All Up A Multidisciplinary Team Approach For Pain Management May Be Necessary In Addition To Your Movement Disorder Specialist Providers May Include Physical Or Occupational Therapists Psychiatrists And Even Pain Management Experts Each Of These Practitioners Targets A Different Aspect Of The Pain

Exercise to Relieve your Pain
Many different types of exercise can be beneficial for people with Parkinson’s disease , including non-contact boxing, tai chi, dancing and cycling, as some examples. If you have limited mobility, you can try chair yoga or other seated exercises. Whichever exercise you choose, make sure it is something safe and enjoyable so that you can stick with it.
It’s important to pace yourself and know your personal limitations. If during or after exercise you experience extreme pain you should look at modifying your routine and choose a less intensive exercise. Even the simplest exercise, including walking your dog or just puttering around the house or garden, can help alleviate symptoms of pain.
- Cycling
If you need help or advise consult with a physical or occupational therapist to help design a personalised program for you. Learn more about exercise and Parkinson’s.
Non-pharmacological pain treatments
Complementary therapies are treatments used alongside conventional medicine. They take a more holistic approach than conventional medicine, aiming to treat the whole person including mind, body and spirit, rather than just the symptoms. These include massage therapy, mindfulness and meditation techniques, acupuncture, and heat or cold application. These may be used on their own or in combination with medication.
Anti Inflammatories
Since A Back Injury In 1985 John Has Experienced Multiple Types Of Pain Some Of Which Have Been Triggered By His Parkinson’s He Was Diagnosed With The Condition In 2016
I’ve been experiencing varying degrees of pain since injuring my back, which caused me to have lower-back pain, which continues to this day. Since then, I have also developed pain in other parts of my body due to Parkinson’s, including my hands, ribs, upper back and shoulder.
The pain in my ribs is deep, aching and constant, and I get internal tremors in this area. However, the pains in my legs are sharp, intermittent and become very rigid, especially in my calves.
When I walk, the pain can get so bad that I end up having to stop and rest. On really bad days, I use a wheelchair. When I’m in a lot of pain, it affects my Parkinson’s symptoms even more, and also my spatial awareness, that I tend to lose my balance and fall or freeze.
I was referred to a pain specialist…who enrolled me on an 8-week pain management course led by a Parkinson’s-trained physiotherapist. Now I do an hour of gentle movements and stretching every morning.
I can’t stand for long enough to wash and have a shave, or to wash the dishes, so I use a perching stool. I can no longer carry out my hobby of canoeing to the same degree. While I use to be able to do it all day, I’m now lucky if I can do it for an hour.
I was referred to a pain specialist, who prescribed me medication, and advised on workable changes to my lifestyle and diet. They also enrolled me on an 8-week pain management course led by a Parkinson’s-trained physiotherapist. Now I do an hour of gentle movements and stretching every morning.
Im In Pain But I Dont Want To Take Carbidopa/levodopa Yet Because My Doctor Says It Will Only Work For Five Years Any Advice
It is true that as time passes and your disease progresses, you will have to take higher doses to replace the dopamine your body can no longer produce. However, the rate of dopamine loss is different for everyone. What your doctor may be telling you is that after taking carbidopa/levodopa for some time, you may begin to experience side effects like dyskinesia. It is important to understand that while you may experience this unwanted side effect, for example, you still benefit from the carbidopa/levodopa. If you believe your pain is Parkinson’s-related, and you have already tried other medications and complementary therapies without relief, it is probably time to try carbidopa/levodopa.
Colm Was Diagnosed With Parkinson’s Around 3 Years Ago And Experiences 4 Different Types Of Pain Related To The Condition
The 4 different types of pain I experience all affect my muscles and joints. This includes sudden-onset joint pain – typically a frozen shoulder, or pain when I bend an elbow or knee. It usually lasts between 6-8 weeks and will usually go away for a week or 2, only to reappear in another joint. It greatly restricts my movement and its constant nature can be frustrating.
I also have issues with leg cramps and dystonia, which I frequently experience when waking in the morning, or when moving between different ground surfaces. The cramps are very severe with sudden onset, but slowly wear off after some minutes.
My Parkinson’s has worsened certain pre-existing conditions, including back problems, which were caused by a childhood injury. This has caused me painful episodes throughout my life, but my Parkinson’s seems to have exacerbated this to the point where I’m totally incapacitated with pain and stiffness.
As a carer, I have no option but to try and carry on with my normal duties…I find it helps to wake about 2 hours earlier than normal to take my medication.
I keep an armchair and some dressing aids in my bedroom, as a bout of very severe back pain makes getting in and out of bed or dressing myself difficult.
I also experience muscle stiffness and inflexibility, which cause me pain due to over-exertion. This happens if I don’t take regular breaks throughout the day. As a carer myself for 3 disabled family members, this can prove very difficult.
James* Was Diagnosed With Parkinson’s In 2011 His Pain Has Worsened As His Condition Has Progressed
When I was diagnosed with Parkinson’s, I initially felt little to no pain. It’s only now, in the advanced stages of the condition, that I’ve started feeling pain, coupled with the normal ageing process.
One of the worst pains I experience is dystonia and dyskinesia of the upper body, especially in my neck and head. It usually starts with a pulsing headache, followed by jerking of the muscles in my face, neck, upper torso and hands. It’s particularly severe in my arthritic finger and my neck. It can be severe to mild, often very distressing, and can last up to 2 hours.
I also have mild to moderate, uncontrollable movements – or swaying – associated with dyskinesia. It’s more prominent when I’m sitting down at a table or working on my laptop. Strangely, I feel this pain at its worst when I’m on the phone, or trying to explain something, or if I’m feeling over-excited or anxious – which is when I become severely dyskinetic. There’s now a dull, continuous pain in my neck, caused through the movement, which gets sharper during bouts of the symptom.
I also experience pain when standing, mostly during a ‘wearing off’ period. My knees pull towards each other and the pain is so severe that I can’t walk. Luckily it only lasts a minute or 2, but the pain can be distressing.
To ease the pain, I take paracetamol as and when, occasionally co-codamol, and very occasionally an anti-inflammatory, for the arthritis. I previously tried cannabis oil but it was of no benefit to me.
Negative Impact Of Severity Of Pain On Mood Social Life And General Activity In Parkinson’s Disease
This case control study designed for clinicians and rehabilitation specialists to effectively identify pain from the patient’s point of view determined that PD patients had significantly higher pain severity scores compared to controls. PD patients with depressive symptoms had significantly higher pain severity and pain interference scores than controls without depressive symptoms. PD patients reported greater scores on Global BPI pain interference and all components of the pain interference subscale. Therefore, PD and depression seem to be correlated with higher perceived pain, severity and interference. A report on this study, by Jose Marques Lopes, PhD., was published in Parkinson’s News Today, September 21, 2018.
Lower Back Pain That Gets Worse When You Lay Down Constant Pain On Lower Back On Side Of Spine
Pain In Lower Back Feels Like Stabbing Needles Lower Back Pain In Ramadan ? Can Parkinson S Disease Cause Lower Back Pain. Acute Lower Back Pain Elderly When Lower Back Pain Is Serious. Be Active Back Pain Relief Back Pain Remedies For Upper Pain. Effective Safe Relief For My Back Pain Exercise For Lower Back Pain While Sitting.
Sharp Pain In Lower Back Near Tailbone Yoga Mudra For Back Pain Relief. Stomach And Right Side Upper Back Pain Nausea Weakness Lower Back Left Leg Pain Dull Sharp Pain In Stomach Lower Back Pain And Lightheadedness. Back Pain In Right Upper Quadrant I M 20 And I Have Lower Back Pain.
Interested In Parkinsons Disease Research Sign Up For Our Forums And Join The Conversation
A total of 97 Parkinson’s patients at a mean age of 67.7 years, including 60 men, and 97 individuals used as controls at a mean age of 67.5 years, including six men, without the disorder or other neuromuscular diseases, filled out a questionnaire on the intensity of local lumbar back pain. The intensity of leg radicular pain — caused by inflammation and/or injury to a spinal nerve root – was quantified by the visual analogue scale — a continuous scale used to measure pain intensity.
In addition, the participants’ permanent functional disability was assessed via the Oswestry Low Back Pain Disability Questionnaire — a self-completed questionnaire that includes 10 different topics: intensity of pain, lifting, ability to care for oneself, ability to walk, ability to sit, sexual function, ability to stand, social life, sleep quality, and ability to travel.
Patients were further asked to describe the painful sensation they experience as pricking, tingling, burning, paresthesia — often described as feelings of pins and needles, or numbness — or other.
The team also assessed Parkinson’s duration, medications being used, severity of motor symptoms — as assessed by the Unified Parkinson’s disease rating scale part III — and the Hoehn and Yahr stage, which is a system used to assess symptom progression.
According to the ODI results, minimal disability was reported by 43.8% of Parkinson’s patients, moderate disability by 27.5%, severe disability by 22.5%, and “crippled” by 6.3%.
How To Sleep To Heal Lower Back Pain Can Parkinson S Disease Cause Lower Back Pain
Best Studies Comparing Nsaids To Conservative Treatment For Low Back Pain Low Back Pain Posture Physiopedia Do Prostrate Issues Cause Lower Back Pain. Can Contractions Cause Pain In Your Lower Back And Butt Lower Back Pain Arm Pain Sore Throat. Symptom Small Hard Lump Pain After Pressing On It Lower Back Swelling Bladder Irritation Pain On Left Lower Chest And Mid Back Worse With Cough.
Revisiting Pain In Pdthe 50 Shades Of Pain Experienced By Parkinsons Patients
Pain is a quality of life issue for people with Parkinson’s disease and can be under treated by doctors who may assume that is worsens as the disease progresses, although for some pain is an initial symptom of PD. This article helps focus your physician’s attention in the right direction to accurately diagnose your pain.
Pain Management In Patients With Parkinsons Disease: Challenges And Solutions
This review focuses on the diagnosis and management of Parkinson-related pain. It reviews the incidence and prevalence of PD, general pain and PD-related pain, the pathophysiological pathways of pain in PD, physiological pathways of pain relief, measurements of pain, clinical diagnosis of PD-related pain, and treatment strategies.
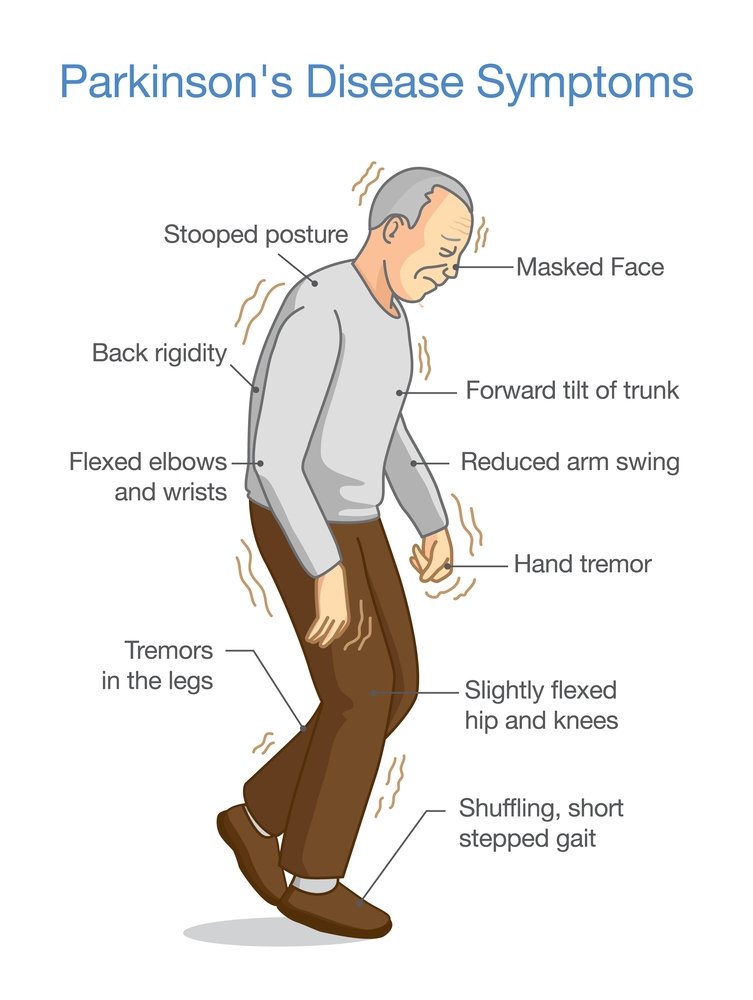
What Are The Different Types Of Pain Experienced By People With Parkinsons
Five main types of pain are common for people with Parkinson’s. Multiple types may be present simultaneously or occur at different points throughout a person’s path with Parkinson’s. Recognizing which kind of pain is present can help you optimize treatment, as can paying attention to what activities or times of day make your pain better or worse.
Musculoskeletal pain
Musculoskeletal pain that affects muscles, bones, tendons, ligaments, and/or nerves. The pain can be localized or generalized and can fade or intensify at different times. Existing musculoskeletal pain can be exacerbated by Parkinson’s.
Neuropathic pain
Rather than being caused by a physical injury, this type of pain is caused by damage to the somatosensory nervous system or a disease affecting the somatosensory nervous system, which responds to external stimuli like touch, temperature, and vibration. It tends to be fairly consistent throughout the day and is present no matter what activity you’re doing. Unlike the aching you may feel when you’re doing a strenuous physical activity, neuropathic pain feels more like a tingly, crawly, uncomfortable sensation.
Dystonic pain
Dystonia, the movement disorder in which involuntary muscle contractions cause repetitive or twisting motions, is often very painful. Many people with Parkinson’s experience dystonia as a motor symptom, whether it’s localized , in multiple nearby body parts , or all over .
Akathisia
Central pain
Q Are There Any Alternative Therapies That Are Effective For Pain In Pd

Dr. Fleisher: Although alternative therapies may be helpful, there is little evidence-based research to support their use. Certainly massage therapy, anecdotally, seems to be helpful for managing pain. Small studies suggest that acupuncture might improve sleep in patients with PD, but data on the effects on pain in PD is lacking. Larger, more well-controlled and reproducible studies of these therapies are needed.
Patients frequently ask about the effects of medical marijuana in managing PD, including pain symptoms. Several studies have looked at efficacy of marijuana in PD and have found that it probably is ineffective for most PD symptoms.11 However, we just don’t have enough evidence to know for sure. The most rigorous study of medical marijuana in PD showed a trend toward worsening tremor.11,12
For most people, stress and anxiety worsen tremor, and anything that relieves anxiety will improve tremor. Thus, modalities such as yoga, meditation, and mindfulness training will improve tremor. Similarly, medical marijuana may improve tremor in certain people by temporarily reducing anxiety and stress, but the evidence has not borne this out yet.
Q What Is The Pain Experience In Pd And Does It Differ Between Genders
Dr. Fleisher: As with almost everything else in PD, the pain experience is highly individualized, and no 2 people, regardless of gender, will have the same symptoms. Female gender appears to be an independent risk factor for chronic pain in PD, even though PD is more common in men than in women.2 Pain intensity also is higher in women than in men with PD.1
There is a lot of interesting research examining the contributions of hormones to the greater prevalence of PD in men or, conversely, the lower prevalence in women.3 Once we better understand the roles of sex hormones in the pathophysiology of PD, we may better understand whether hormones also play a role in the higher incidence of chronic pain in women with PD.
Sensory Acuity Kinesthesia And Dynamic Central Sensory Integration
Any type of physical activity optimally requires accurate sensation and perception of one’s own position and movement , and both PD and LBP associate with impaired kinesthesia. People with PD exhibit impaired tactile sensation and impaired kinesthesia to detect limb position during active motion as well as to detect passive limb and trunk rotation . People with LBP exhibit impaired two-point discrimination and can be unable to kinesthetically perceive their lumbar trunk based on body image traces . In contrast to the global somatosensory impairment exhibited by people with PD, the impaired tactile discrimination of people with LBP appears to be isolated to the area of the LBP . Impaired lumbosacral repositioning accuracy has also been reported for people with LBP . Further, similar to the impaired detection of trunk motion exhibited by people with PD, people with LBP exhibit increased thresholds for detecting passive trunk flexion and lateral bending . Thus, although the extent of impairment may differ between people with PD versus LBP, both health conditions associate with impaired tactile acuity and kinesthesia.
Q Are There Any Gender Disparities In The Treatment Of Pain In Pd
Dr. Fleisher: I don’t think there is any literature demonstrating gender disparities in pain treatment among patients with PD, but we do know that there are certainly gender disparities overall in the treatment of women with PD, so it would not be surprising to learn that women with PD-related pain are at a disadvantage and not getting the appropriate care that they need.
Innovative Treatment Modalities For Managing Pain In Parkinson’s
Botulinum toxin
Non-dopaminergic pharmacotherapy may benefit patients with PD-related pain. Botulinum toxin , both A and B derivatives, should be considered in patients who do not respond to dopaminergic treatment optimization.1,8 Botulinum toxin injection provides localized treatment by blocking the release of acetylcholine at the neuromuscular junction.4 Local injections of BTX type A or B can be effective for persistent dystonia-related pain and central pain, based on its neuromuscular action in movement disorders plus analgesic mechanism.
A randomized, double-blind, crossover, placebo-controlled trial concluded that BTX-A in patients with PD is safe and potentially useful in treating limb pain.29 The study was conducted in patients with PD over the age of 30 years with painful limbs not responding to the optimization of anti-Parkinsonian medications. Patients were randomized to receive BTX-A injection or placebo, followed by the other treatment per the crossover design. Depending on the location of pain, patients received up to 200 units in upper limbs or up to 300 units in lower limbs. Patients experienced a significant reduction in their self-reported numerical pain score 4 weeks after the BTX-A injection , but not with placebo . There was no difference between the change with BTX-A compared to placebo . This study demonstrated that targeted BTX-A injections are safe in patients with PD.
Cannabinoids
Investigation Of Back Pain In Patients With Parkinsons Disease
O. Yaremchuk, I. Yaremchuk
Session Time: 1:15pm-2:45pm
Location: Agora 3 West, Level 3
Objective: The aim of this study was to investigate prevalence and influence of different methods of treatment of back pain in patients with Parkinson’s disease in the Chernivtsi region of Ukraine.
Background: Pain is one of frequently observed non-motor symptoms in patients with PD. Chronic pain occurs in 30% to 85% of patients with PD, particularly in women, and is one of the strongest predictors of poor quality of life.
Method: We used clinical, epidemiological and statistical methods of research. These were examined 84 patients with PD who were treated in Department of Nervous Diseases, Chernivtsi Regional Psychiatric Hospital. They were clinical examination and interviewed by using specially designed questionnaires. The visual analog scale was used for pain severity.
References: A. D. Ha, J. Jankovic. Pain in Parkinson’s Disease. Movement Disorders, Vol. 27, No. 4, 2012. 485-491.
To cite this abstract in AMA style:
Mov Disord.
Pain Is An Unfortunately Common Problem In Parkinsons Disease
Of course, pain is common in the general population, especially among older people. A recent American study found that pain affected about twice as many people with Parkinson’s Disease than those of the same age and gender without PD. About 50% of Parkinson’s Disease patients in that study suffered from painful disorders. Men and women seem to be about equally affected. A very well described scenario is the patient who is followed for a painful frozen shoulder for a year or so before a tremor develops leading to a diagnosis of PD. Pain clearly plays a major role in quality of life. Everyone with chronic pain enjoys life less, leading to a vicious cycle in which pain causes depression or isolation which in turn leads to more pain.
Parkinson patients suffer from the same pain problems that other people have, often amplified by the motor dysfunction, but they also have additional pain problems which are unique to PD.
One recent review classified the types of pain Parkinson’s Disease patients have into: musculoskeletal, in which the pain results from problems with the muscles , bones or joints; dystonic, which is due to abnormal muscle contractions caused by the Parkinson’s Disease or the medications used to treat it; radicular pain, which is feels like the pain caused by pinched nerves; central pain, which is presumed due to abnormalities in the brain, and is a continuously present pain that cannot be explained otherwise; and discomfort related to an unpleasant urge to move.
Q What Is The Role Of Depression In The Pain Experience In Pd
Dr. Fleisher: Depression is one of the most overlooked symptoms of PD, and it can affect over 30% of people with the disease at some point in their illness.5 I think there is a misconception that depression results from an adjustment disorder following diagnosis. While that may be partially true, patients with PD have alterations in various neurotransmitters—including serotonin and norepinephrine in addition to dopamine—that predispose them to depression.6,7
Depression is the primary factor related to quality of life in PD and is an independent risk factor for medication nonadherence. A physician could prescribe the most comprehensive regimen to control Parkinson’s symptoms, including pain, but if depression symptoms are not being addressed simultaneously, the likelihood that that person is going to take that regimen is pretty minimal.
Given the link between depression and chronic pain, patients who are depressed should be screened for chronic pain and vice versa. In my practice, we screen every patient with the Unified Parkinson’s Disease rating scale , which has both a patient-reported subjective component that includes questions about depression, pain, and altered sensation, as well as an objective component that includes a physical examination and questions about potential medication adverse effects . The patient fills out the subjective component every single time they come to the office.
Pain Is A Common But Overlooked Problem In Parkinsons Disease
Pain is an often overlooked non-motor symptom of Parkinson’s disease . Studies show that between 40-80% of people with PD report pain, which is likely why it is often suggested as a topic for this blog.
One of the reasons why the topic of pain and PD is difficult to address is that it is sometimes tough to discern whether a particular pain is due to PD or not. Chronic pain is such a common symptom among the general population, and people with PD are not immune to common problems as well. However, there are aspects of PD that may exacerbate the pain experienced from a common problem. In addition, there are particular types of pain that may be unique to people with PD.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Opening The Medicine Box In The Mind: The Psychology Of Pain
In this 50-minute lecture, Beth Darnall, PhD explains how our experience of pain goes beyond the physical sensation of pain. It has emotional and psychological components that affect our ability to treat pain. She cites research to demonstrate that and shares 13 specific tips to reduce the experience of pain and increase treatment effectiveness. Audience questions follow the lecture.
Q Is There Anything Else You Would Like To Tell Our Readers
Dr. Fleisher:There are so many symptoms of PD that it can be easy to overlook pain symptoms if a patient doesn’t report them. Remember that pain may be a really prominent symptom for patients, but, given that we have only learned how pain is connected to PD in the past 20 years, patients may not be aware of the association and may not bring up pain symptoms with their neurologist.
Thus, the burden is on us to ask about pain, particularly if the patient is depressed. If a patient with PD has both pain and depression, both of those comorbidities should be targeted, because it can be hard to achieve successful outcomes for either pain or depression if one is treated without the other.
What Causes Pain In Cases Of Parkinsons Syndrome Sufferers
Parkinson’s Syndrome Sufferers may present with various combinations of back, buttock and leg pain, numbness and muscle weakness, Symptoms are often aggravated by an abnormal asymmetrical gait arising from loss of spatial awareness muscle spasm and loss of limb control. The back pain may arise from irritation within the disc wall but more commonly arises from the pinching of the trapped nerve in the exit doorway from the spinal column. The foramen may be distorted and the nerve is tethered by years of scarring reaction to repetitive bruising, can not evade the pinching by the bulging distorted disc wall or overriding facet joints . The disc may be degenerate and bulging and contribute to the irritation of the tethered nerve. When advanced the compression causes numbness and weakness to develop. The patchy weakness or spasm of the muscles controlling the spinal segments results in asymmetrical loss of control or stiffness of the disc levels and aggravation of the effects of the local pathology at each level and aggravation of symptoms arising at these levels.
Q Which Pharmacotherapies Are Best For Treating Pain In Pd
Dr. Fleisher: The first step is to make sure that Parkinson’s medications are optimized. For example, dystonic or musculoskeletal pain may be caused by Parkinson’s motor symptoms when dopamine levels are too low. If the patient is able to keep a pain diary, it may show a clear pattern of pain occurring the hour before each dose or before specific doses, suggesting the need to either increase the dosage preceding the pain episode, increase the frequency of medication dosing, or use adjunctive dopaminergic therapies to achieve more steady dopamine levels throughout the day.
In addition, optimal management of comorbidities that may contribute to pain is needed. The choice of pain medication depends on the pain type.
The first lines of treatment for musculoskeletal pain can be heat and cold packs and nonsteroidal anti-inflammatory drugs alone or in combination with acetaminophen.
For dystonic pain, adjustment of dopaminergic medications is particularly critical; however, if dystonia consistently occurs in 1 particular body part, botulinum toxin injections also can be helpful. The goal of botulinum toxin injection is to weaken the muscle enough to stop the abnormal contractions and twisting, but the patient may lose function in the body part as a result . Thus, patient counseling is important to manage expectations.
Lower Back Pain And Back Of The Neck Pain Are Most Common
Pain occurs for a number of reasons and it’s not always clear what the cause is, making it difficult to figure out how best to treat it. I believe that most common pain problems in Parkinson’s Disease are the same as in the general population, but amplified. Low back pain and back of the neck pain are probably the most common pain conditions in PD. The reason Parkinson’s Disease patients have so many problems with their low back and their neck is their posture. Parkinson’s Disease causes a stooped posture. Some of this happens with age anyway, particularly in women after menopause when their bones soften, but is always worse from the PD. All Parkinson’s Disease patients have some degree of stooped posture and many also tilt to one side. Because of the stooped posture, the muscles in the lower back have to pull much harder to keep the spine upright.
The Preponderance Of Injury In The Past Of People With Pd
Neck issues or damage can be caused by injuries, but the injury site doesn’t have to be local to the neck itself, since it is an integral part of the kinetic chain of the human body – problems anywhere else which affect posture can, in turn, profoundly affect how we tense our necks and cause strains on it by the way we are holding up the head. I’ve frequently asked people with Parkinson’s Disease to think carefully about any pains and injuries which they might have incurred either before or concurrent with their PD diagnosis. I’ve found that the overwhelming majority of us have suffered a prior accident or physical trauma. Injuries to jaw, neck, shoulders, back, hips, knees or feet predominate. All these severely affect posture and hence the kinetic chain and are liable to make our necks prone to permanent strains and stiffness. So in my view, even if chemical “cures” were invented tomorrow, people with PD would still present with the postural problems, still suffer from the old injuries which have been masked by the narratives of neurology, and would probably quickly decline into pain and problems again, unless these past injuries are properly attended to.
Active Research Into Several Aspects Of Parkinsons Pain

Researchers are working to better understand the mechanisms behind pain in Parkinson’s so that it can be more effectively addressed. They are looking for objective measurements, such as brain imaging, to diagnose and monitor pain, and to evaluate response to treatment. And, they’re investigating several drugs and deep brain stimulation for their potential benefits in treating Parkinson’s disease pain.
