Talking To Your Doctor
How do you know if your neck pain is potentially related to early signs of Parkinsons disease?
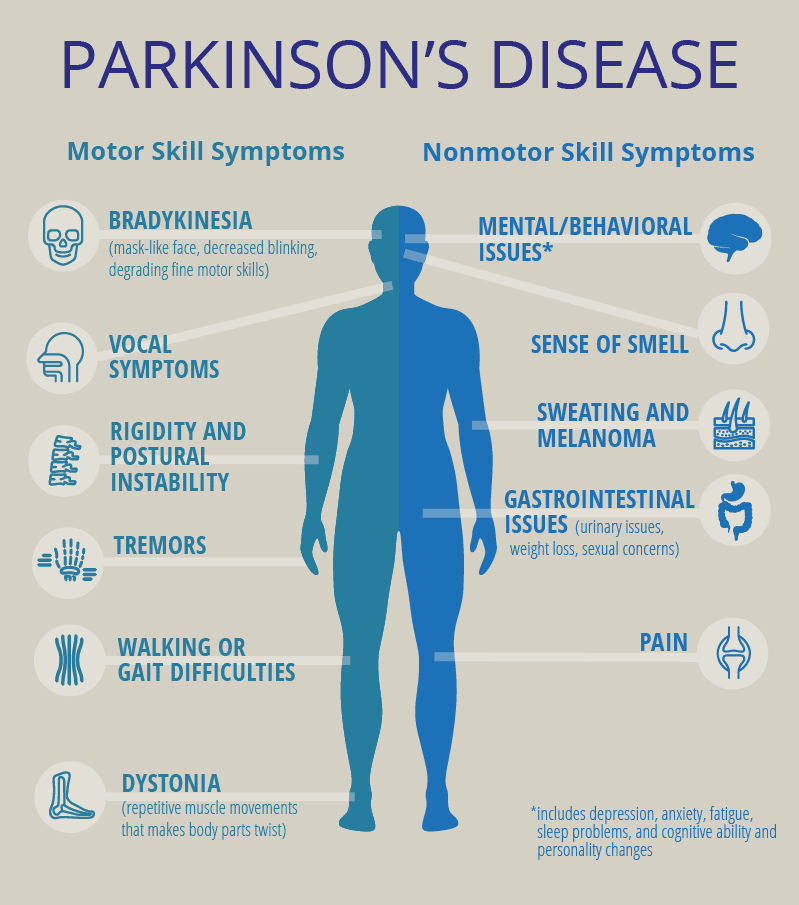
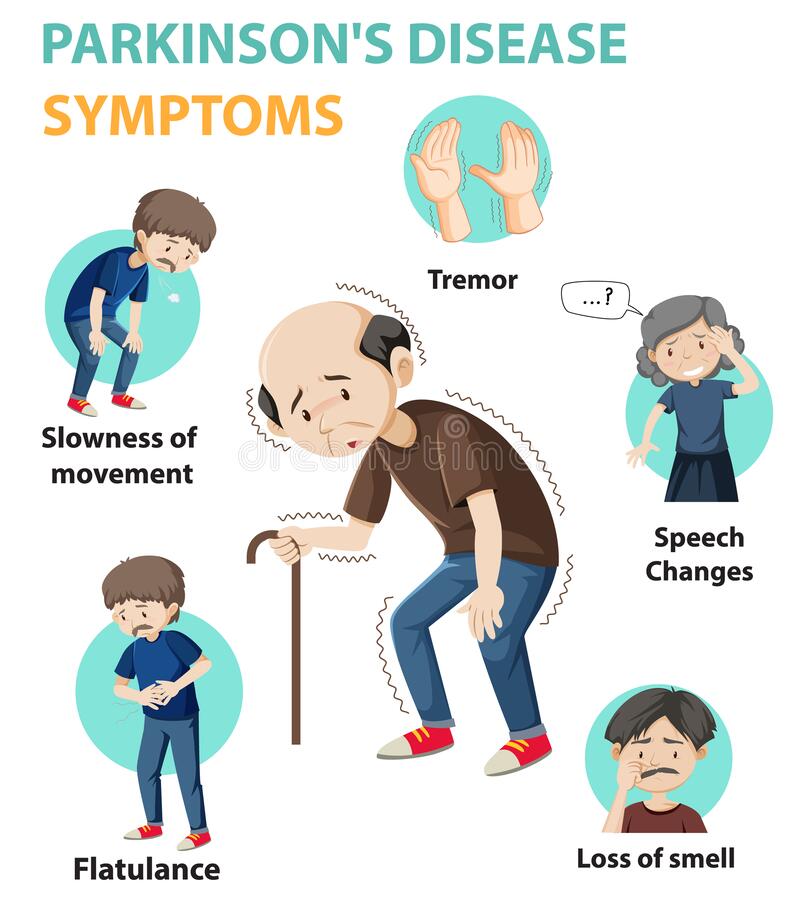
You cant know for sure, but you and your doctor can explore the issue. If your neck pain is accompanied by any of the other early warning signs of the condition, such as stiff shoulder, small handwriting, hand tremor, reduced arm swing, and shuffling gait, then it becomes more likely that you may have Parkinsons disease.
If you have one or more of these symptoms, you should speak to a neurologist about them. Early identification may allow doctors to slow the progression of the disease, if, in fact, you do have the disease.
When Should I Call The Doctor
You should call your healthcare provider if you experience:
- Frequent or severe muscle twitches that affect your ability to work, sleep or enjoy life.
- Severe headaches.
A Note from Cleveland Clinic
Everyone has occasional involuntary muscle twitches, or myoclonus. But for some people, muscle spasms become disruptive and even dangerous. Your healthcare provider can determine the cause of myoclonus. Medications can reduce the severity and frequency of myoclonic twitches and jerks.
Last reviewed by a Cleveland Clinic medical professional on 09/28/2020.
References
All Up A Multidisciplinary Team Approach For Pain Management May Be Necessary In Addition To Your Movement Disorder Specialist Providers May Include Physical Or Occupational Therapists Psychiatrists And Even Pain Management Experts Each Of These Practitioners Targets A Different Aspect Of The Pain
Exercise to Relieve your Pain
Many different types of exercise can be beneficial for people with Parkinsons disease , including non-contact boxing, tai chi, dancing and cycling, as some examples. If you have limited mobility, you can try chair yoga or other seated exercises. Whichever exercise you choose, make sure it is something safe and enjoyable so that you can stick with it.
Its important to pace yourself and know your personal limitations. If during or after exercise you experience extreme pain you should look at modifying your routine and choose a less intensive exercise. Even the simplest exercise, including walking your dog or just puttering around the house or garden, can help alleviate symptoms of pain.
- Cycling
If you need help or advise consult with a physical or occupational therapist to help design a personalised program for you. Learn more about exercise and Parkinsons.
Non-pharmacological pain treatments
Complementary therapies are treatments used alongside conventional medicine. They take a more holistic approach than conventional medicine, aiming to treat the whole person including mind, body and spirit, rather than just the symptoms. These include massage therapy, mindfulness and meditation techniques, acupuncture, and heat or cold application. These may be used on their own or in combination with medication.
Anti Inflammatories
Read Also: Parkinsons Education For Nurses
Don’t Miss: How To Beat Parkinson’s
Pain Sites And Assessments
All patients were asked to indicate the distribution of pain sites, duration of pain, and rate average pain intensity over the past 3 months on an 11-point numeric rating scale , with 0 indicating the absence of pain and ten indicating the most intense pain imaginable. The patients reported NRS scores in both the ON and OFF states of motor function on the same day. NRS scores were then transformed into WHO severity stages of mild , moderate , and severe , respectively . MSP responsiveness to Levodopa was defined as a 30% reduction in NRS scores from baseline, 2 h after taking the medication . Data regarding multiple types of pain were also recorded. The ID-pain scale detected central parkinsonian pain.
Memory Or Thinking Problems
Having issues with thinking and processing things could mean your disease is progressing. Parkinsons is more than a movement disorder. The disease has a cognitive part as well, which means it can cause changes in the way your brain works.
During the final stage of the disease, some people may develop dementia or have hallucinations. However, hallucinations can also be a side effect of certain medications.
If you or your loved ones notice that youre getting unusually forgetful or easily confused, it might be a sign of advanced-stage Parkinsons.
You May Like: Why Is Parkinson’s Medication Time Specific
Prevalence Of Pain In Pd Patients According To Pain Characteristics
Depending on the population assessed and the criteria employed to define the presence of pain, its prevalence ranges from 40% to 83% of PD patients.5, 6, 7, 8, 9 In a casecontrol study, pain was present in at least one quarter of PD patients before any treatment6 and in almost 40% of patients early in the course of the disease.10 In a recent cohort study, pain has been considered a premotor symptom.11 Pain occurrence further increases with disease progression, particularly associated with the development of therapydependent motor fluctuations.9
A second study, performed in French outpatients, distinguished between nonPD and PDrelated pain, including pain syndromes directly or indirectly caused by PD.8 In this series, 60% of patients suffered from chronic pain, which was related to the disease in 60% and unrelated in 40%. Finally, in the Norwegian study, 83% of patients had PDrelated pain, 70% with musculoskeletal pain, 40% with dystonic pain, 20% with radicular or peripheral neuropathic pain, and 10% with central neuropathic pain.5
What Can I Expect If I Have This Condition
Parkinsons disease is a degenerative condition, meaning the effects on your brain get worse over time. However, this condition usually takes time to get worse. Most people have a normal life span with this condition.
You’ll need little to no help in the earlier stages and can keep living independently. As the effects worsen, youll need medication to limit how the symptoms affect you. Most medications, especially levodopa, are moderately or even very effective once your provider finds the minimum dose you need to treat your symptoms.
Most of the effects and symptoms are manageable with treatment, but the treatments become less effective and more complicated over time. Living independently will also become more and more difficult as the disease worsens.
How long does Parkinsons disease last?
Parkinsons disease isnt curable, which means its a permanent, life-long condition.
Whats the outlook for Parkinsons disease?
Parkinson’s disease isn’t fatal, but the symptoms and effects are often contributing factors to death. The average life expectancy for Parkinson’s disease in 1967 was a little under 10 years. Since then, the average life expectancy has increased by about 55%, rising to more than 14.5 years. That, combined with the fact that Parkinson’s diagnosis is much more likely after age 60, means this condition doesn’t often affect your life expectancy by more than a few years .
Recommended Reading: Parkinson’s Disease Prognosis With Treatment
S Of The Body Affected By Dystonia
People with Parkinson’s can experience this disease-related cramping or clenching differently. Areas impacted include:
- Arms, hands, legs and feet: Involuntary movements, spasms or twisting and “curling”
- Neck: May twist uncomfortably, causing the head to be pulled down or to the side. This is called cervical dystonia or spasmodic torticollis
- Muscles around the eyes: May squeeze involuntarily, leading to a person to blink too much or to have difficulty opening the eyes also called blepharospasm.
- Vocal cords and swallowing muscles: May cause a person’s voice to sound softened, hoarse or breathy
- Jaw: May open or close forcefully or there may be grimacing of the face
- Abdominal wall: May cause sustained contractions, involuntary, writhing movements of the abdominal wall, or grimacing of the face
Lifestyle Changes For Muscle Atrophy
Along with medication making some positive changes in the lifestyle can be of great help in coping up with the physical limitations in movement. Instead of blaming god and others for the problem, it is better to adapt with the condition and look for ways to improve. One very common problem, which almost all the people suffering from Parkinsons disease face is getting up and sit in the chair. However, having a lifted chair or customizable chair can be of great help to cope with this physical limitation similarly, making a use of physical support tool while walking can help in maintaining balance and avoiding any fall or injury.
Also Read:
Recommended Reading: Zhittya Genesis Medicine Parkinson’s Disease
How Do Methamphetamines Cause Parkinsons Disease
Parkinsons disease is caused by the death of a region of the nervous system known as the substantia nigra. This part of the brain both produces and releases the neurotransmitter dopamine. Since dopamine is so closely tied with the primary functions of the nervous system as they relate to coordination and movement, a permanent dopamine deficiency can lead to the same progressive and chronic symptoms that characterize Parkinsons disease.
Researchers have long known from non-human animal studies that methamphetamine induces cell death within the substantia nigra, though only recently have studies been able to verify the correlation to any large degree. One of the animal studies conducted in the mid-1990s indicated a total reduction in dopamine within the substantia nigra in laboratory mice of 40-45 percent within one week of exposure to methamphetamine.
A similar study on mice demonstrated that just three dose-proportioned methamphetamine injections set at three-hour intervals produced a fairly immediate reduction in dopaminergic cells of between 20 and 25 percent.
Observable significant increases in microglial cells, designed to protect the nervous system, are seen within the substantia nigra within hours after methamphetamine exposure, indicating some level of neurotoxicity.
Pain Stress And Biomarkers Of Stress
Stress and pain are often closely linked. Each has an impact on the other, creating a vicious cycle that sets the stage for chronic pain and chronic stress. Therefore, stress management should be a component in pain therapy.
The Merriam-Webster Encyclopedia® defines the term stress as a physical, chemical, or emotional factor that causes bodily or mental tension and may be a factor in disease causation. The result of stress can be explained as physical or mental tension resulting from factors that tend to alter an existing equilibrium.
You May Like: How Long Parkinson Patients Live
Don’t Miss: How Fast Does Parkinson’s Disease Progress
Specific Pain Syndromes In Pd
Orthostatic hypotension can cause headache or neck pain . If necessary, antihypertensive co-medication should be adjusted in accordance with recently given recommendations . Additional measures are physical exercises, fluid intake, wearing of compression stockings class two, and administration of substances such as midodrine, fludrocortisone or, in severe cases, L-threo-3,4-dihydroxyphenylserine . Camptocormia is often accompanied with pain. Prior to therapy the cause has to be differentiated . In addition to the use of pain killers, the focus is on physiotherapy. There is no specific pain medication recommended currently.
Migraine is reported less often in PD, and often associated with depression and sleep disturbances . Therefore the therapy has to focus on the comorbidities as well. The usual medication for migraine can be used, but due to an increased risk for orthostatic hypotension in PD, caution should be exercised with beta blockers .
Is Parkinsons Disease Inherited
Scientists have discovered gene mutations that are associated with Parkinsons disease.
There is some belief that some cases of early-onset Parkinsons disease disease starting before age 50 may be inherited. Scientists identified a gene mutation in people with Parkinsons disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinsons disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinsons disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinsons disease.
Scientists think that about 10% to 15% of persons with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
Dont Miss: How Does Parkinsons Disease Spread From Person To Person
You May Like: Diet Parkinson’s Disease Treatment
General Aspects Of Pain Treatment In Pd
Despite the high prevalence of pain in PD, literature data suggest that only up to a maximum of 50% of PD patients receive at least some type of pain therapy .
Still, the fundament of pain therapy should be an optimized dopaminergic treatment which can improve pain related to insufficient dopaminergic supply such as akinesia and/or rigidity , pain due to dopaminergic over-supply such as dyskinesia and/or dystonia , or central pain that is dopamine-sensitive . This concept was reported to be effective in about 30% of PD patients . A standardized levodopa test can be helpful to decide whether the pain is dopaminergic responsive or not, but any result of this short-term effect must always be interpreted with caution so that the long-term assessment of pain under dopaminergic therapy over several weeks remains essential .
A systematic review and meta-analysis including databases from January 2014 until February 2018 investigated the efficacy of a variety of novel, complimentary, and conventional treatments for pain in PD and found the greatest reduction in pain for safinamide, followed by cannabinoids and opioids, multidisciplinary team care, COMT-inhibitors, and electrical and Chinese therapies, while the weakest effects were obtained for dopaminergic agonists and miscellaneous therapies . Table 1 gives an overview of larger randomized controlled trials of antiparkinsonian drugs and opioids assessing the effect on pain in PD patients.
Table 1
Fig.1
What Treatment Is Available
For treatment to be effective, it is essential to understand the trigger or cause of the dystonia. Certain medications may be effective for some people but not for others. Some work by interfering with neurotransmitters in the brain and disrupting the messages they send to muscles. Others work by relaxing the muscles to reduce shaking and improve muscle control.
Depending on the cause and severity of your dystonia, your doctor may suggest the following strategies:
Remember that not all of these strategies will work for everyone so it is important to communicate well with your doctor so that, together, you can find the best solution for you.
Keeping a diary: If the dystonia is levodopa-related, it is a good idea to keep a motor diary to record when dystonic spasms occur and how they relate to the timing of medications. This information can help your doctor adjust dosage and/or timings of medication to better manage your dystonia. For more information, see Keeping a diary.
Read Also: Does Parkinson’s Affect Your Heart
Increased Urination Urgency And Frequency
Bladder problems are a common occurrence in people with Parkinsons, occurring in 30-40 percent of people with the disease. The most common urinary symptom is a frequent and urgent need to urinate even when the bladder is empty, as well as trouble delaying urination.
Trouble emptying the bladder is a less common feature of Parkinsons urinary dysfunction. It may be caused by difficulty in relaxing the urethral sphincter muscles that allow the bladder to empty.
How Is Pain Treated For People With Parkinsons
No matter the cause, pain is often complex. When a person with Parkinsons experiences intense pain, especially in combination with other symptoms of Parkinsons, managing it can be challenging. There are, however, several ways you can adjust your medication regimen, exercise schedule, and lifestyle to reduce your pain and improve your quality of life.
Medications
There are various kinds of medications used to treat pain, especially for people with Parkinsons. In a recent webinar, Dr. Janis Miyasaki described how physicians approach pharmacological treatment of pain for people with Parkinsons:
The principle is to start with what is called the pain ladder. You always start with the least intensive, least side effect-giving treatment.Janis Miyasaki, MD
Step one
The first step of the pain ladder is hot and cold treatments along with stretching and flexibility exercises. People who experience rigidity and stiffness can sometimes alleviate pain using heating pads to loosen their muscles, then improve mobility by stretching, then address any residual pain with ice packs.
Step two
Step three
Step four
Step five
Other medical interventions
Read Also: A Typical Parkinson’s Progression
Leg Pain And Parkinsons
Interestingly enough, one of my early symptoms of the disease was deep searing pain in my left leg, the type of pain my grandma had complained about many times. Initially this type of pain was worst in the morning as well as at night, making me think is was some sort of fasciitis. However not only did typical anti-inflammatories and muscle relaxants not alleviate my pain but pain worsened over time to a constant burning pain that felt as if someone was tearing the muscle and pouring hot oil on it. The pain was so excruciating it was permeating into all aspects of my life. I was constantly in need of deep tissue massage asking my husband to massage my legs just as my grandmother had asked of us time and time again. This helped only temporarily.
Which brings me to the four types of leg pain in PD.
You May Like: Movie Stars With Parkinsons Disease
Urinary Issues In Advanced Parkinsons Disease
Urinary dysfunction and symptoms in PD are most commonly caused by overactivity of the detrusor muscle, or the muscle of the bladder, which contracts excessively despite the fact that it is not filled with urine. This causes an increased urge to urinate and/or an increased frequency of urination, which can be especially prominent at night. In advanced PD, this could culminate in urinary incontinence, or involuntary release of urine. Mobility issues which make getting to the bathroom slower and more cumbersome, compound the problem.
Always remember that people with advanced PD may have other medical problems that affect their urination such as an enlarged prostate. Make sure to have a complete evaluation before assuming that the problem is only related to PD. It is also essential to keep in mind that if changes in urination occur suddenly, there could be a urinary tract infection present.
Once other medical issues and urinary tract infection are ruled out, there are a number of approaches to the issue of urinary incontinence in a person with advanced PD:
Unfortunately, for some, the above available options may not be sufficient to effectively treat urinary incontinence in advanced PD. If this is the reality, it becomes extremely important to keep the skin dry with frequent changes of incontinence products to prevent skin breakdown and the potential development of skin infection.
Also Check: Can Essential Tremor Become Parkinsons
Also Check: What Essential Oils Help Parkinson’s
