Parkinson’s Disease Dementia Surgery And Gene Therapy
- Great strides have been made in the surgical treatment of Parkinson’s disease. Several different procedures are now available, and they are successful in many patients in relieving movement symptoms. Unfortunately, surgery has no effect on cognitive symptoms. In fact, most people with dementia are not candidates for surgery.
- Gene therapy is in its infancy; there are ongoing human and animal trials with various methods to insert genes into neuronal cells to reduce or stop Parkinson’s disease symptoms by causing cells to produce dopamine coded by the newly inserted genes. Early results with the treatment termed ProSavin are encouraging. However, it is not clear if such therapy could prevent or reverse Parkinson’s disease dementia.
Tip 2: Whatand Howyou Eat Can Make A Difference
Theres no specific Parkinsons disease diet, but by adjusting your eating habits, you can help protect your brain. Diets that are good for your heart tend to also be good for brain health. Eating habits such as those promoted in the Mediterranean diet can help reduce inflammation, protect neurons, and promote better communication between brain cells.
Primarily, its important to eat plenty of fruit and vegetables, cut down on sugary foods and refined carbs, reduce fried and processed foods, and boost your intake of healthy fats and home-cooked meals. High protein meals may also help to benefit your brain chemistry.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
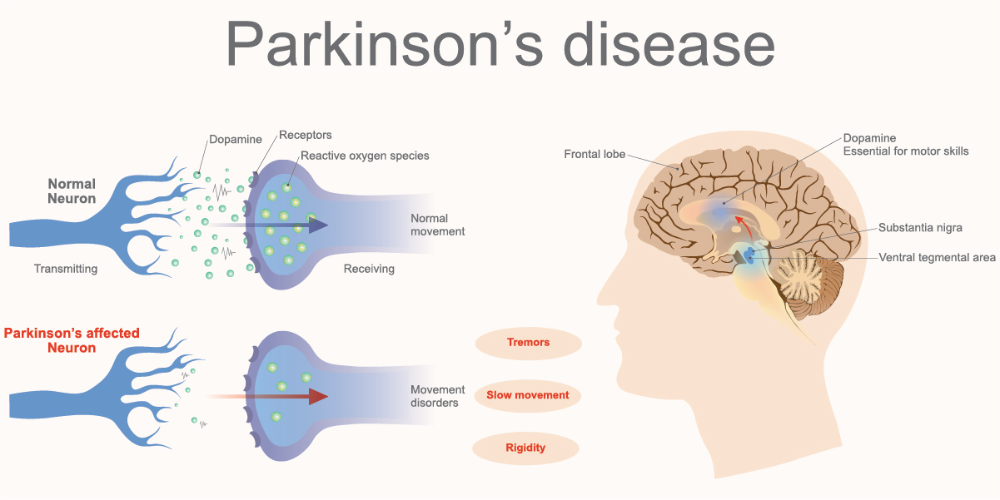
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Recommended Reading: Does Parkinson’s Affect Speech
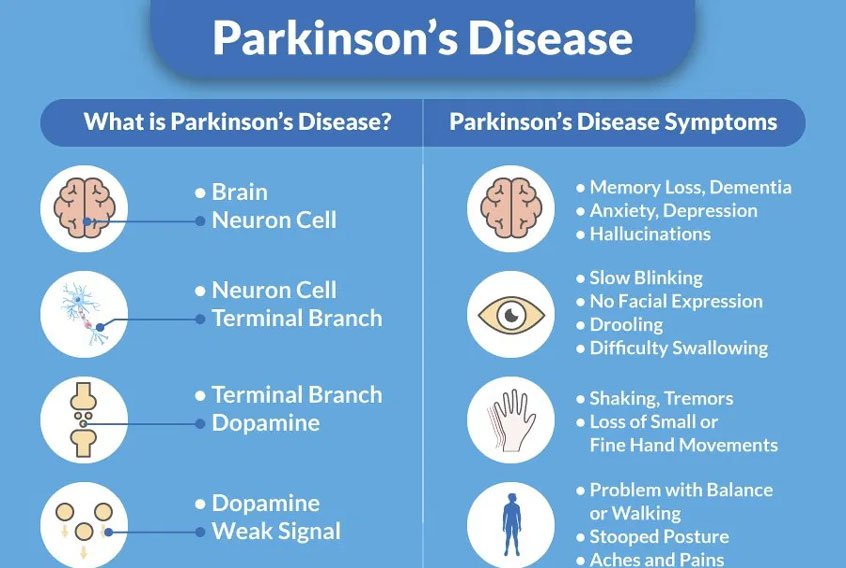
Behaviors Seen In Parkinsons Disease Dementia
As dementia progresses, managing disorientation, confusion, agitation, and impulsivity can be a key component of care.
Some patients experience hallucinations or delusions as a complication of Parkinsons disease. These may be frightening and debilitating. Approximately 50 percent of those with the disease may experience them.
The best thing to do when giving care to someone experiencing hallucinations or delusions from Parkinsons disease dementia is to keep them calm and reduce their stress.
Take note of their symptoms and what they were doing before they exhibited signs of hallucinating and then let their doctor know.
This element of the disease can be particularly challenging for caregivers. Patients may become unable to care for themselves or be left alone.
Some ways to make caregiving easier include:
- sticking to a normal routine whenever possible
- being extra comforting after any medical procedures
- limiting distractions
- using curtains, nightlights, and clocks to help stick to a regular sleep schedule
- remembering that the behaviors are a factor of the disease and not the person
Living With Parkinson Disease
These measures can help you live well with Parkinson disease:
- An exercise routine can help keep muscles flexible and mobile. Exercise also releases natural brain chemicals that can improve emotional well-being.
- High protein meals can benefit your brain chemistry
- Physical, occupational, and speech therapy can help your ability to care for yourself and communicate with others
- If you or your family has questions about Parkinson disease, want information about treatment, or need to find support, you can contact the American Parkinson Disease Association.
Also Check: Can Cannabis Help Parkinson’s Disease
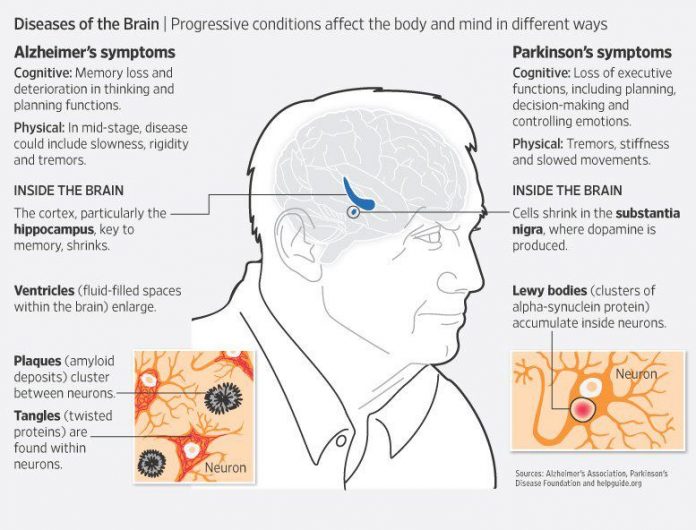
Lewy Body Dementia Vs Parkinsons Disease Dementia
Diagnoses of Lewy body dementia include dementia with Lewy bodies and Parkinsons disease dementia. Symptoms in both of these diagnoses can be similar.
Lewy body dementia is a progressive dementia caused by abnormal deposits of a protein called alpha-synuclein in the brain. Lewy bodies are also seen in Parkinsons disease.
The overlap in symptoms between Lewy body dementia and Parkinsons disease dementia include movement symptoms, rigid muscles, and problems with thinking and reasoning.
This seems to indicate that they could be linked to the same abnormalities, though more research is needed to confirm that.
The later stages of Parkinsons disease have more severe symptoms that may require help moving around, around-the-clock care, or a wheelchair. Quality of life can decline rapidly.
Risks of infection, incontinence, pneumonia, falls, insomnia, and choking increase.
Hospice care, memory care, home health aides, social workers, and support counselors can be a help in later stages.
Parkinsons disease itself isnt fatal, but complications can be.
Research has shown a median survival rate of about
Efns Task Force Recommendations
A joint task force of the EFNS and the European section of the MDS provided their recommendations for the therapeutic management of PD in 2006, including a section devoted to the management of non-motor problems in PD, such as dementia . Although they acknowledged that cognitive improvements in patients with PDD treated with cholinesterase inhibitors were modest, they classified clinical evidence with rivastigmine and donepezil as class I and II studies respectively. For overall management, they recommended both discontinuation of medications that might impair cognition and the addition of cholinesterase inhibitor therapy either with rivastigmine or with donepezil . Additionally, the authors recommended that the addition of cholinesterase inhibitor therapy with rivastigmine or donepezil may also help in the treatment of psychosis in this population .
Read Also: What Body Systems Are Affected By Parkinson’s Disease
Advice For Carers Family And Friends
Living with or caring for someone with Parkinsons disease dementia can be challenging. Sometimes help and support will be relied on heavily but there will be times when it will be better to step back and allow the person with dementia to do things for themselves. This balance will be difficult to judge at first, but with time and patience new routines and approaches to day-to-day living can be established.
It is important to encourage, stimulate and help the person with dementia, but remember too that rest is important.
Can Parkinsons Disease Make You Aggressive
Parkinsons disease Dementia or PD Dementia can make a patient very aggressive. Parkinsons Dementia Aggression germinating from Parkinsons disease Dementia can lead patients to behave erratically, experience sudden anger outbursts, feel constantly irritated, and always be in a state of restlessness. Outbursts are generally in the form of:
- Shouting
- Falling
You May Like: Does Parkinson’s Skip A Generation
Dysexecutive Symptoms May Emerge When Inter
How dysfunction in the fronto-striatal and mesocortical dopaminergic networks may interact to cause dysexecutive symptoms in PDD is unclear. However the results of suggest that it is supervening dysfunction in the mesocortical projections to the insular upon existing fronto-striatal network disruption that heralds major executive impairment. Indeed there is limited evidence suggesting some redundancy between the two systems in early Parkinsons disease: in one study patients performing a set-shifting task did not display behavioural impairment despite fronto-striatal hypoactivation on functional MRI, possibly because they displayed concurrent hyper-activation in the insular and fronto-parietal networks, which was not present in controls . Using functional MRI, also noted a relative increase in blood-oxygen level-dependent activity within frontal regions in patients during a matching task. Although this evidence is indirect it suggests that the mesocortical network may partially compensate for fronto-striatal dysfunction in early disease, until it too is damaged, compensation is lost, and a full-blown dysexecutive syndrome develops. Such a proposal is compatible with, and extends, the hypothesis proposed by others that deficient interplay between the fronto-striatal and mesocortical dopamine networks underlies the dysexecutive syndrome of Parkinsons disease .
Memory And Thinking Problems
You may experience forgetfulness, slowed thinking and difficulty concentrating. You might find it harder to follow conversations, and remember some words and names. This can make communication difficult.
You may also find it increasingly difficult to make decisions, plan activities and solve problems. This can make everyday activities harder.
Also Check: Which Is Better For Parkinson’s Indica Or Sativa
Degeneration In The Mesocortical Dopamine Network Contributes To Executive Dysfunction
However, dopamine-dependent neural circuitry underlying executive deficits in Parkinsons disease may not be limited to the fronto-striatal network alone. The mesocortical dopamine network originates in the midbrain ventral tegmental area and projects diffusely to neocortical areas, particularly prefrontal, insular and cingulate cortices . Release of dopamine from this network modulates prefrontal D2 receptors and thereby facilitates cognitive flexibility, a core feature of executive processing . Insular cortex in particular is considered to mediate such flexibility, acting as a hub to recruit other cognitive circuits such as the fronto-parietal network . In support of this, insular lesions in human patients have been shown to impair performance on tasks requiring cognitive flexibility .
Epidemiology And Natural History Of Dlb And Pdd
Approximately 12% of those aged above 65;years are diagnosed with DLB worldwide , affecting approximately 5% of all dementia cases in those over the age of 75 . Its incidence is 0.71.4 new cases/100,000 person-years or 3.5/100,000 person-years . For PDD, the cumulative prevalence is of 75% of PD patients surviving more than 10;years , 83% after 20;years , and up to 95% by age 90;years , with an overall prevalence of 31.1% and incidence rates from 0.43 to 1.13/100,000 person-years , indicating that, annually, approximately 10% of a PD population will develop dementia . The data concerning age at disease or dementia onset are highly variable. Whereas in the Olmsted County study DLB patients were younger at symptom onset than those with PDD and had more hallucinations and cognitive fluctuations, others have reported younger age at disease onset in PDD , or no essential differences between disorders .
Recommended Reading: What Is Freezing In Parkinson’s
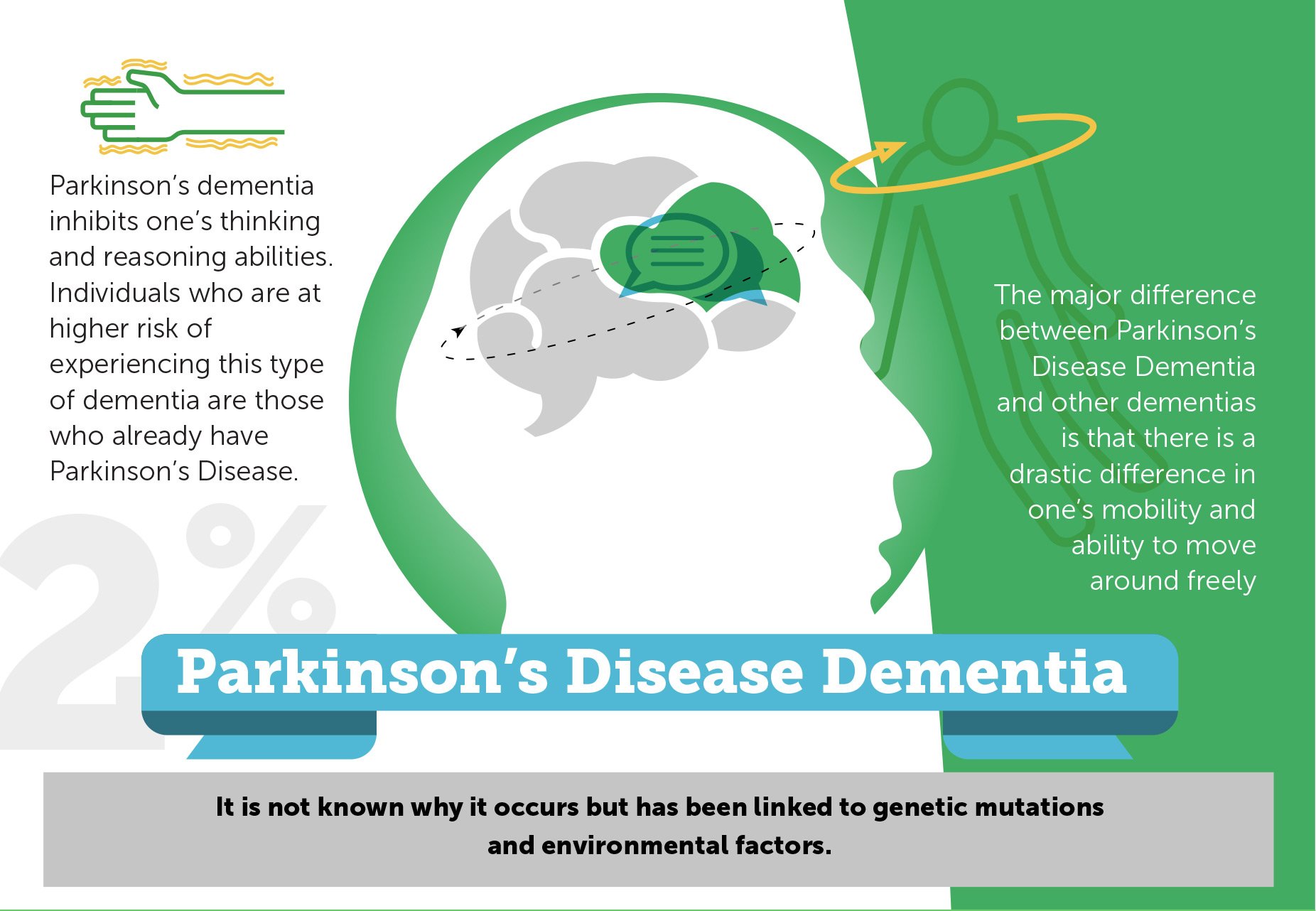
How Is Parkinsons Disease Dementia Different From Alzheimers Disease
Parkinsons disease Dementia must not be confused with Alzheimers disease. Dementia is a hallmark feature of Alzheimers whereas a patient may not necessarily contract Dementia if he happens to contract Parkinsons. Having mentioned that, Dementia does have a greater social and occupational impact on the functioning of people when it affects someone with Parkinsons as compared to Alzheimers.
This is due to the combination of motor and cognitive impairments. Parkinsons directly affects problem-solving functions in a person, besides other aspects such as the speed of thinking, memory, and mood. Parkinsons Dementia Aggression can also be related to Lewy bodies, where sticky clumps of protein are found in the nerve cells of people diagnosed with Parkinsons.
Finally, it must be known to all those associated with Parkinsons in any capacity, whether be it a patient or a caregiver, that majority of people with Parkinsons may experience some of the other forms of cognitive impairment over time. Though cases vary from person to person, the development of Dementia in those diagnosed with Parkinsons cannot be predicted. To put it in numbers, 30 percent of people with Parkinsons never develop dementia as a part of their progression.
How Is Parkinson Disease Treated
Parkinson disease can’t be cured. But there are different therapies that can help control symptoms. Many of the medicines used to treat Parkinson disease help to offset the loss of the chemical dopamine in the brain. Most of these medicines help manage symptoms quite successfully.
A procedure called deep brain stimulation may also be used to treat Parkinson disease. It sends electrical impulses into the brain to help control tremors and twitching movements. Some people may need surgery to manage Parkinson disease symptoms. Surgery may involve destroying small areas of brain tissue responsible for the symptoms. However, these surgeries are rarely done since deep brain stimulation is now available.
Don’t Miss: Can Boxing Cause Parkinson’s Disease
Do You Die From Pd Dementia
People with Parkinsons-related dementia often want to know how the disease can impact their lifespan. While people with Parkinsons can expect a similar lifespan to the general population, studies show both Parkinsons disease dementia and Lewy body dementia can shorten lifespan, generally due to medical complications from the disease, rather than the disease itself.;
Is There A Test To Diagnose Pd Dementia
There is no single test for PDD. The diagnosis is made clinically. If you or someone you spend time with notices cognitive changes, it is important to discuss them with your care team. If you dont have a care team in place, its important to find a specialist or physician familiar with dementia or geriatric medicine. Call the Parkinson’s Foundation Helpline 1-800-4PD-INFO for a referral.
Read Also: What Foods Are Good For Parkinson’s Disease
Relation Of The Neural Network Perspective To The Neuropathology Of Parkinsons Disease Dementia
At the neuropathological level the consensus from most studies to date is that the amount of Lewy-related pathology in neocortical and limbic areas is the most important factor in the development of PDD . However, the significance of Lewy-related pathology occurrence in particular cortical areas is debated, for example one retrospective autopsy study found that severity of cognitive decline in PDD correlated with Lewy-related pathology in the frontal and cingulate gyri , while another found no significant correlations in these regions but did find one in relation to temporal lobe Lewy-related pathology . Meanwhile some patients with Parkinsons disease with cortical Lewy-related pathology do not develop dementia at all . The significance of concurrent Alzheimer-type pathologies is hotly debated , although a recent study quantitatively assessing cortical Lewy-related pathology and Alzheimer-type pathologies found that a combination of both correlated most robustly with development of PDD . The relative contributions of other pathologies including microvascular disease, cerebral amyloid angiopathy, argyrophilic grains and TARDBP remain unclear .
What Are Parkinson’s Disease Dementia Medical Treatment And Medications
There is no specific therapy for dementia in Parkinson’s disease. Although cognitive symptoms initially may appear to respond to drugs that promote dopamine production, the improvement is mild and transient in contrast to the early responses to motor control improvement with medication in patients with Parkinson’s disease.
Parkinson’s disease dementia medications
Various medications are used to treat the movement disorders of Parkinson’s disease, some may exacerbate symptoms related to dementia.
- These include dopamine given in the form of levodopa; medications known as dopamine agonists that act on the dopamine receptor; and medications that slow down the metabolism of dopamine. They are often used in conjunction with monoamine oxidase inhibitors such as rasagiline. In addition, anticholinergic drugs are sometimes used.
- Unfortunately, these drugs may affect cognitive symptoms and mood disorders.
- The anticholinergic drugs, for example, help balance levels of dopamine and acetylcholine, another neurotransmitter, in the brain. These drugs can improve movement disorders but often make memory loss worse.
The dementia of Parkinson’s disease may respond to drugs used in patients with Alzheimer’s disease. However, these drugs, called cholinesterase inhibitors , lead to only small and temporary improvements in cognition.
Mood disorders and psychoses are usually treated with other medication.
Also Check: What Is Used To Treat Parkinson’s Disease
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinsons disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinsons disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinsons disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinsons disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinsons disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Caring For Someone With Parkinsons
Practice patience and understanding when dealing with Parkinsons. You may be very frustrated and challenged as a caregiver, but those with Parkinsons are just as frustrated. Their physical and mental conditions can be debilitating, depressing, and humiliating.
Diet and nutrition can have a huge impact on the health and comfort of a Parkinson patient. Eating well, getting more rest, sleeping well, fresh air, and exercise can make a difference. Getting the right medication and complementary therapies is also important.
As Parkinsons impacts a patients motor skills, modifications to the living environment may have to be made to accommodate wheelchairs and limited mobility issues. Professional in-home assistance for Parkinsons can allow Parkinson patients to remain independent and can enhance quality of life.
Most importantly, seek help and support from family, friends, and caregiving support groups. Take advantage of the resources in your community. Shouldering all the burden can take a toll on a caregiver.
Take care of yourself or you wont be able to take care of your loved one. Follow the preventive advice provided above for yourself as well, and take deep breaths!
Resources
Read Also: Who Diagnoses Parkinson’s Disease