Support For People With Parkinsons Disease
Early access to a multidisciplinary support team is important. These teams may include doctors, physiotherapists, occupational therapists, speech therapists, dietitians, social workers and specialist nurses.
Members of the team assess the person with Parkinsons disease and identify potential difficulties and possible solutions.
There are a limited number of multidisciplinary teams in Victoria that specialise in Parkinsons disease management. But generalist teams are becoming more aware of how to help people with Parkinsons disease.
Learn More About Parkinsons Disease
Parkinsons Disease: The Essentials
If youre new to Parkinsons disease and would like a good overview to help you better understand the disease, please view our Parkinsons Disease: The Essentials presentation. Its a great place to get started with reliable and concise information.
Causes
The exact cause of Parkinsons is still unknown, but there is an enormous amount of research being done to learn more. This research has led scientists to formulate a number of theories on the cause of this disease.
Diagnosing
While there is no definitive test that can be taken to determine whether a person has Parkinsons disease, movement disorder specialists look for symptoms and use brain imaging technology to accurately diagnose Parkinsons.
Symptoms
Even though Parkinsons is classified as a movement disorderand its motor symptoms are the most discussed and well-knownthere are many non-motor symptoms that display in people with Parkinsons as well.
Treatments
As of today, there is no cure for Parkinsons disease. But there are many ways in which the disease can be treated to make symptoms more manageable.
Living With Parkinsons
Discuss The Latest Research In The Parkinsons News Today Forums
All individuals ages 45 and older who participated in the five cohort studies in California, Minnesota, Hawaii, and Ontario, Canada, were included in the calculations.
The overall estimated prevalence of Parkinsons disease in the U.S. population, according to the 2010 census, was 572 per 100,000. These estimates were higher in men than in women , and values rose with age in both genders.
Data indicated that in 2010 about 680,000 individuals in the U.S. ages 45 and older had been diagnosed with the disease. Given the projected future growth of the population, the researchers predicted this number will rise to 930,000 cases in 2020, and to 1,238,000 by 2030.
Geographical analysis of the data showed that, for all regions except Olmsted County, Minnesota, and Northern California, the estimated numbers were in accordance with those retrieved from the Medicare database. For Olmsted County, 14-27% more cases of Parkinsons were identified in the study than in the Medicare data. In Northern California, the study indicated 30% more Parkinsons cases than in the Medicare data.
This finding suggests regional variation deserves to be studied so researchers can understand if variations result from differences in susceptibility to the disease or in access to or utilization of healthcare services, the authors wrote.
Don’t Miss: Parkinson’s With Lewy Body
What Are The Stages Of Parkinsons Disease
Parkinsons disease is often divided into two parts: early stage and advanced stage disease.
- Early stage: when symptoms appear and start to affect everyday activities, such as washing, getting dressed and walking.
- Advanced stage: when motor complications occur from the long term use of one of the main treatments for Parkinsons disease, levodopa.
Writing And Talking About Parkinson’s
Based on feedback from the Parkinson’s community, here are the preferred words and terms for talking about Parkinson’s, and the ones to avoid. If you’re unsure about any of this, please get in touch with our Media and PR team:
- When describing people with, affected by, or living with Parkinson’s, use ‘people living with Parkinson’s’.
- Avoid saying ‘suffering’, ‘surviving’, ‘battling’. Also avoid ‘victims’ or ‘sufferers’.
Parkinson’s, symptoms and medication:
- When talking about Parkinson’s, always refer to it as simply ‘Parkinson’s’ or a/the ‘condition’.
- Avoid saying ‘Parkinson’s disease’.
Recommended Reading: Tests To Confirm Parkinson’s Disease
How Were These Figures Calculated
We analysed anonymous medical records of over 2.5 million individuals over the age of 20 registered with GPs in the UK from the Clinical Practice Research Datalink database.
Clinical experts helped us assess the records to work out how many patients had a definite diagnosis of Parkinsons and then we adjusted the numbers to make sure they matched the UK population in terms of age profile and gender.
Finally, we used projected population figures from the Office of National Statistics, to estimate how many people have Parkinsons in 2018 and how many will go on to be diagnosed in 2025 and beyond.
The UK population is growing and people are living longer, which means that the number of people of people living with Parkinsons is expected to rise.
For more information, you can
Dont Miss: Boxing And Parkinsons Disease
Trends In The Pd Incidence
Globally, the incident number of PD was 1,081.72 × 103 in 2019, which increased 159.73% since 1990. The overall age-standardized incidence rate was 13.43/100,000 in 2019, and it increased with an annual average of 0.61% from 1990 to 2019 . Compared to female patients, male patients had a larger incident number, and a higher increasing trend in ASIR . Among the age groups, the high incident numbers of PD were observed in the patients aged over 65 years, and the largest increasing percentage occurred in the age group of over 80 years .
Table 1. The changes in incidence and prevalence of Parkinson’s disease worldwide, and in sexes, SDI areas, and regions, 19902019.
Figure 1. Trends in the ASR of incidence, prevalence, and YLDs of Parkinson’s disease in global, SDI areas and geographic regions from 1990 to 2019. ASR, age-standardized rate SDI, sociodemographic index YLDs, years lived with disability.
Figure 2. The distribution of Parkinson’s disease incidence in age groups, SDI areas and geographic regions from 1990 to 2019. was the incident number in age groups was the ASIR in SDI areas was the incident number in geographical regions. ASIR, age-standardized incidence rate SDI, sociodemographic index.
Also Check: Does Parkinson’s Affect Heart Rate
Number Of People With Parkinsons
The number of people with Parkinsons in New Zealand has been steadily increasing, from an estimated 7,000 in 2006 to 11,000 in 2020 . We project that the number of people in New Zealand with Parkinsons is expected to reach 22,000 by 2040. This is due to the ageing population, which puts more people into the highest risk age groups , and also due to people now living longer with the disease.
Figure 1: Number of people in New Zealand that have Parkinsons.
Read Also: Adaptive Silverware For Parkinsons
How Is Parkinsons Diagnosed
Doctors use your medical history and physical examination to diagnose Parkinsons disease . No blood test, brain scan or other test can be used to make a definitive diagnosis of PD.
Researchers believe that in most people, Parkinsons is caused by a combination ofenvironmental and geneticfactors. Certain environmental exposures, such as pesticides and head injury, are associated with an increased risk of PD. Still, most people have no clear exposure that doctors can point to as a straightforward cause. The same goes for genetics. Certain genetic mutations are linked to an increased risk of PD. But in the vast majority of people, Parkinsons is not directly related to a single genetic mutation. Learning more about the genetics of Parkinsons is one of our best chances to understand more about the disease and discover how to slow or stop its progression.
Aging is the greatest risk factor for Parkinsons, and the average age at diagnosis is 60. Still, some people get PD at 40 or younger.
Men are diagnosed with Parkinsons at a higher rate than women and whites more than other races. Researchers are studying these disparities to understand more about the disease and health care access and to improve inclusivity across care and research.
Aging is the greatest risk factor for Parkinsons, and the average age at diagnosis is 60. Still, some people get PD at 40 or younger.
The Michael J. Fox Foundation has made finding a test for Parkinsons disease one of our top priorities.
Read Also: American Academy Of Neurology Parkinson Disease Treatment Guidelines
Michael J Fox: Parkinsons Champion For A Cure
Michael J. Fox is among the most well-known people living with Parkinsons disease. Many remember him as the fresh-faced young star of the 1980s TV comedy hit Family Ties and the popular Back to the Future movies. Though most people with Parkinsons are diagnosed between ages 40 and 60, Fox was diagnosed at age 30 but his diagnosis didnt slow him down.
He shared his young-onset Parkinsons disease diagnosis with the world in 1998 and, two years later, founded the Michael J. Fox Foundation for Parkinsons Research. Fox is committed to helping the foundation build Parkinsons disease awareness and raise funds for research into prevention, treatment, and a cure. In addition to his advocacy work, hes still a working actor some more recent roles have included characters with Parkinsons in the TV shows The Good Wife and Curb Your Enthusiasm.
As long as I play a guy with Parkinsons, I can do anything, he joked in a 2013 AARP interview.
How Soon After Treatment Will I Feel Better And How Long Will It Take To Recover
The time it takes to recover and see the effects of Parkinson’s disease treatments depends strongly on the type of treatments, the severity of the condition and other factors. Your healthcare provider is the best person to offer more information about what you can expect from treatment. The information they give you can consider any unique factors that might affect what you experience.
Also Check: Can Parkinson’s Affect Eyesight
Sidebar: Morris K Udall Centers Of Excellence For Parkinson’s Disease Research
The Morris K. Udall Parkinsons Disease Research Act of 1997 authorized the NIH to greatly accelerate and expand PD research efforts by launching the NINDS Udall Centers of Excellence, a network of research centers that provide a collaborative, interdisciplinary framework for PD research. Udall Center investigators, along with many other researchers funded by the NIH, have made substantial progress in understanding PD, including identifying disease-associated genes investigating the neurobiological mechanisms that contribute to PD, developing and improving PD research models, and discovering and testing potential therapeutic targets for developing novel treatment strategies.
The Udall Centers continue to conduct critical basic, translational, and clinical research on PD including: 1) identifying and characterizing candidate and disease-associated genes, 2) examining neurobiological mechanisms underlying the disease, and 3) developing and testing potential therapies. As part of the program, Udall Center investigators work with local communities of patients and caregivers to identify the challenges of living with PD and to translate scientific discoveries into patient care. The Centers also train the next generation of physicians and scientists who will advance our knowledge of and treatments for PD. See the full list of Udall Centers.
The Following Issues Are At The Forefront Of The Discussion
There are no clear answers to these questions yet, but as state registries develop, each will need to consider these points:
What are the best ways to ensure privacy and protection of data?
Privacy is of supreme concern to all those who are involved in registries. As registries evolve and grow, the focus remains on ensuring that data is protected and secure.
What data should be collected in a registry?
The data could theoretically be more limited, including just basic demographics, or it could be expanded to include more wide-reaching information such as date of diagnosis, symptoms, and treatments. This additional information could be very useful to researchers to better understand how PD is diagnosed and treated across the population. Ideally, the data elements collected would be standardized across registries so that data could be aggregated amongst the different registries.
Who should be in the registry?
Should it include only people with a clear diagnosis of PD, or should it include cases of atypical parkinsonism which are related neurodegenerative disorders?
What is the best way to enroll cases in the registry?
As discussed above, automatically pulling cases from the electronic medical records is how it is done in California. Other options include having patients report themselves into the database or pulling pharmacy records for prescriptions of Parkinsons medications.
Read Also: Is It Parkinson’s Or Something Else
What Is The Prevalence
It is important to understand the difference between incidence and prevalence. Incidence is the number of new cases of a disease that are diagnosed in a time period. Usually, incidence is the number of new cases per year.3
Prevalence is the number of cases of a disease that exist at any point in time. This number is larger because it includes new cases and all the existing cases of a disease.3
In 2014, the Parkinsons Foundation started a project to get a better measurement of PD prevalence. Currently, there are an estimated 1 million people in the United States living with PD. About 60,000 people in the United States are diagnosed each year with PD in the United States. Experts estimate there will be 1.2 million people in the United States living with PD by 2030.1,3
No One Definitive Cause Of Parkinsons
There are no biomarkers or objective screening tests that indicate one has Parkinsons. That said, medical experts have shown that a constellation of factors are linked to it.
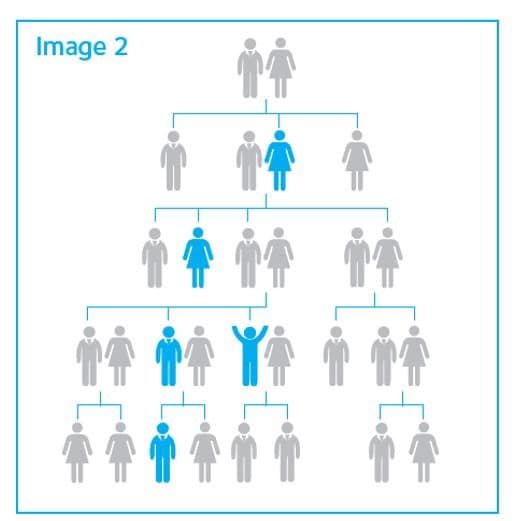
Parkinsons causes are likely a blend of genetics and environmental or other unknown factors. About 10 to 20 percent of Parkinsons disease cases are linked to a genetic cause, says Ted Dawson, M.D., Ph.D., director of the Institute for Cell Engineering at Johns Hopkins. The types are either autosomal dominant or autosomal recessive .
But that leaves the majority of Parkinsons cases as idiopathic, which means unknown. We think its probably a combination of environmental exposure to toxins or pesticides and your genetic makeup, says Dawson.
Age. The biggest risk factor for developing Parkinsons is advancing age. The average age of onset is 60.
Gender. Men are more likely to develop Parkinsons disease than women.
Genetics. Individuals with a parent or sibling who is affected have approximately two times the chance of developing Parkinsons. Theres been an enormous amount of new information about genetics and new genes identified over the past 10 or 15 years that have opened up a greater understanding of the disease, says Dawson.
You May Like: Types Of Exercise For Parkinson’s Disease
More Americans Are Dying From Parkinson’s Disease
HealthDay Reporter
THURSDAY, Oct. 28, 2021 — The number of Americans who are dying from Parkinson’s disease has jumped by 63% in the past two decades, new research shows.
The fresh analysis also revealed that men face double the risk of dying from the progressive and incurable disease than women. A notably higher death rate was also seen among white people, as compared with peers of other racial/ethnic backgrounds.
“The message is straightforward,” said study author Dr. Wei Bao. “This study showed that an increasing number of people died from Parkinson’s disease during the past 20 years, and this cannot be simply explained by population aging.”
Bao is an associate professor in the department of epidemiology at the University of Iowa’s College of Public Health, in Iowa City. He and his colleagues published their findings online Oct. 27 in the journal Neurology.
According to the Michael J. Fox Foundation, Parkinson’s affects roughly 1 million Americans and more than 6 million people around the world.
To get a handle on trends among Parkinson’s patients, Bao and his colleagues analyzed data collected by the U.S. National Vital Statistics System.
The team found that nearly 480,000 Americans died of Parkinson’s between 1999 and 2019.
That steady rise translated into nearly nine out of every 100,000 Americans succumbing to Parkinson’s by 2019. That figure is notably up from a little more than five Parkinson’s deaths for every 100,000 Americans just 20 years earlier.
Are There Places Where Parkinsons Is More Or Less Common
In general, research suggests that the prevalence of Parkinsons is higher in Europe and the United States than in Asian, Latin American and African countries.
These differences may be largely explained by differences in the age-profile. If the population has more younger people and a lower life expectancy then its likely to have a lower number of people with Parkinsons. And in developing nations this may be compounded if they have less developed healthcare systems as Parkinsons is much less likely to be diagnosed or researched.
Although, there have been some reports of specific areas where Parkinsons is more or less common than expected, its usually difficult to prove these hotspots are not simply due to chance, or to see the same patterns in other similar areas.
You May Like: What Type Of Doctor Diagnosis Parkinson’s Disease
What Is The Trend Over Time In The Prevalence And Incidence Of Parkinsonism In Canada
Between 20042005 and 20132014, the number of Canadians living with diagnosed parkinsonism increased from approximately 61,000 to 84,000, while the number of Canadians newly diagnosed increased from approximately 8,000 to 10,000. However, during the same period, there was no significant change in the age-standardized prevalence proportion, which remained at 0.4%, or the incidence rate, which went from 51.6 per 100,000 to 52.6 per 100,000. The sex differential also remained constant over time for both indicators .
Figure 3: Age-standardized prevalence and incidence of diagnosed parkinsonism, including Parkinsons disease, among Canadians aged 40 years and older, by sex, 20042005 to 20132014
| Indicator | |
|---|---|
| 67.8 | 40.3 |
Notes: Age-standardized estimates to the 2011 Canadian population. The 95% confidence interval shows an estimated range of values which is likely to include the true value 19 times out of 20. The 95% confidence intervals of the prevalence estimates are too small to be illustrated.Data source: Public Health Agency of Canada, using Canadian Chronic Disease Surveillance System data files contributed by provinces and territories, July 2017.
