Shake Off Your Stress
Freezing episodes are more frequent and intense when youre anxious. Anxiety leads you to tense up your hands, arms, shoulders and jaw which raises stress in your body and feeds your freezing, making you even more anxious! ;
To combat this vicious cycle, deliberately give your body a good shake before you start walking. Start with loosening and shaking your hands, arms, shoulders, neck and tongue. Take a deep breath, stay as relaxed as possible and set out towards your destination!
How To Manage Freezing In Parkinsons Disease
The patient with Parkinsons disease should keep certain points in mind-
Inform the Doctor: It is extremely important to let the doctor know when the patient encounters episodes of freezing in Parkinsons disease. The doctor may adjust the patients treatment protocol if need be.
Physical Therapy: The patient may ask the doctor about physical therapy as techniques in such a form of therapy help reduce the risks of falling occurring due to freezing.
Occupational Therapy: The doctor may recommend the patient to an occupational therapist. He can help patients with exercises that may help reduce stiffness and immobility.
Why Does Freezing Of Gait Occur
It is not completely clear why some people with PD experience freezing of gait and others do not. Research suggests that there is a relationship between freezing of gait and cognitive difficulties. The brain circuitry that controls gait is extremely complex and involves multiple connections between various parts of the brain, including:
- areas in the front of the brain that plan and initiate movement
- areas of the basal ganglia where the dopaminergic neurons that refine and control movement are found
- areas in the brainstem which modulate movement and wakefulness
Freezing of gait seems to be caused by short-lasting episodes of inhibition of these brain circuits that coordinate gait. The specific abnormalities that cause the problem may differ from person to person.
You May Like: What Are The Stages Of Parkinson’s Disease
The Difference In Stn Activity Between Pdfog+ And Pdfog
When delving into subcortical studies and LFP, an increased high-beta power was observed in the STN during the OFF state in PDFoG+. Levodopa administration was found to effectively reduce the high-beta power . In the study on the power coherence between the STN and EEG, beta-burst duration was longer in PDFoG+ compared with PDFoG during stepping in place and walking forward . In the bicycling and walking study, the greatest beta-band decrease was observed during cycling, indicating its potential therapeutic effect by matching the effects of DBS therapy . Finally, beta power was decreased during stepping without FoG and was proposed to indicate a compensatory mechanism adopted to overcome abnormal gait in PDFoG+. This study also explored sample entropy and found it to be at its greatest during forward walking. This indicated an error in the processing of subthalamic outflow, resulting in abnormal gait patterns . The vast variety of biomarkers and competing results are suggestive of the need for future research to follow similar paradigm and evaluation procedures. For findings to be significant, future research must agree on the way bands are segmented, i.e., beta into high and low bands. Also, to more closely match potential FoG event occurrences, more work must focus on actual lower limb task paradigms and the execution of protocols during ON vs. OFF medication states.
Treating Freezing Of Gait For People With Parkinsons

Freezing of gait episodes often occur when a person is under-medicated and can improve with increased amounts of their PD meds, usually carbidopa/levodopa. However, as mentioned earlier, the brain abnormalities that lead to freezing of gait are very complex, so giving more dopaminergic medication is only part of the solution. In fact, some people have what is referred to as ON freezing. This means that freezing of gait episodes occur even when other PD symptoms are well treated with their medication regimen.
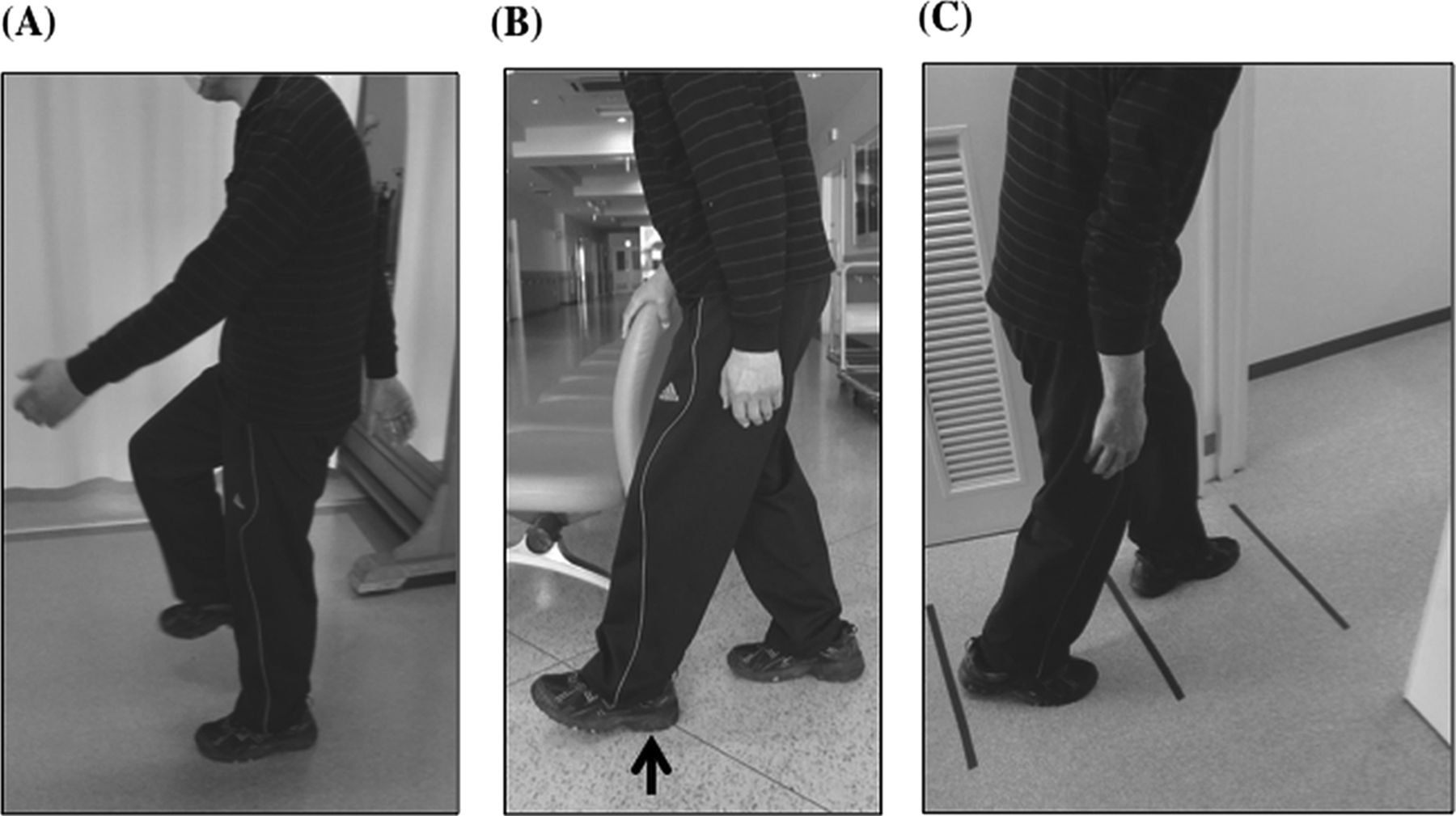
Cueing, or the introduction of an external sensory stimulus to facilitate movement, has been identified as a way to break a freezing episode. Terry Ellis, PhD, PT, NCS, Director of the APDA National Rehabilitation Resource Center at Boston University, and Tami DeAngelis, PT, GCS, compiled this list of cues that can be used to get out of a freezing episode:
You May Like: Can Parkinson’s Disease Cause Seizures
Balance And The Brain
Difficulties with balance and walking are linked to the brain changes that take place with PD. For people who dont have PD, balance is automatic, a reflex. But Parkinsons affects the basal ganglia . To compensate, the brain assigns another brain area an area used for thinking to take over. The thinking part of the brain, mainly the frontal cortex, cant control balance automatically. The result: for many people with PD, balance becomes less automatic.
This means that when people experience freezing and fall, they cant adjust their balance automatically. Taking small steps to try and regain balance can make things worse, because it involves shifting weight with each step. The brain changes from PD inhibit their ability to take a big step to catch their balance and avoid a fall. For some, the drug levodopa can help prevent freezing, but does not improve balance.
A person whose balance is less automatic must pay more attention while walking. For everyone, walking slows down when were talking and thinking slows down when were walking. This is called the dual-task cost and its higher in people with PD. That tells us that people with PD are using more attention and more cognitive control for balance and gait.
The Symptoms Of Parkinson’s Disease
Parkinsons Disease is a neurodegenerative disease, which means the symptoms can get worse over time. PD is also a very complex disease with both motor and non-motor symptoms, and the symptoms present differently in every individual. The most common symptoms of Parkinsons are discussed below. It is important to note that individuals with PD may not experience all of these symptoms, and symptoms will progress at a different rates in different people.
Also Check: What Medications Are Used For Parkinson’s Disease
Ways To Reduce Parkinsons Freezing Of Gait
Do you sometimes feel like your feet are stuck to the floor or your hips are glued to your chair, despite your best efforts to move them?
This symptom, called freezing, has been seen in 30-67% of people diagnosed with Parkinsons, with a higher rate of incidence in later stages.
While everyone has unique freezing patterns, some common triggers include: turning in tight spaces, walking through doorways, walking in narrow hallways or crowded places or changing walking surfaces .
As soon as you notice freezing symptoms creeping up on you, its important to address them so you can prevent them from worsening over time.
The first line of treatment is often dopaminergic medications that aim to keep you in an ON state for longer. However, evidence suggests there is a cognitive component of freezing that medication and deep brain stimulation do not address effectively.
This is why the best long-term treatment option for Parkinsons freezing is non-pharmaceutical, non-invasive and focuses on retraining your brain for success.
Here are six actions you can take to help minimize your freezing of gait.
What To Do When You Freeze Or Cant Get Started
If a movement isnt flowing well, making the effort to think about each separate part of a familiar or simple movement can help you get going.
If your feet freeze you may fall over so make sure that any family, friends and carers know about your freezing and know how to help when it happens.
The first thing to do when you feel yourself freeze is to stop moving, or to slow down. This gives you time to refocus on balance, think about your next move and prepare your body to start again, which can reduce any risk of falling.
The plan method
- STOP: calm yourself and take a breath.
- THINK: what do you want to do?
- PLAN: how are you going to do it?
- DO: complete the task or movement.
The weight shift method
- When you freeze, dont try to move forward straight away. Instead, gently move most of your weight to one leg . Shifting your weight to your one supporting leg like this will let you step forward with the opposite foot. To help with this count one, two, three, step or say ready, steady, go to yourself to get moving again.
- You may be able to re-start walking again by gently rocking your head and shoulders from side to side. This rocking can help you shift your body weight to your supporting leg.
- It may help to say something to yourself as you do this, like move my weight to left leg, then step with right . You may have to rock from leg to leg to release the weight on each foot before stepping off.
Sound and vision cueing methods
Using your imagination
Floor strips
Also Check: Is Parkinson’s A Fatal Disease
Rhythmical Or Auditory Cues
- A steady beat from a metronome or suitable music can help. The rhythm should be a comfortable pace, the beat prompting you to lift your feet and step.
- Develop a trigger word such as go, step or march to re-start your walking.
- Try closing your eyes to take the first step, making sure it is safe to do so, then open your eyes to continue walking.
- Hum a tune or download music with a good beat onto an MP3 player to keep your walking pattern going. Remember though that you should not use your MP3 in busy places where you should listen for traffic.
- The cue timing can be varied according to where you are, for example you will probably walk faster when outside, and slower in your home. See our video -;Coping Strategies: overcoming freezing by counting 1;and our video -;Overcoming freezing by counting 2.
- A physiotherapist or occupational therapist may be able to advise on mini metronomes or similar devices that can be clipped onto clothing so can be taken with you anywhere.
Attentional strategies use your imagination
The weight shift method
Start hesitation
Touch
- Touching a particular part of the body can also sometimes be helpful as a cue to unblock freezing see our video:;Coping Strategies: using touch as a cue.
Electrophysiological Signal Recording And Analysis
The subthalamic LFP recordings were combined with measures of the cortical electrophysiological activity using a 64-channel portable EEG . EEG signals were acquired with the sampling frequency at 1000 Hz and resampled at 400 Hz to match the STN LFP sampling frequency and optimize signals alignment for connectivity analyses. Low frequency and high frequency were eliminated using a bandpass Kaiser windowed FIR filter . Power line noise was eliminated using a bandstop fourth order Butterworth filter. EEG channels affected by bad scalp-electrode were visually identified and replaced with spherical spline interpolation. Stereotypical artefacts were removed by independent component analysis . Laplacian montage was applied to reduce muscular artefacts . We ruled out the effect of movement artefacts by comparing the wavelet transformation of epochs of walking with epochs of gait freezing, focusing on the 13 Hz band. In this frequency band, the epochs of walking and gait freezing showed similar spectral profiles, thus further excluding a confounding effect due to movement artefacts.
We first computed the power in the specific – and -frequency bands of the two STN and compared it between walking and the abovementioned time frames of gait freezing.
You May Like: How Soon Will There Be A Cure For Parkinson’s
What Freezing Is Like For My Dad
Like many Parkinsons patients, my dad notices that he usually only freezes when hes not on his medication. It usually happens while hes moving through doors: When you pivot youre worried about losing your balance. Thats why we shuffle our feet and take baby steps initially. Once Im moving Im fine, he says.
Since hes worried about maintaining balance while navigating, its possible that theres a connection between fear and freezing. Continuous motion seems to bypass the risk of freezing, while shifting motion types can present challenges.
Walking Aids To Help With Freezing Of Gait
Often freezing of gait cannot be overcome with medication adjustment and physical therapy, and a walking aid needs to be introduced for safety and walking support.
There are many types of walkers that are available for people with walking difficulties. Here is a simple guide:
- Basic walker this is usually just a metal frame without wheels
- Wheeled walker a metal frame with wheels. The wheels may be on two or four legs and the wheels may swivel or be fixed
- Rollator a walker with swivel wheels on all four legs and hand brakes. The brakes typically need to be engaged for the walker to stop. Often the rollator has a seat and a basket for convenience.
A common concern with all these walkers is that there either is no braking system or the braking system must be engaged in order for the walker to be stopped. Therefore, if a freeze occurs with the feet stuck to the floor, and the person is not fast enough to engage the brake, the walker will continue to move, potentially precipitating a fall.
Your physical therapist can help you determine the walking aid that is best-suited for your specific situation.
You May Like: What Is The Difference Between Tremors And Parkinson’s Disease
Demographic And Clinical Assessments
A total of 227 participants were recruited to the study; 147 of which were diagnosed with idiopathic PD and 80 healthy older adults . Of those with PD, 66 were classified as FOG+ and 81 were classified as FOG. Demographic and clinical assessments are shown in Table . When comparing OA and PD, there were no differences for age or gender but those with PD had a poorer MoCA score . When comparing FOG+ and FOG, there was no significant difference for age, gender or MoCA . However, motor disease severity, as measured by the MDS-UPDRS III, was significantly greater in the FOG+ group compared to the FOG group . The FOG+ group had significantly greater FOG severity, as demonstrated by the FOG ratio score compared to FOG .
Table 1 Demographic and clinical characteristics for controls, PD and PD without freezing and PD with freezing .
Differences In Eeg Between Pdfog+ And Pdfog
Table 1 summarizes the studies that focused on differentiating PDFoG+ vs. PDFoG for developing potential biomarkers. For PDFoG+ the LRP in EEG was shown to have an earlier onset and a larger magnitude during cognitive decision-making of target detection compared to PDFoG. These findings support the second mechanistic hypothesis, which states that dual-task-triggered FoG events are caused by the loss of automatic updating of motor programs by the dysfunctional BG . In terms of EEG frequency band analysis, the beta band was shown to increase in the frontal region during lower limb pedaling in PDFoG+, indicating preparatory adjustments and motor plan execution through top-down signaling . Also, for PDFoG+ theta band power was attenuated in the mid-frontal location, indicating an impairment in cognitive control . In the study that used the dual-task oddball paradigm, although the stimulus was detected by an increased P300, beta ERD was unchanged for PDFoG+. The inability of PDFoG+ to react to stimuli might have been caused by impairments at the BG. The BG impairments were suggested to be caused either by reduced input to the sensory-motor cortex or by the hypersynchronized thalamocortical activity. Additionally, the duration of beta ERS was found to be longer after the cue signal in the PDFoG+ compared with PDFoG .
Table 1. What differentiates PD with and without FoG?
Read Also: When Was Billy Graham Diagnosed With Parkinson’s
Coping With Freezing In Parkinson’s Disease
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology.
Around half of people who have Parkinson’s disease experience freezinga temporary inability to move that occurs suddenly and without warning. Such episodes are short-lived, lasting from a few seconds to up to several minutes.
Parkinson’s freezing can affect nearly any part of the body and disrupt nearly any activitychewing for example, or writing. However, it most often occurs when someone is walking, causing them to feel as if their feet are glued to the ground even though the upper part of their body is still mobile. This sometimes is referred to as freezing of gait and can have repercussions ranging from a brief disruption in stride to an increased risk of falling that can lead to broken bones and other injuries.
The exact physiological cause of freezing in Parkinson’s has yet to be determined. What is known is that it’s often associated with lulls in the effectiveness of medication, particularly among people who have mid-to-late stage disease. There also are a number of common triggers of freezing while walking, such as changing direction, approaching a doorway, or navigating a crowded area. Although Parkinson’s freezing can have a negative impact on a person’s quality of life, there are simple and effective ways to manage it.
Clinical Molecular Imaging And Biomechanical Data
Detailed demographic and clinical data are listed in . All subjects showed a sustained improvement from DBS , which was similar to the benchmark positive response from levodopa . This further supports the correct placement of the electrodes that were used for the recording of the STN neural activity.
In comparison with healthy controls, all patients showed a significant bilateral reduction of striatal DAT binding, with one hemisphere more dopamine-depleted than the opposite one . The average asymmetry index of the striatum was 27 . The H was contralateral to the clinically most impaired body side in each patient. The individual values of striatal DAT binding were previously reported for all patients except Patient nwk01 .
Biomechanics measurements showed reduced stride length and maximal velocity in subjects with Parkinsons disease with respect to healthy control subjects . All five subjects suffering from FOG showed gait freezing episodes during the study . We recorded 14 freezing episodes , clinically and biomechanically defined. All freezing episodes occurred while approaching a door .
Also Check: What Happens In Stage 5 Of Parkinson’s Disease
