What The Caregiver Can Do
- Encourage or help the patient with appropriate skin care after using the bathroom. Use warm water and pat the area dry.
- Help the patient keep a diary that records specific foods or drinks that may affect how frequently the patient goes to the bathroom.
- Help the patient maintain a bladder or bowel plan.
- Encourage the patient to go to the bathroom at consistent time frames during the day, like after a meal.
- Encourage regular daily exercise, as permitted by the health care team.
How Might Parkinson’s Affect The Bowels
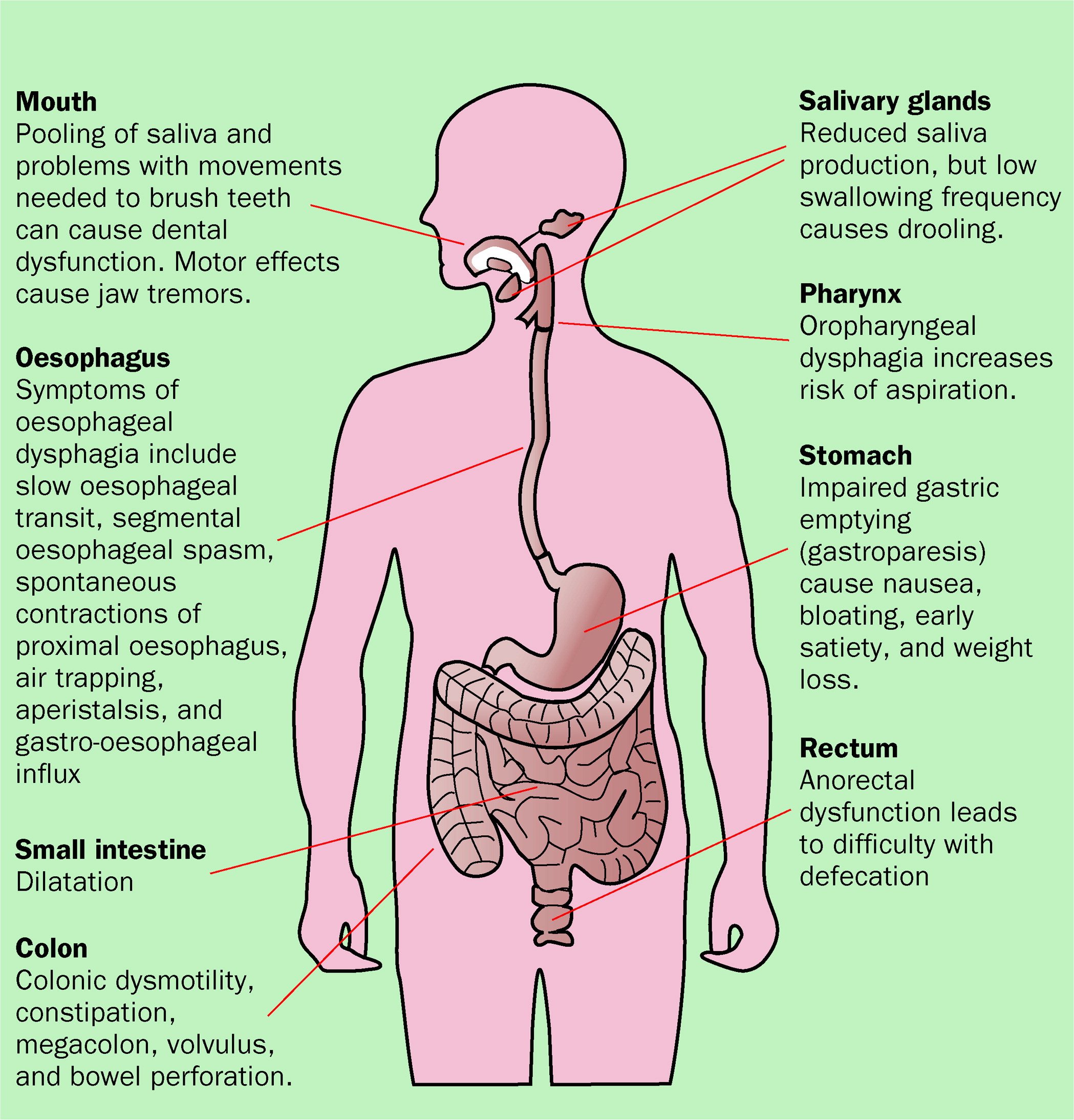
Bowel problems can occur in anyone, but some problems, especially reduced bowel movement or constipation, are particularly common in Parkinsons. This tends to be as a result of slowness of movement and muscle rigidity, both of which are visible symptoms of the condition. But Parkinson’s also muscles we cannot see including the bowel muscles – which in turn causes a reduction or slowness of bowel movements.
Poor bowel function may be exacerbated if chewing and swallowing food is difficult, which is quite common in Parkinsons. This may make it harder to eat a diet that is rich in fibre – for example fruit, vegetables and whole grains which helps form soft, bulky stools and aids bowel function.
Exercise is also thought to play a role in efficient bowel function, but if Parkinson’s makes activities more difficult, the bowel may be less stimulated and the intestines can become sluggish.
Constipation is thought to affect up to 65% of people with Parkinson’s the bowel symptoms may predate the neurological ones . Tremor and a fear of spilling drinks can mean some people unintentionally reduce their fluid intake which can make stools hard and more difficult to pass. When stools remain unpassed for a long time, they become harder as the body absorbs more water from them. If stools build up in the rectum they can become impacted and block the rectum. They may also overflow as lumps of stool or watery mucus.
Parkinsons Disease And Your Bladder
Many diagnosed with Parkinsons disease experience urinary tract issues. A Michigan Medicine urologist discusses treatment options for patients to consider.
Anne Pelletier-Cameron, M.D., often jokes to her patients that shes a female plumber of the lower urinary tract. On a more professional note, however, shes a urologist in the Michigan Medicine Department of Urology.
In this role, Pelletier-Cameron treats patients with a variety of lower urinary tract symptoms. Some of her patients have been diagnosed with Parkinsons disease, a progressive nervous system disorder that impacts movement. But the breakdown of nerve cells that characterize Parkinsons disease can also cause non-movement symptoms, including bladder issues.
Half of all women and 17% of men will experience urinary incontinence, or the inability to hold urine, she says, noting that for Parkinsons disease patients, those numbers escalate.
Many of my PD patients end up having other bladder problems, including issues with urgency and frequency, says Pelletier-Cameron. Nocturia, or the need to urinate many times during the night, is also common, along with difficulty in emptying the bladder.
The bladder is very complicated, says Pelletier-Cameron. It needs to be big enough to store urine so you can go about your life without having to empty your bladder every 10 minutes. It also needs to store urine at low pressure and squeeze at the right time to make sure the urine doesnt back up to the kidneys.
Don’t Miss: Does Parkinson’s Disease Run In Families
Treatment Of Sexual Dysfunction In Pd
4.4.1. Male Sexual Dysfunction
Dopaminergic Drugs
It is possible that levodopa and other antiparkinson medication may affect sexual function in PD. However, it is not entirely clear to what extent levodopa ameliorates sexual dysfunction in PD. In contrast, subcutaneous apomorphine injection is used to ameliorate fluctuating symptoms in PD. It has also been used to treat erectile dysfunction in the general population and in patients with PD , although the dose is different . Apomorphine is thought to stimulate dopamine D2 receptors, and activate oxytocinergic neurons in the PVN. Nausea is a common side effect of this drug. Cabergoline and pergolide are also reported to improve sexual dysfunction in PD. In contrast, pathological hypersexuality may occur together with or without delirium , which is attributed to the dopamine dysregulation syndrome in this disorder. DBS in the STN has produced either improved sexual wellbeing or transient mania with hypersexuality in patients with PD.
Phosphodiesterase-5 Inhibitors
When dopaminergic drugs did not help, phosphodiesterase-5 inhibitors, for example, sildenafil, vardenafil, and so forth, become the first line treatment in PD . These drugs inhibit nitric oxide degradation and facilitate smooth muscle relaxation in the cavernous tissue. When treating PD patients with postural hypotension, these drugs should be prescribed with extreme caution .
Other Drugs
4.4.2. Female Sexual Dysfunction
Thanks For Signing Up

We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Also Check: What Are The Symptoms Of End Stage Parkinson’s Disease
Bowel Incontinence: Another Embarrassing Casualty Of Pd
Fecal Incontinence is where you lose control of your bowels. This blog post explains the primary cause of this in Parkinsons disease. Problems reaching the toilet in time because of mobility, abdominal bloating or cramping compound the problem. Dr. De León has included a check list of things to help minimize occurrences and embarrassment, even to the point of surgery, if necessary.
Causes Of Constipation In Parkinsons Disease
The ways in which Parkinsons disease can increase the risk of constipation include:
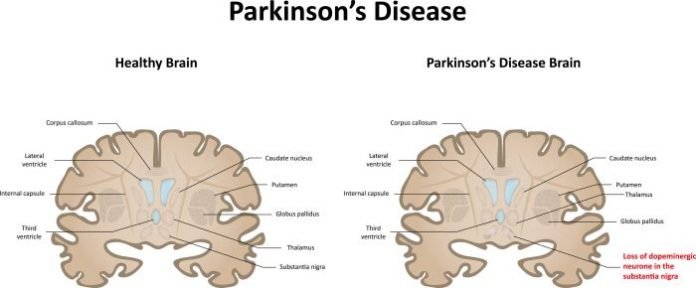
- lack of dopamine in the brain impairs control of muscle movement throughout the body. Bowel muscles can become slow and rigid
- uncoordinated bowel motions the bowel muscles may be weak and unable to contract, or they may clench instead of relaxing when trying to pass a motion
- eating problems dietary fibre containing insoluble fibre adds bulk to your bowel motions and can help prevent constipation. However, if a person with Parkinsons disease finds it difficult to chew or swallow, they may avoid eating fibrous foods
- drinking problems you need water to plump up the dietary fibre in your bowel motions. Swallowing difficulties may discourage a person with Parkinsons disease from drinking enough fluids
- sedentary lifestyle lack of exercise slows the passage of food through your intestines. Parkinsons disease reduces muscle control, so lack of exercise is common
- medications many different medications can cause constipation. Medications used in the treatment of Parkinsons disease may slow bowel movements or cause a decrease in appetite.
Don’t Miss: When Was Ozzy Osbourne Diagnosed With Parkinson’s
Hypothalamic Neurons And Dopamine In Men
Among the 3 types of erection, reflexive erection requires an intact sacral cord, particularly the intermediolateral cell columns. Pathology studies have shown that involvement of the IML nucleus is common in MSA, whereas it is uncommon in PD. Therefore, reflexive erection can be affected in patients with MSA. In patients with a supra-sacral spinal cord lesion, reflexive erection might be preserved, whereas psychogenic erection is severely disturbed because of a lesion in the spinal pathways to the sacral cord. Libido and erection are thought to be regulated by the hypothalamus; particularly the medial preoptic area and the paraventricular nucleus . Electrical or chemical stimulation in the MPOA/PVN evoked erection and mating behaviors in experimental animals, both of which were abolished by destruction of these areas. Somatosensory inputs from the genitalia ascend in the anterior spinal cord, and project to the MPOA/PVN via the thalamic nuclei. Erotic visual inputs from the retina are thought to reach the MPOA via the mamillary body. Recent neuroimaging studies have shown that penile stimulation or watching pornography activated these areas in humans . NPT seems to be regulated by the hypothalamic lateral preoptic area .
Urinary Problems In Parkinsons Disease
Parkinsons disease has many features that have little or nothing to do with movement. Among these non-motor symptoms are problems with the autonomic nervous system the part of the nervous system that controls automatic bodily functions, such as heart rate, blood pressure, sweating, sexual function and both gastrointestinal and urinary function. These symptoms are often among the most serious and complex issues faced by people with PD.
Unlike bowel dysfunction , which often occurs before Parkinsons movement symptoms, urinary dysfunction is not typically a problem until the later stages of the disease.
Recommended Reading: Is Parkinson’s Disease A Mutation
Treating And Managing Bowel Problems
The first step in dealing with bowel disorders is to talk to your doctor. He or she will probably review your medication to see if this is a contributory factor. Whilst it is usually possible to control any difficulties with diet, fluid intake and exercise, your doctor, or Parkinsons nurse specialist if you have one, will be able to advise further, and may, for example, prescribe laxatives in severe cases of constipation. If you have any alarm features such as unintentional weight loss or rectal bleeding, then you may need to be referred for specialist assessment.
The following healthcare professionals can also advise on aspects of bowel care:
- A dietician will be able to advise on diet and fluid.
- A physiotherapist may be able to help with advice and abdominal exercises which will help in passing stools.
- A speech and language therapist can help with swallowing problems. They may be able to advise on ways of relaxing your throat, and give guidance on posture and exercises to help overcome any difficulties you have.
- An occupational therapist may also be able to suggest practical ways to overcome any difficulties you have with eating and drinking.
What’s Next For Those Suffering From Urinary Incontinence
I decided I did not want to add another medication to the medicine bag. I was trying to see if there was something I could do besides resigning myself to wearing pads or some other incontinence protection all the time. At 53 years old, I wanted to see if there was a way I could help myself.
Part 2 of this article will address my experiences. I plan to discuss what I lovingly refer to as “PEE PEE PT” – physical therapy to help treat urinary incontinence.
Recommended Reading: What Toxins Can Cause Parkinson’s Disease
Why Worry About Weight Loss Associated With Pd
Weight loss has been linked to a poorer quality of life and more rapid progression of PD. The reasons for this are two-fold. On the one hand, as outlined in the list above, weight loss can be a hallmark of advancing disease as it could be a consequence of more swallowing difficulties, worsened mobility, more impaired gut function etc.
On the other hand, having weight loss can further lead to poorer health. Inadequate food intake can contribute to malnutrition and vitamin deficiencies. Malnutrition can subsequently be the cause of increased susceptibility to infection, increased fatigue and increased frailty. The situation can spiral with more fatigue and frailty causing a further decrease in activity and function.
Osteoporosis, or porous and fragile bones, is more common in under-weight people since bone structure is dependent on weight-bearing. Since osteoporotic bones are more prone to fracture during a fall, this too can be a contributor to more disability and frailty. Bottom line is that it is important for your health to maintain a healthy weight.
Urinary Issues In Advanced Parkinsons Disease
Always remember that people with advanced PD may have other medical problems that affect their urination such as an enlarged prostate. Make sure to have a complete evaluation before assuming that the problem is only related to PD. It is also essential to keep in mind that if changes in urination occur suddenly, there could be a urinary tract infection present.
What Examinations May I Need To Have
Your GP or specialist will probably ask a series of questions to find out what the problem is. These may include:
- When did the trouble start?
- How often does it happen?
- Can you feel when your bladder or bowel is full?
- Are you having difficulty emptying your bladder or bowel?
- How often are you using the toilet?
Parkinson’s symptoms, such as slowness of movement and rigid muscles, affect the muscles in the bowel wall. This can make it harder to push stools out of the body. You may be asked to keep a chart for several days of how often you use the toilet and how much you drink.
You may also be asked for a urine sample to test for infection and they will normally carry out a physical examination.
Bladder or bowel problems can be complex in Parkinson’s, so sometimes specialist tests or X-rays may be needed. All of these can usually be done in an outpatient department or clinic.
Read Also: What Is The Latest Treatment For Parkinson’s Disease
What Are They Wearing
Although you should allow someone with Parkinsons Disease to assert their individuality, you can ensure they are not wearing awkward clothing. Unnecessary zips and buttons on clothing can make it difficult to remove clothing in time, resulting in leakages. Try and encourage them to wear simple clothing that is fast and efficient to remove.
How Can I Help Myself
It is easy to become obsessed with bowel activity, but it is not necessary to have a bowel movement every day it can be quite normal for some people to empty their bowels only three or four times a week. What is important is that passing stools does not cause pain or unnecessary strain. Focus on what is normal and healthy for you and remember that bowel activity is affected by food and exercise, so will vary according to what you are eating and doing.
Remember that learning to manage your bowels will take time and patience, so dont expect to solve problems overnight. It may take a few weeks to adjust diet etc, so be patient. There are also plenty of ways you can help yourself.
Don’t Miss: How To Donate To Parkinson’s Research
Dietary Fibre For Constipation In Parkinsons Disease
Be guided by your doctor, but general suggestions include:
- Choose easy-to-eat fibrous foods such as soft fruits. Consider mashing or pureeing fruits to make them easier to eat. Make sure to include the skin, where most of the fibre is found.
- Eat at least two pieces of fruit and five serves of vegetables every day.
- Eat homemade vegetable soups.
- Sprinkle a tablespoon of bran, psyllium husks or chia seeds on your breakfast cereal or add the bran to baked products such as cakes. However, avoid bran if you have swallowing problems.
- Fibre supplements may be helpful, but you must drink enough fluids for these to work properly. Avoid fibre supplements if you have problems swallowing.
- Dont increase dietary fibre too quickly or youll risk bloating and abdominal cramps. If discomfort occurs, cut back your fibre intake, increase your fluid intake, apply a hot water bottle to your abdomen and see your doctor.
Toilet Habits And Constipation In Parkinsons Disease
Suggestions for good toilet habits include:
What Can You Do About Weight Loss Associated With Pd
If you do find yourself unable to maintain a healthy weight, discuss this with your doctor. The good news is that after a medical workup, he or she may suggest one or more of the following steps that can help you:
Tips and takeaways
Do you have a question or issue that you would like Dr. Gilbert to explore?
Dr. Rebecca Gilbert
APDA Vice President and Chief Scientific Officer
Addressing Practical Aspects Of Eating And Drinking
Bladder Incontinence In Women
Bladder incontinence is more common in women than in men. Other than the possible causes listed above, some things that may increase risk of bladder incontinence in women are:
- Changes to urinary or vaginal tissue from hormone therapy, surgery, chemotherapy, or targeted therapy
- Hormonal changes from menopause
- Pelvic prolapse – the bladder, uterus, and or rectum may slip backward or downward into the vaginal canal because of weak pelvic wall muscles
- Pregnancy
- Hysterectomy
Read Also: What Is The Difference Between Essential Tremors And Parkinson’s
Bowel Issues In Parkinson’s
Recently, I was doing an interview about Parkinsons troublesome issues and I had to admit that by far my most troublesome and annoying problem is related to the effects of my gut. This is true for the majority of us living with this disease. Whether it be a direct or indirect consequence of our illness is irrelevant in my opinion when the effect is the same. Plus to be honest I am not sure anyone of us can tell the difference most of the time.
As I have re-discovered the agony of suffering from one of these ailments over the last several months when I had several bouts of ileus. In my opinion, there is nothing worse than having stomach pain, bloating, nausea, indigestion, and gas to make life miserable.
Below are all the plausible GI symptoms all of us can experience throughout our journey with PD.1 The most common symptoms are those related to poor motility or dysmotility and can be compounded by the effect of the medication.
Does Parkinsons Cause Incontinence
I have recently been diagnosed with Parkinsons Disease and am shocked to see I am experiencing heavy leaks..during the day AND night. Im finding it difficult to know when my bladder is full, which is leading to urine overflowing during the day!! I wasnt told this would happen!! I am new to this.. what do I do?? How do I choose a product? Im not sure I want to talk to a Doctor and would rather get an answer on here. Im a 50 year old male.
ll Edward,
Parkinsons Disease is a common cause of incontinence. Bladder problems occur due to Parkinsons affecting the nerves that control bladder emptying. Parkinsons can also affect your ability to reach the toilet quickly before leakages. Painkillers commonly used for Parkinsons such as codeine and anticholinergics prescribed for tremor can even cause incontinence.
You describe your leaks as heavy, therefore more protection is needed for you than an incontinence pad. Either protective pants or an all-in-one brief will be suitable for you. Belted all-in-one products are ideal if you are less mobile or immobile and would like a product that is easy to put on and off. They have velcro fastenings for fast removal and will keep you dry for longer than other product options.
You can read our blog on overflow incontinence symptoms for more information on the condition.
Take care and do not hesitate to ask other questions!
Also Check: How To Avoid Parkinson’s Disease
Neurologic Disease Or Injury
The main functions of the colon and anorectum are to mix and absorb water from ingested material, to store fecal wastes, and to eliminate them voluntarily at a suitable time. A wide variety of neurologic diseases can affect colonic and anorectal function and are associated with constipation and or fecal incontinence. Examples include:
- Multiple Sclerosis
- Spinal Cord Injury
- Parkinsons Disease
Neurological diseases can affect nerve pathways to the large intestine. They can also affect the nerve network within the bowel wall that regulates intestinal smooth muscle, a type of muscle that functions automatically without direct voluntary control. This article summarizes what is known about these conditions and how best to manage constipation and incontinence associated with these disorders.
Study Reveals Ibs Risk

BERLIN — Irritable bowel syndrome may be a more frequent symptom in Parkinson’s disease than constipation, researchers reported here.
In a case-control study, about a quarter of Parkinson’s patients had IBS compared with only 5% of healthy controls , according to Tuomas Mertsalmi, MD, of the University of Helsinki, and colleagues.
On the other hand, the prevalence of constipation was higher among Parkinson’s patients, but the difference from healthy controls wasn’t significant, they reported at the Movement Disorders Society meeting here.
“Gastrointestinal symptoms in Parkinson’s disease are more complex than just constipation,” Mertsalmi told MedPage Today. “Usually constipation is just seen as decrease bowel frequency, but it is also about straining during defecation, hard and lumpy stools, and diarrhea in these patients.”
Previous work has shown that the majority of patients with Parkinson’s suffer from gastrointestinal symptoms. About 70% have been estimated to have constipation, which is considered to be a premotor symptom of the disease and is one of the strongest risk factors for Parkinson’s, Mertsalmi said.
IBS is among the most common functional gastrointestinal disorders, and is characterized by symptoms of abdominal pain or discomfort, and alteration of bowel habits.
All patient with a pre-existing diagnosis of IBS were excluded, he added.
Disclosures
Don’t Miss: Can Yoga Help Parkinson’s Disease
Treatment Of Bladder Dysfunction In Pd
2.4.1. Dopaminergic Drugs
It is possible that levodopa and other antiparkinson medication may affect bladder function in PD. Aranda and Cramer studied the effects of 38mg apomorphine injection on the storage function in 2 de novo PD patients, and found that the bladder capacity increased. They gave oral levodopa to one of the patients, and the bladder capacity increased. We compared the frequency of bladder dysfunction in de novo PD and PD with levodopa. In that study, LUTS was less frequent than in the treated group . In another study, after 3 months of treatment with levodopa, the storage urodynamic parameters were slightly improved in de novo PD .
2.4.2. Cholinergic Drugs
Anticholinergics are generally used as a first-line treatment for overactive bladder. However, it is important to balance the therapeutic benefits of these drugs with their potential adverse effects. When the dose of drug increases, postvoid residuals may appear . Dry mouth and constipation are common . Cognitive adverse events by anticholinergics are a concern particularly in the elderly. For example, trihexyphenidyl and oxybutynin have been shown to have central side effects . Factors contributing to the central effects of drugs may include blood-brain barrier penetration . Among the factors of BBB penetration, diffusion is facilitated by lipophilicity . Particularly in elderly patients who have hallucinations or cognitive decline , anticholinergics should be used with extreme caution.
Bladder & Bowel Issues
Bladder and Bowel Problems
Bladder and bowel problems are common to people of all ages in the general population. People with Parkinsons disease are more likely to suffer from some of these problems, particularly constipation. The problems which can affect people with Parkinsons are discussed in this leaet.
You should tell your GP, Consultant or Parkinsons Disease Nurse Specialist about your problems and they will be able to provide advice on any additional support available to you.
Bowel problems
The most common bowel problem in Parkinsons is constipation. Other problems which can occur include diarrhoea and leakage due to a weak anal sphincter.
Constipation is the number one reason why a persons Parkinsons has become suddenly worse the levodopa medications used to treat Parkinsons are absorbed by the bowel, so if it is lled to capacity, you are unlikely to get the full benet from these drugs.
Constipation
Also, people with Parkinsons often have a delay in gastric emptying, meaning that the contents take longer to leave the stomach and enter the bowel. This is another reason to ensure levodopa medication is taken without food.
Another cause of constipation is the medication itself levodopa medication can cause constipation, so it is essential that you monitor your bowels, and manage a sluggish bowel.
Inadequate uid intake or dehydration will result in stools being hard and difcult to pass. Fibre helps form soft bulky stools that are easy to pass.
Don’t Miss: Does Stress Cause Parkinson’s Disease
Toilet Habits And Constipation In Parkinsons Disease
Suggestions for good toilet habits include:
- Go to the toilet as soon as you feel the urge to pass a bowel motion. Hanging on can contribute to constipation.
- Use the correct posture on the toilet to help you pass a bowel motion place your elbows on your knees, bulge out your stomach, straighten your spine and put your feet on a footstool.
- Avoid holding your breath and dont strain when you are on the toilet. Allow yourself plenty of time.
- Use a warm washcloth pressed against your back passage or gently massage with one or two fingers to help to relax the muscles.
- Talk to your doctor or pharmacist about medicines to help soften your bowel motions.