caregivers should be provided with a list of drugs capable of worsening parkinsonism.
-
Patients taking dopamine agonists should be informed about sleep attacks and risk of impulse-control disorders before starting treatment and regularly during follow-up.
-
Periodically, at least annually, review falls, sleepiness, cognition, autonomic disturbances and psychiatric symptoms.
-
Disease rehabilitative therapy should be proposed to minimise complications such as falls and swallowing problems.
-
In case of elective admission, it is important to plan in advance how to make medication changes. If oral medication intake is limited, consider transdermal agonists, enteral administration of usual medication, and levodopa-carbidopa intestinal gel infusion.
Read Also: Does Parkinson’s Cause Anger
