Continuous Dopaminergic Stimulation Therapies
Deep brain stimulation
Cross-sectional studies have suggested a positive effect of subthalamic Deep Brain Stimulation on autonomous responses of PD subjects . In one of this analysis, including 14 patients, there was a mean general decrease on blood pressure in on and off stimulation status , but the baroreflex responses were preserved only when the stimulation was on, suggesting, therefore, a positive influence of the DBS in BP mediated by its influence on central autonomous nervous system pathways . In another study comparing subthalamic DBS with a pharmacotherapy-only group, no positive correlation was found between the on-stimulation state and the decrease in blood pressure but this occurred in the only medicated group. Based on this finding it was suggested that subthalamic DBS did not affect cardiovascular autonomous responses . Noteworthy, in a previous longitudinal study, the initial differences of blood pressure were not found after 1 years follow-up, with a similar mean blood-pressure decrease for the subthalamic DBS and the only medicated groups . Additionally, two other studies could not find differences in the cardiovascular responses of the treated subjects .
Apomorphine pump/apomorphine injections
Continuous duodenal L-DOPA infusions
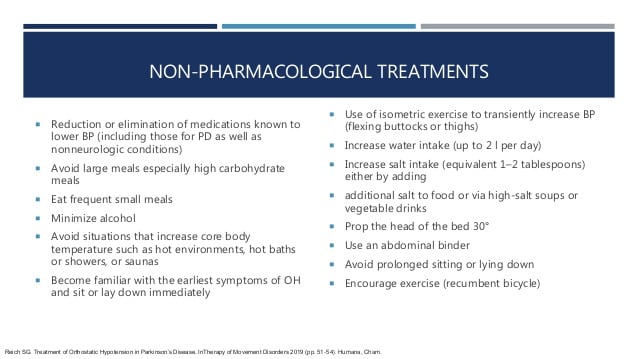
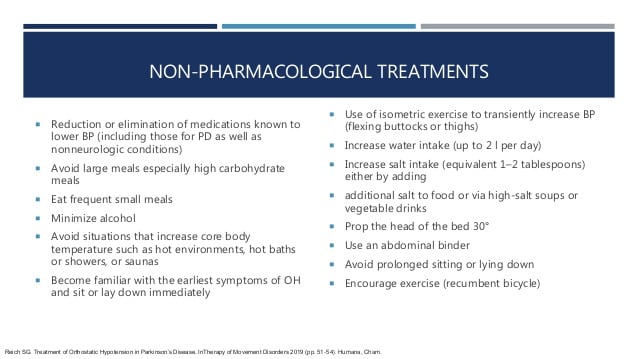
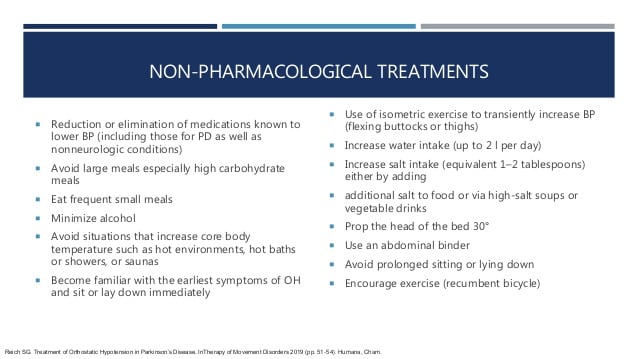
Tips: Avoiding Neurogenic Orthostatic Hypotension
- Drink lots of water and other fluids, at least one cup with meals and two more at other times of the day.
- Regularly practice gentle exercise and avoid long periods of inactivity.
- Eat small, frequent meals. Reduce alcohol intake and avoid hot drinks and hot foods.
- After consulting your doctor, increase your salt intake by eating prepared soups or pretzels. Note: for people with heart disease, this should be avoided.
- If you expect to be standing for a long period of time, quickly drinking two eight-ounce glasses of cold water will increase blood volume and causes blood pressure to go up for several hours.
- Try wearing compression garments such as anti-gravity stockings.
- Do isometric exercises, like marching your legs slowly in place, before getting up.
- Shift slowly from lying to sitting and then standing.
Printing made possible with a grant from Theravance. Content created independently by the Parkinsons Foundation.
For more insights on this topic, listen to our podcast episode Understanding Neurogenic Orthostatic Hypotension.
Medications/lifestyle To Constrict Blood Vessels
- Alcohol dilates blood vessels and dehydrates. Most sources recommend avoiding and/or limiting alcohol. If drinking alcohol, it is extremely important to also drink water.
- Caffeine has different effects on different people. It is dehydrating, so if consuming caffeine, additional water intake is essential. It is generally thought that caffeine dilates blood vessels, which would make it bad for orthostatic hypotension. However, caffeine generally raises blood pressure, which may be helpful for some cases of OH. There are some theories that caffeine primarily dilates smaller capillaries, as opposed to the major blood vessels. Bottom line: Listen to your body, and pay attention to how your body reacts, you may need to avoid caffeine, or you may need your daily fix.
- A recent Michael J. Fox Foundation webinar recommends avoiding hot liquids. Hot liquids too generally promote blood vessel dilation, while cold liquids promote constriction. Caffeine drinkers with OH may want to consider cold beverage options.
- Prescription drugs that are often considered for treatment include Fludrocortisone , Midodrine , Droxidopa , Octreotide and Pyridostigmine. See the references at the bottom of this article for links to research papers that provide more details on these medications.
Recommended Reading: What Are The Different Forms Of Parkinson’s Disease
Is There A Dose
It seems plausible, based on different observational approaches, that higher doses of dopaminergic medications and combined therapies could also increase the chances of manifesting OH. Also some works have suggested that the main effect of medications could be at the beginning of the therapy developing some tolerance thereafter .
Based on all these evidence, the possibility of OH should be especially considered, when starting/adding a new drug or increasing its dose as the probability of symptoms could increase.
Dont Miss: Survival Rate For Parkinsons Disease
Low Blood Pressure In Parkinsons Disease
This 2-page article discusses the frequency of orthostatic hypotension in those with PD, the cause, symptoms and several simple measures that can be used to restore normal blood pressure regulation, including medication evaluation, increase of fluids and salty foods, caffeine, frequent small meals, environment, clothing, slow position change, bed position and medication options.
Dont Miss: Parkinsons Bike Therapy
Also Check: What To Know About Parkinson’s Disease
Whats Hot In Pd If You Are Dizzy Or Passing Out It Could Be Your Parkinsons Disease Or Parkinsons Disease Medications
This 3-page article, with references, is a personal statement by Dr. Okun describing the mis-diagnoses Parkinsons patients can be given when visiting the ER for symptoms of dizziness or syncope outlining what defines a proper diagnosis of orthostatic hypotension, its frequency in people with Parkinsons, medication and lifestyle changes that can help.
Management Of Parkinsons Disease
Overall treatment is specific to the patient and the symptoms they experience. Symptoms can be variable from day to day or even hour to hour therefore, it is important that patients have a good understanding of their treatment, disease, coping mechanism, support system and regular reviews. Life expectancy can be normal however, more advanced symptoms can lead to increased disability and poor health, which may make someone more vulnerable to complications .
Recommended Reading: Best Cbd Oil For Parkinsons
Read Also: Does Parkinson’s Cause Incontinence
First Step: Make The Right Diagnosis
Given its unspecific, and sometimes asymptomatic, presentation, OH should be actively screened at bedside by measuring the BP and heart rate supine and after 3 minutes upon standing . OH is diagnosed in case of a systolic BP fall 20mmHg and/or diastolic 10mmHg with respect to baseline . Standing systolic BP values < 90mmHg are also highly suggestive of OH and often predict symptoms of orthostatic intolerance . In case of milder BP falls at the 3rd minute upon standing, it is recommendable to prolong the orthostatic challenge to 510 minutes, in order to screen for delayed OH, a possible precursor of classic OH .
Once a diagnosis of OH is established, non-neurogenic causes and exacerbating factors, such as dehydration, anemia or infections should be ruled out. The medication schedule should be also reviewed for drugs with BP lowering effect, which may have been recently introduced or increased in dose: not only anti-hypertensive agents, but also dopaminergic drugs, tricyclics, opioids, neuroleptics or -blockers.
Fig.1
Management of orthostatic hypotension and supine hypertension in Parkinsons disease. OH, orthostatic hypotension BP, blood pressure HR, heart rate NSAIDs, non-steroidal anti-inflammatory drugs SNRI, serotonin-noradrenaline reuptake inhibitors. Adapted from Fanciulli et al. 2014 and Fanciulli et al., 2016 with permission from Springer and John Wiley and Sons.
Fig.2
Template of a home blood pressure diary for patients with orthostatic hypotension.
Literature Search And Study Selection
Combining both the lists of titles and abstracts resulted in 836 records. Fig. 1 shows the results of the search and the study selection. A total of 80 full-text articles were selected for further review. Of these, 25 fulfilled our selection criteria. The other 55 articles were excluded for the following reasons: 33 studies reported a mean change of blood pressure after standing for the total patient group instead of the number of patients with OH 8 studies used the presence or absence of autonomic symptoms as inclusion criteria 4 studies were part of a drug trial 4 studies did not include idiopathic PD patients 3 studies had partially overlapping data sets 2 studies were retracted and 1 manuscript could not be retrieved.
Flowchart of the reviewing process.
Read Also: Can Mri Detect Parkinson’s Disease
Preventing And Treating Orthostatic Hypotension: As Easy As A B C
Drug therapy alone is never adequate to treat orthostatic hypotension. A patient-oriented approach that emphasizes education and nonpharmacologic strategies is critical. This article provides easy-to-remember management recommendations, using a combination of drug and non-drug treatments that have proven effective.
Orthostatic Hypotension In Parkinsons Disease Multiple System Atrophy And Lewy Body Dementia
Movement disorder specialist, Dr. Veronica Santini spoke for a half hour on orthostatic hypotension, a common symptom of Parkinsons disease, Multiple System Atrophy and Lewy Body Dementia. Following her talk, moderator Candy Welch, Brain Support Networks MSA caregiver support group leader, presented Dr. Santini with questions from webinar participants for another half hour.
You May Like: Cbd Oil Parkinsons Disease
Also Check: Can Parkinson’s Kill You
Effects Of Parkinsons Disease On Blood Pressure
This short web page explains the physical operation of blood pressure in the body, symptoms of low blood pressure and when they are most likely to occur, why low blood pressure is dangerous, medical treatments and lifestyle strategies to cope with low blood pressure, and a reminder that low blood pressure can affect the ability to drive safely.
Managing Orthostatic Hypotension For Your Safety
Orthostatic hypotension also known as postural hypotension is a form of low blood pressure.
It happens when the blood vessels do not constrict as you stand up from a sitting or lying position.
It can also be experienced as a side-effect of medication taken for Parkinsons, or when a person is taking anti-hypertensive medications when they are no longer required. Orthostatic hypotension can also be a pointer to a Parkinsons diagnosis.
Its symptoms include:
- Feeling dizzy or light- headed
- Blurred vision
How to manage orthostatic hypotension:
- Do not sit or stand or be inactive for long periods
- Avoid activity in the heat
- Stay cool
- Prior to getting up, move your toes around and adjust your heels and calf muscles
- Allow your feet to dangle on the floor for a short time if getting out of bed
- Gentle marching leg movements may also help
- Get up slowly, stand for a short time and monitor for steadiness
- If feeling dizzy or faint, sit with your legs elevated until the feeling passes
- Ensure that you are well hydrated drink a glass of water prior to getting up
- If feeling dizzy at the end of a meal, try having a glass of water then
- Reach over slowly and find a hand-hold to prevent over balancing
- Eat smaller meals more frequently
- Avoid straining whilst having bowels open
- Avoid vigorous exercise
Read Also: What Helps Parkinson’s Patients Sleep
Management Of Orthostatic Hypotension In Parkinsons Disease
Issue title: Special Issue: Clinical management of Parkinsons disease: Essentials and new developments
Guest editors: Bastiaan R. Bloem and Patrik Brundin
Article type: Review Article
Authors: Fanciulli, Alessandraa * | Leys, Fabiana | Falup-Pecurariu, Cristianb | Thijs, Rolandc d | Wenning, Gregor K.a
Affiliations: Department of Neurology, Medical University of Innsbruck Innsbruck, Austria | Department of Neurology, Transilvania University, Faculty of Medicine Brasov, Romania | Department of Neurology, Leiden University Medical Centre, Leiden, The Netherlands | Stichting Epilepsie Instellingen Nederland , Heemstede, The Netherlands
Correspondence: Correspondence to: Alessandra Fanciulli, MD, PhD, Department of Neurology, Medical University of Innsbruck, Anichstraße 35, A-6020 Innsbruck, Austria. Tel.: +43 512 504 83238 E-mail: .
Keywords: Parkinsons disease, orthostatic hypotension, post-prandial hypotension, supine hypertension, nocturnal hypertension
DOI: 10.3233/JPD-202036
Journal: Journal of Parkinson’s Disease, vol. 10, no. s1, pp. S57-S64, 2020
Abstract
Normal Ans Response To Standing
Postural change induces gravitational redistribution of blood volume, leading to changes in blood pressure. Upon standing, pooling of venous blood in the legs is countered by the normal sympathetic ANS to maintain standing blood pressure. Lying supine also causes gravitational redistribution of blood volume, and the normal ANS minimizes blood pressure from rising too high. Norepinephrine is the major neurotransmitter in the ANS regulation of blood pressure in response to postural changes. Sympathetic activation in response to standing leads to: venoconstriction with increased venous return an increase in heart rate and myocardial contractility with increased cardiac output and vasoconstriction with increased blood pressure. Normal activation of the intact ANS, along with sufficient circulating blood volume, prevents the gravity-induced fall in standing systolic blood pressure , maintaining cerebral perfusion and of other vital organs.
You May Like: What Is An Off Period In Parkinsons
Read Also: Does Parkinson’s Affect Your Eyesight
Prevalence Of Orthostatic Hypotension
A decrease of at least 20 mm Hg in systolic blood pressure values was found in 53 of the ninety one patients investigated. The postural fall in blood pressure was asymptomatic in 35 and associated with at least one clinical event in 18 patients .
When a 20 mm Hg decrease in systolic blood pressure was chosen as the main criteria for orthostatic hypotension, patients with orthostatic hypotension did not differ from those without it regardless of age, sex, disease duration, daily levodopa dose, or daily bromocriptine intake . The proportion of patients receiving bromocriptine was significantly higher in the group of patients with manometric orthostatic hypotension than in patients without . There was no significant difference between patients with or without orthostatic hypotension for other antiparkinsonian drugs such as lisuride , deprenyl , or domperidone . The presence of manometric orthostatic hypotension was not associated with arterial hypertension or antihypertensive drug intake . The severity of the disease assessed using Hoehn and Yahrs classification was significantly higher in patients with than without orthostatic hypotension .
Clinical characteristics of patients with Parkinsons disease without orthostatic hypotension , with asymtomatic OH fall 20 mm Hg without postural symptoms) and with symptomatic OH
When Is Orthostatic Hypotension Treated
Not all forms of orthostatic hypotension require treatment. If you experience a drop in blood pressure when you stand up, but have no other symptoms you probably wont need treatment. Sometimes all it takes is sitting on the edge of the bed for a minute or steadying yourself for a moment after you stand up. But, if you feel dizzy or lightheaded to the point where you might lose your balance or lose consciousness, you will need treatment.
Because some drugs can cause severe orthostatic hypotension, your doctor may first try reducing some of your medicine or may switch you to another type of medicine. If you have significant symptoms of orthostatic hypotension, and it is not possible to change your medications, then your doctor will likely treat the orthostatic hypotension itself.
Also Check: How Long Can Someone Live With Parkinson’s
What Are The Neurogenic Causes Of Orthostatic Hypotension
Autonomic neuropathy is a common cause of neurogenic OH. Possible etiologies of autonomic neuropathy are too numerous to list but include diabetes mellitus, amyloidosis, toxic neuropathies , infections, autoimmune diseases, hereditary conditions, paraneoplastic syndromes, and metabolic disorders. provides a summary of the most common causes of peripheral autonomic neuropathies to help guide further diagnostic testing based on clinical plausibility.
Relevant causes of peripheral autonomic neuropathies to help guide the diagnostic evaluation
An approach to sorting out the neurogenic causes of OH involves considering the type of associated neurologic findings and whether the onset of the OH was acute/sub-acute or chronic and progressive. Using this approach, the following 5 distinct categories arise:
No neurologic symptoms, acute or sub-acute onset . Consider autoimmune or paraneoplastic ganglionopathy and toxic exposures, particularly neurotoxic drugs. These cases often go undiagnosed. It is essential that these conditions be identified because they often have specific therapy, such as immunomodulatory therapy for autonomic ganglionopathies or removal of a potentially toxic drug.
No neurologic symptoms, chronic, slow progression. Consider pure autonomic failure, a synucleinopathy that usually presents without nonautonomic features but often progresses to Parkinson disease or multiple system atrophy after prolonged follow-up.
Living With Postural Hypotension
This 7-page fact sheet was developed for people affected by MSA, but is just as useful to those with Parkinsons disease, who are experiencing drops in blood pressure and postural hypotension. It covers symptoms, when they are likely to happen, what to do, exercise and other tips for daily living with OH, including medication options.
Don’t Miss: How To Tell If Someone Has Parkinson’s
Impaired Ans Response To Standing In Noh
In patients with PD and nOH, autonomic dysfunction causes blood pressure to fall upon standing, due to an inappropriate NE response to postural change. Orthostatic hypotension has been defined as a drop in SBP of at least 20 mmHg or a drop in diastolic blood pressure of at least 10 mmHg after 3 minutes of standing. There is often a loss of the cardioacceleratory response too. Non-neurogenic causes of orthostatic hypotension are also common in patients with PD, and contribute to blood pressure drop. These non-neurogenic causes of orthostatic hypotension should be identified first, and include dehydration, medications, and cardiac pump failure. A clinical diagnosis of nOH can be made when these non-neurogenic causes of persistent orthostatic hypotension are excluded, and can be confirmed through autonomic testing and plasma NE levels.
In PD, autonomic dysfunction is mainly a result of cardiac sympathetic denervation with inadequate activation of NE pathways, and also baroreflex failure. This can emerge during the course of PD or can occur early in its course. Parkinsonism due to multiple system atrophy is also accompanied by prominent autonomic dysfunction, but nOH results from failure of central NE pathways.,
Orthostatic Hypotension: A Prodromal Marker Of Parkinsons Disease
Department of Epidemiology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Department of Neurology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Francesco U.S. Mattace Raso PhD
Department of Geriatric Medicine, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Department of Epidemiology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Department of Neurology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Correspondence to: Dr. M. Kamran Ikram, Erasmus MC University Medical Center, P.O. Box 2040, 3000 CA Rotterdam, the Netherlands E-mail:
Department of Epidemiology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Department of Neurology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Francesco U.S. Mattace Raso PhD
Department of Geriatric Medicine, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Department of Epidemiology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Department of Neurology, Erasmus MC University Medical Center, Rotterdam, the Netherlands
Correspondence to: Dr. M. Kamran Ikram, Erasmus MC University Medical Center, P.O. Box 2040, 3000 CA Rotterdam, the Netherlands E-mail:
Lisanne J. Dommershuijsen and Alis Heshmatollah contributed equally to this article.
Relevant conflicts of interests/financial disclosures:: Nothing to report.
Read Also: Physiotherapy Management For Parkinsons Disease Ppt
Read Also: What Is Usually The First Symptom Of Parkinson Disease
