Bringing Light To Darker Side Of Parkinsons
Often the hardest part of Parkinsons disease psychosis is the fear of the unknown. As a person with Parkinsons, you may worry about having hallucinations and/or delusions and not being able to do anything about it. As a care partner, you may worry that you wont be able to help your person with Parkinsons feel safe if something does happen.
The good news is you now have information on what Parkinsons disease psychosis is; the risk factors to look out for; biological and environmental triggers that can bring them on; and how to manage them if they show up.
But what about the emotional toll these types of symptoms can place on you over the long-term as the person with Parkinsons or as a care partner?
The diagnosis of a chronic illness in and of itself requires a lot of adjustments. When you add something like Parkinsons disease psychosis into the mix, its important that you also add another level of self-care to your everyday life.
Emergencies With Prominent Aggravation Of Parkinsonism Or Dyskinesias
Severe parkinsonism and generalised hyperkinesia are common in people with Parkinsons disease. These disabling motor syndromes usually develop in advanced disease, manifesting as prominent fluctuations associated with chronic levodopa therapy. Motor complications are usually managed initially in an outpatient setting but if severe may need hospitalisation. Rare cases can progress to fever and rhabdomyolysis, resembling neuroleptic malignant syndrome, and requiring intensive care unit treatment.
Illustrative Case Of Parkinsonism
A 73-year-old man with a 15-year history of Parkinsons disease was admitted for neurosurgical evacuation of traumatic subdural haematoma. His parkinsonism had deteriorated in the last 3 months despite high daily levodopa dosage . During the postoperative period, his bradykinesia and rigidity markedly worsened. There was no clear improvement despite increasing the levodopa in combination with dopamine agonists in several presentations . He became confused, febrile and diaphoretic. On examination, he had marked generalised rigidity and bradykinesia. CT scan of head was normal. Other factors that may aggravate parkinsonism, such as addition of dopaminergic blockers, and concurrent medical conditions, were ruled out. Blood tests showed high muscle enzyme levels and markers of acute renal failure. Response to dopaminergic therapy remained minimal. He later developed shortness of breath and tachycardia. Pulmonary embolism was diagnosed and he was admitted to the intensive care unit. Levodopa was administered via a nasogastric tube and intense physiotherapy implemented with gradual improvement of his health status although daily functioning was still significantly impaired despite continuous dopaminergic therapy.
-
Learning points: Risk and contributor factors to develop parkinsonism-hyperpyrexia syndrome; benefit of nasogastric levodopa administration in cases with an inappropriate oral intake; the relevance of paying attention to systemic complications.
Communicating With Your Doctor
Unfortunately, fear, embarrassment, or stigma can cause people not to share symptoms of Parkinsons psychosis with their health care providers. Its important to tell your doctor if you experience hallucinations or delusions, so you can discuss possible solutions.
Your doctor can help determine the cause of hallucinations and delusions. They may be caused by an infection, like an urinary tract infection, or they could be a side effect of a treatment for an unrelated condition. Hallucinations and delusions can also be an indication of another medical condition, such as dementia with Lewy bodies. Dementia with Lewy bodies is a movement disorder that can be difficult to distinguish from Parkinsons disease.
Whatever the cause, your doctor can recommend treatments or strategies to help you and your family better deal with episodes of psychosis. One member shared tips from her husbands doctor: According to his neurologist, you should always be honest. His neurologist coaches him to listen to me because I am looking out for his best interests, and I will not lie to him about what is real and what is not. He seems content with that.
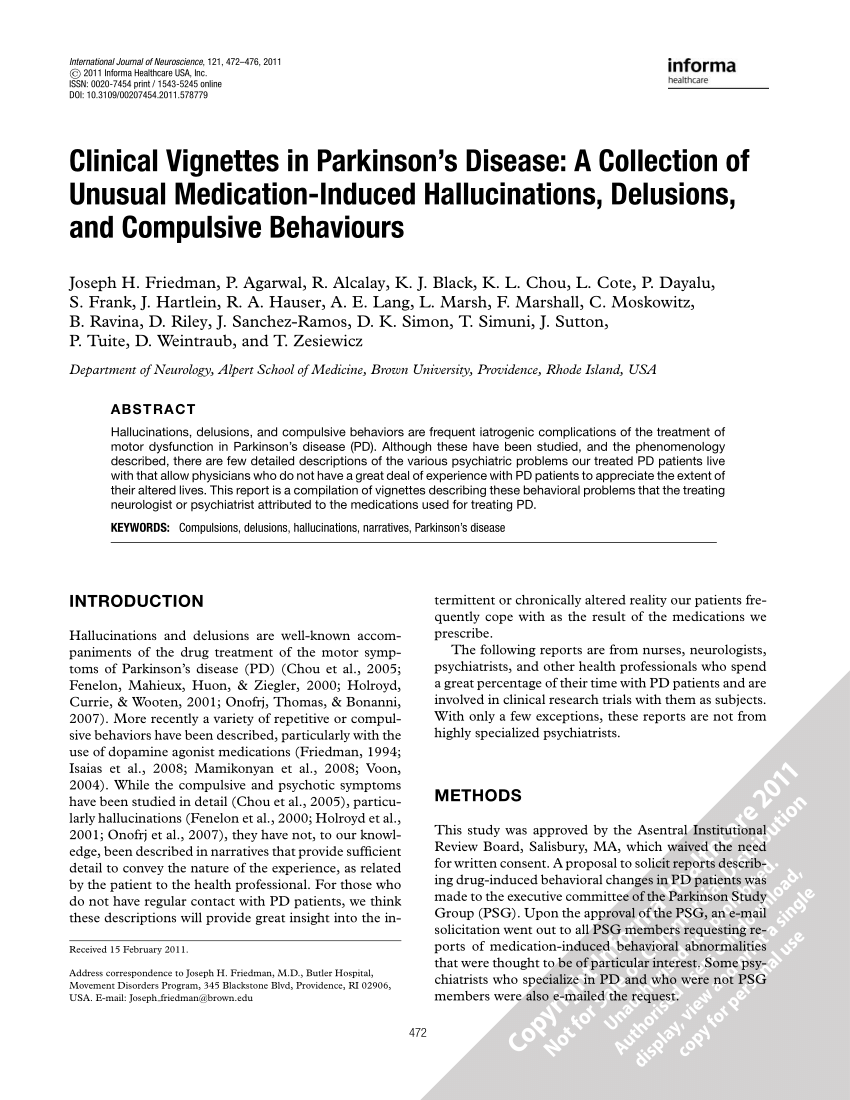
Treatments That Can Cause Psychosis
Dopamine therapies and anticholinergics are treatment types that can lead to hallucinations and delusions. If you or a family member are experiencing symptoms of Parkinsons psychosis, your doctor may recommend adjusting or discontinuing medications in these classes.
Dopamine Therapies
Hallucinations and delusions can be a side effect of dopamine therapies. Parkinsons disease develops when the brain cannot produce sufficient dopamine, a neurotransmitter that controls movement and emotions. Dopamine therapies, also referred to as dopaminergic drugs, work by increasing dopamine levels in the brain. Some dopamine therapies work by converting the brain chemical levodopa to dopamine, and others mimic dopamines effects in the brain .
Anticholinergics
Anticholinergics reduce the levels of acetylcholine a neurotransmitter that helps regulate motor functions. Hallucinations can be a side effect of these medications, especially for people over age 70.
Help For Families And Caregivers
Wanting to correct the notion of imposters can be frustrating and upsetting for caregivers as well as those experiencing the delusions. Delusions are fixed, unfounded beliefs; attempts at making corrections, sometimes called reality orientation, tend not to be effective. For caregivers, learning to accept that those with CS are not malicious is helpful to accepting the condition. Vilayanur S. Ramachandran, PhD, known for his work in behavioral neurology and visual psychophysics, says the lack of visual recognition can be terrifying for someone with CS. Validation theories whereby caregivers acknowledge the delusions as truths but provide reassurance that the imposters are not harmful, is an approach to constructive care.4
Practical Tips For Caregivers Of People With Parkinson’s Psychosis
This 2-page tip sheet has bullet point suggestions for what to do if the person you care for experiences hallucination, delusions or confusion, or becomes agitated or aggressive. In addition, there are tips for how to best be prepared for a doctors appointment when you bring this behavior to the attention of your medical team.
What Is Capgras Syndrome
A delusional misidentification syndrome , Capgras causes disruptions in the brains facial recognition system. These delusions have a person thinking someone close to them, a spouse, parent, close friend, or family member, has been replaced by an identical-looking impostor.2
Although relatively uncommon, Capgras is associated with neurodegenerative disorders including Parkinsons and Lewy body dementia .3 Anyone caring for someone with these conditions has likely experienced the stressful ups and downs of caregiving. As a caregiver, a reward can be signs of love and appreciation from the person being cared for. In the case of Capgras, this recognition may be missing because of the strong visual confusion experienced by people with CS. Their loss of recognition and lack of emotional response can be painful.
How Can You Improve Aggressiveness And Hallucinations In Parkinsons
Hallucinations may spark anger or aggression in a person with Parkinsons disease. Some ways to help include:
- Reassure them, tell them they are safe.
- Speak slowly and calmly.
- Ask questions about the persons feelings.
- Listen to the person, dont interrupt.
- Avoid sudden movements.
- Give the person space and a way out, so they dont feel cornered or threatened.
- Make an emergency plan ahead of time for what you and others in the house will do if the person experiencing hallucinations becomes a danger to themselves, you, or anyone else.
- When it is safe, help the person speak with their healthcare provider about making a plan to address the hallucinations.
Treatment And Management Of Hallucinations
You should discuss any hallucinations or delusions with your doctor, or Parkinsons nurse if you have one, so that all treatment options can be considered.
In mild cases no specific action may be required and simple reassurance that the images, sensations or sounds are harmless may be all that is needed.
Reacting In The Moment
It can be hard to know how to respond to a hallucination or delusion while its happening. A member described a friend with delusions: She believed that up to 10 children come and stay in her house, and she is responsible for their care. I didnt know whether to tell her they are not real or just go along with her.
The right response will vary, depending on the person and the particular circumstances. In all cases, doing your best to remain calm and patient will go a long way to helping manage the situation.
If a person is hallucinating but has insight, you can explain that the hallucination isnt real. I just talk with him about what he is seeing and then show him that nothing is there. I never try and pretend what he sees is real, a spouse on MyParksinsonsTeam commented. Another caregiver wrote, If his hallucinations are during the day, I will tell him he is hallucinating and ask him to show me where or what is the problem. That way he ends up seeing there is nothing there.
If the person has lost insight, it may be better not to challenge their reality. Instead, you can offer a distraction, move to another room of the house, or start a new activity. One caregiver explained, If it is the middle of the night and he wants to get dressed and go to work, I generally ask him to come and sit with me first so I can go to sleep.
Strategies To Prevent Complications
Prompt diagnosis and intervention are the basis to guarantee a good prognosis for most complications. It is important to note that medication changes cause the large majority of these problems.
Based on the quality standards for Parkinsons disease published by the National Institute for Health and Care Excellence and the American Academy of Neurology, we suggest several measures for preventing or, at least, minimising serious complication in Parkinsons disease .
Treating Psychosis That Can Accompany Parkinson’s Disease
Although treatment options are limited, physicians must learn to recognize and effectively treat Parkinson’s psychosis.
A new medication may soon be available to treat the hallucinations and delusions that often accompany Parkinson’s disease. “It shows promise in improving the hallucinations without worsening the motor functions,” says Jennifer G. Goldman, MD, an associate professor of neurology at Rush University Medical Center in Chicago.
She explained that, to date, good medications for treating Parkinson’s psychosis have been unavailable. “It would be very exciting to have another agent available to use,” she says.
Parkinson’s Psychosis People who have Parkinson’s disease may develop psychosis, possibly as a result of the medications used to treat the movement disorders but also possibly related to the disease itself. These misperceptions can range from illusions, such as a chair looking like a dog, to false beliefs, perhaps of an unfaithful spouse or an imaginary person living in the house, Goldman explains.
The hallucinations are primarily visualone of the many differences between psychosis symptoms in Parkinson’s and those in schizophrenia. With schizophrenia, people might have delusions of grandeur, believing they have unreal abilities, or they might hear voice commands. With Parkinson’s psychosis, Goldman explains, auditory hallucinations are infrequent and if they arise, generally are confined to background noise, such as children or music playing.
Parkinsons Disease Psychosis: My Husbands Frightening Symptom
Photo Courtesy of Diane Sagen
More than 50 years ago, I married the love of my life, Jay. We started a family and built a wonderful life together in Southern California. Jay, an artist, was a professor of art at several community colleges and painted in his spare time.
Things had been going wonderfully for us. But in 2009, I began to notice that Jay wasnt himself. His hands would shake, and he had trouble concentrating at work. Challenged by grading papers and maintaining his focus in class, he eventually retired, possibly sooner than he might have otherwise.
It was at this time that Jay was diagnosed with Parkinsons disease, which changed our lives and altered the course of our future together.
Hallucinations Delusions And Parkinson’s
It is estimated that about 50% of people with Parkinsons will, at some point, experience hallucinations. They can affect younger people but are more often associated with those who are older and have had Parkinsons for some time.
Hallucinations experienced early in Parkinsons may also be a symptom of the condition dementia with Lewy bodies so it is important to let your doctor know if hallucinations begin at an early stage.
Parkinsons itself can be a cause of hallucinations and delusions, but very often they are a side effect of certain medications used to treat the condition. Not everyone who takes Parkinsons medications will experience hallucinations and delusions though. This varies from person to person and is often related to the particular type of medication and dosage.
Other factors may also be involved such as underlying illness, memory problems, sleep difficulties and poor eyesight.
What Causes Parkinsons Disease Psychosis
Parkinsons is a brain disorder associated with a loss of dopamine-producing nerve cells deep inside the brain. Dopamine is a neurotransmitter that helps regulate the bodys movement, and it also allows us to think clearly and regulate our emotions. When you try to replace the dopamine thats been lost in a person with Parkinsons, it can cause the system to get out of whack which can impact thinking, how visual things are processed and more. Parkinsons disease psychosis is therefore typically a side effect of the disease itself or the medications used to manage it.
As a result, its an ongoing balancing act for Parkinsons doctors to prescribe enough dopamine to control a person with Parkinsons motor symptoms, but not so much that the person experiences hallucinations and/or delusions.
Medications Used For Treating Psychosis
Antipsychotic agents are designed to balance abnormal chemical levels in the brain. Up until the 1990s, the use of antipsychotics in PD was controversial because the drugs used until that time work by reducing excess dopamine. This alleviated psychosis but caused dramatic worsening of PD motor symptoms.
Fortunately, medications that are better tolerated by people with PD are now available. Today, there are three antipsychotic medications considered relatively safe for people with PD: quetiapine , clozapine and the newest agent, pimavanserin . They cause limited worsening of PD while treating hallucinations and delusions.
Hallucinations And Delusions In Pd
Hallucinations and delusions are collectively referred to as psychosis.
Visual hallucinations are the most common type of hallucination. In a visual hallucination, someone sees things that are not actually there. There can also be auditory and olfactory hallucinations. Often hallucinations are not alarming to the person experiencing them.
Delusions are when there is an alternative view of reality: an entire irrational story is created. Paranoia is a common type of delusion. Capgras delusions are a specific type of delusion where the person believes that a spouse, adult child, or other family member has been replaced by an imposter.
How To Deal With Hallucinations In Pd Patients
At first, the doctor must know all the physical and mobility-related disorders that the patient suffers from. And neurologists, internists, and psychiatrists can cooperate in order to determine the proper approach for the patient. There are safe hallucination and psychosis medications that can help reduce the symptoms; however, many psychosis medications are prohibited for people with PD.Pimavanserin is one of the safe medicines for PD patients since it does not affect dopamine. Wherein hallucinations usually occur due to the increase of dopamine level in the brain. This dopamine increase is generally due to taking medications for controlling the movement-related symptoms of Parkinsons disease. And the supervising doctor has to reduce the dopamine doses in similar cases, or recommend taking dopamine from natural sources, such as Mucuna Pruriens, Moringa Oleifera, and others.
The Cause Of Parkinsons Delusions And Hallucinations
Some risk factors associated with the development of psychosis in Parkinsons disease include:
- Age: Parkinsons disease usually occurs in people over age 60.
- Duration and severity of Parkinsons disease: Psychosis is more common in advanced or late-stage Parkinsons disease.
- Later onset: Occurring later in life
- Hyposmia: A decreased sense of smell
- Cognitive impairment: Problems with thinking, including trouble remembering, difficulty learning new things, difficulty concentrating, problems making decisions that affect everyday life
- Depression: People who have both depression and Parkinsons disease are at a greater risk of developing psychosis.
- Diurnal somnolence: Daytime sleepiness
- REM sleep behavior disorder: A sleep disorder in which you physically act out dreams; involves making vocal sounds and sudden, often extreme, arm and leg movements during REM sleep
- Visual disorders: Impaired vision
- Severe axial impairment: Speech, swallowing, balance, freezing of gait
- Autonomic dysfunction: Impairment of the autonomic nervous system , which controls involuntary or unconscious actions such as heart rate, breathing, body temperature, blood pressure, digestion, and sexual function
- High medical comorbidity: The existence of more than one condition or illness in the same person at the same time; with Parkinsons disease, may include conditions such as dementia, depression, and sleep disorders
How Are They Treated

Your medical team should be aware of non-motor issues, just like your physical symptoms. Internists, neurologists, and psychiatrists together can help determine the right course for each person.
There are antipsychotic medications that are safe and can help to reduce the symptoms of Parkinson’s disease psychosis, but there are even more antipsychotics that are contraindicated for PD.
Let a medical provider know you have Parkinson’s when seeking emergency care or treatment for something by doctors who are not a part of your regular medical team.
There is only one drug, pimavanserin, approved in 2016 by the FDA specifically for PD. It has a mechanism of action that doesn’t block dopamine. This has made it a safer drug for people with Parkinson’s.2
Two other medications, quetiapine and clozapine, that have been used for a longer time, are also considered safe for treating hallucinations and delusions in people with PD.2
A Caregivers Guide To Parkinsons Disease Psychosis
While more than 50% of those taking carbidopa-levodopa may experience psychosis , medication management of these symptoms is a balancing act. First, families must bring psychotic behavior to the attention of your medical team. Medical causes of the behavior, like infection must be ruled out, followed by a review of medications and possible medication adjustments before a lifestyle changes and possible medications for treatment are added.
What Are Hallucinations And Delusions
Hallucinations are not dreams. They occur when a person is awake. Sometimes people are aware of their hallucinations this is called insight. Hallucinations are categorized by the five senses:
- Visual hallucinations occur when a person sees something that isnt actually there. These types of hallucinations are the most common among people with Parkinsons.
- Auditory hallucinations are sounds that are not there.
- Olfactory hallucinations occur when a person smells a smell that isnt present.
- Tactile hallucinations are experiences of feeling something that isnt there.
- Gustatory hallucinations occur when a person tastes a taste that has no source.
Delusions are false beliefs that are often irrational. They are less common than hallucinations about 1 in 10 people with Parkinsons disease experience delusions. Often people who have delusions believe they are being mistreated and can become angry or paranoid as a result.
People frequently experience jealousy delusions usually a belief that a spouse is being unfaithful. Persecutory delusions, a belief that someone is conspiring against you or trying to hurt you, are also common. These types of delusions usually involve a spouse, family member, or caregiver. The delusions make it hard to handle. They are directed at me and are very hurtful, a wife caring for her husband with Parkinsons shared on MyParkinsonsTeam.
Read How to Recognize Hallucinations and Delusions.
What Are The Causes
Parkinsons, a neurodegenerative disorder of the brain, affects the cells that produce chemicals in the brain that control movement and balance. PD medications boost dopamine levels to ease motor symptoms.3
However, too much dopamine can cause hallucinations and delusions. Other characteristics of disease progression such as cognition and visual-perceptual changes can also bring on these psychological changes.3
Oh So Thats A Delusion
We as a society casually label beliefs we dont understand delusions, but as seen in the examples provided above, a delusion isnt simply an eccentric opinion someone holdsits a completely illogical and often times bizarre conviction one steadfastly clings to in the face of insurmountable proof. In other words, your neighbor who thinks the buffet down the street purposefully serves whole wheat bread in order to make its patrons feel full more quickly is not delusional; your neighbor who thinks shes a time-traveler sent by aliens to save the world is delusional.
In general, we humans arent very accommodating to the absurdities of others. When we hear someone make a claim thats truly delusional in nature, our impulse is to immediately begin aggressively challenging that persons judgment by means of a one-two combination of disapproving expressions and fierce condemnations. To not do so, we presume, would be to tacitly allow their irrationalities to become a part of our logic-driven world.
But does forcefully rebuking someone experiencing a clinical delusion make it more likely the individual will realize the error of their judgment?
The answer is no.
Hallucinations And Delusions In Parkinsons Disease
It might be surprising to learn that 20 to 30 percent of people with Parkinsons disease will experience visual hallucinations. While typically not a symptom of PD itself, they can develop as a result to a change in PD medication or as a symptom of an unrelated infection or illness. It is important to know the signs of hallucinations and how to manage them.
Hallucinations and other more severe perceptual changes can be distressing to family often more so than to the person experiencing them. For the well-being of people with PD and caregivers, it is important to identify hallucinations as early as possible and take steps to reduce them.
The following article is based on the latest research and a Parkinsons Foundation Expert Briefings about hallucinations and delusions in Parkinsons hosted by Christopher G. Goetz, MD, Professor of Neurological Sciences, Professor of Pharmacology at Rush University Medical Center, a Parkinsons Foundation Center of Excellence.
Emergencies And Complications Of Device
Device-aided therapies include deep-brain stimulation, levodopa-carbidopa intestinal gel, and apomorphine subcutaneous injections and infusion. These are indicated to treat response fluctuations, such as recurrent disabling offs and dyskinesias refractory to standard therapy. Deep-brain stimulation is also used for drug-refractory tremor. Emergencies and complications related to device-aided therapies are not uncommon, and require prompt medical attention since they are generally associated with significant aggravation of Parkinsons disease symptoms .
An algorithm approach for DBS efficacy loss. DBS, deep-brain stimulation; LD, levodopa.
Risk Factors For Psychosis
Not everyone with Parkinsons will develop hallucinations or delusions, but there are several things can increase your risk:
- Dementia or impaired memory
- Depression: Individuals suffering from depression and PD are at a greater risk. In addition, severe depression alone can cause psychosis.
- Sleep disorders, such as vivid dreaming. Individuals commonly report vivid dreaming prior to the onset of psychosis. Other associated sleep disturbances include REM sleep disorder and general insomnia.
- Impaired vision
- Use of PD medications
Hallucinations In Parkinsons Disease Patients
Hallucinations are sensory experiences that do not exist nor relate to reality, and they include the five senses, sight, touch, hearing, smell, and taste. These delusions occur due to changes in the brain. People with dementia, delirium, Parkinsons, and other aging-associated diseases may suffer from these delusions and hallucinations.
Parkinsons Disease is a neurodegenerative disorder. Most people think that it is a mobility disorder related to shaking, rigidity, and slow movements. However, it can also impact the mood and the ability to think clearly.Coping with the movement-related symptoms may be hard, but the behavioral changes can be more devastating since they affect their lives completely.
In this article, we will tackle the definition and how to deal with hallucinations in Parkinsons disease patients.
What Are The Symptoms Of Psychosis
Two of the most prominent symptoms are hallucinations and delusions.7 Hallucinations involve seeing, hearing, experiencing or sensing things that are not really there. Delusions are false beliefs that are not based in reality. In describing symptoms of Parkinsons disease psychosis, patients may use such common terms as: seeing things, paranoia, flashbacks, nightmares, false beliefs, or not being in touch with reality.8
