If You Have Parkinson’s Disease
If you have been diagnosed with Parkinson’s, call your doctor if:
- You notice any significant change in your symptoms, such as severe episodes of freezingâa sudden loss of mobilityâwhich may affect walking.
- Your response to your medicine changes.
- Any other symptoms occur, such as constipation, sexual problems, or incontinence.
- You have symptoms of depression, such as feeling sad or hopeless and losing interest in daily activities.
- You or your family notice that you have problems with memory and thinking ability.
Is Early Diagnosis Possible
Experts are becoming more aware of symptoms of Parkinsons that precede physical manifestations. Clues to the disease that sometimes show up before motor symptoms and before a formal diagnosis are called prodromal symptoms. These include the loss of sense of smell, a sleep disturbance called REM behavior disorder, ongoing constipation thats not otherwise explained and mood disorders, such as anxiety and depression.
Research into these and other early symptoms holds promise for even more sensitive testing and diagnosis.
For example, biomarker research is trying to answer the question of who gets Parkinsons disease. Researchers hope that once doctors can predict that a person with very early symptoms will eventually get Parkinsons disease, those patients can be appropriately treated. At the very least, these advances could greatly delay progression.
Parkinson’s Disease and Movement Disorders Center
Our center provides compassionate and timely treatment to patients with movement disorders, such as dystonia, ataxia, essential tremor and similar conditions. But our mission goes beyond patient care excellence. By offering educational events and support groups, we empower patients and caregivers to become better partners in their health.
Passive Manipulation Of Limbs
To test for the presence of rigidity, we need to passively manipulate the limbs of the patient. However, If the disease is in its early stage or the symptoms are well controlled with medications, we may not be able to see rigidity. We will need to use some activation maneuvers, that basically consist in performing repetitive movements with the limb contralateral to the one that is being tested.
Also, there are two types of rigidity:
– Lead-pipe rigidity: where the tone is uniformly and smoothly increased throughout the entire range of movement
– Cogwheel rigidity: where a tremor is superimposed on the hypertonia, making the movement irregular due to intermittent increase and reduction of tone
Upper Extremity Testing
For the upper extremity the most sensitive joint where to check for rigidity is the wrist. To uncover rigidity, passively rotate the wrist and feel for a resistance to the movement. It is very important that the arm of the patient is fully relaxed when rotating the wrist. To do this, place your proximal hand under the patients forearm, while your distal hand grabs and rotates the wrist of the patient. When rigidity is present, the range of motion will be preserved but you will feel a resistance in performing the movement.
Wrist rotation with activation maneuver.
It is also possible to test for rigidity in the elbow by passively flexing and extending the forearm.
Elbow flexion-extension with activation maneuver.
Lower Extremity Testing
Also Check: Is Parkinson’s A Terminal Disease
The Importance Of Early Diagnosis
Early detection and diagnosis is important because the treatments for PD are more effective in the early stages of the disease. In addition, physical therapy and exercise, which greatly improve symptoms and delay progression of the disease, are much easier to perform in the early stages.
Current diagnosis is made through the presence of motor symptoms however, researchers have found that by the time motor symptoms occur, over 60% of all dopamine neurons in the basal ganglia of the brain have been damaged. Non-motor symptoms become apparent in people with PD long before motor symptoms, including sleep disturbances and loss of the sense of smell.3
Active areas of research include looking for markers in the blood, urine, or cerebral spinal fluid that reliably detect PD, called biomarkers. In addition, brain imaging tests that have high sensitivity for detecting PD are also being actively researched.4
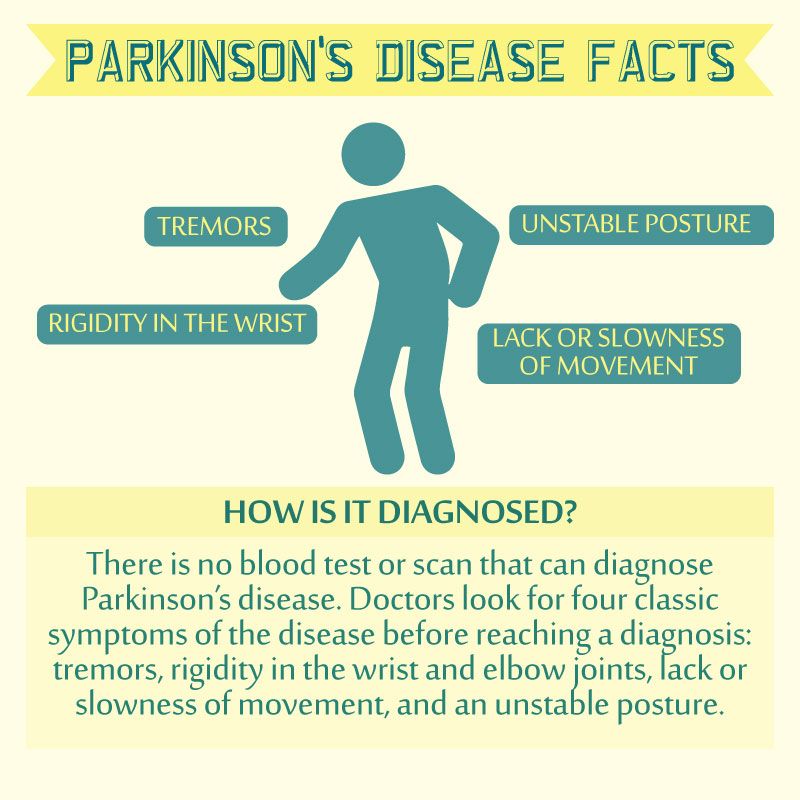
What Doctors Look For When Diagnosing Parkinsons
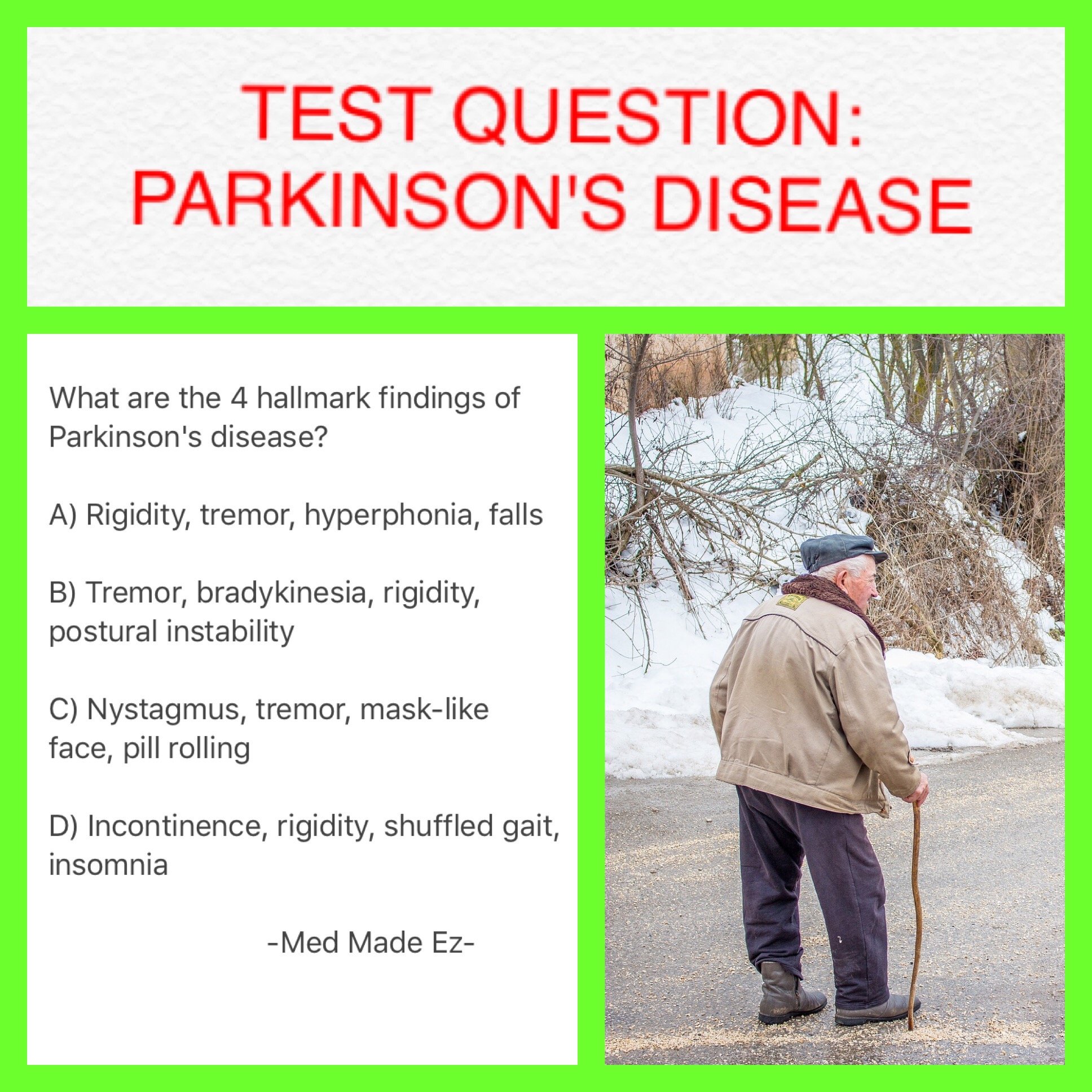
Certain physical signs and symptoms noticed by the patient or his or her loved ones are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctors office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinsons disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
Also Check: What Is The Life Expectancy Of Someone With Parkinson’s Disease
The Evolution Of Treatments
The history of Parkinson’s disease is tightly linked to therapeutic interventions, ranging from serendipitous observations to controlled clinical trials of specifically designed agents.
Parkinson devoted a chapter of his monograph to considerations respecting the means of cure . In humility and perhaps with a vision toward current concepts of neuroprotection, he hoped for the identification of a treatment by which the progress of the disease may be stopped . To this end, he advocated very early therapeutic intervention when signs were largely confined to the arms without balance and gait impairments. Reflecting therapeutic approaches of the early nineteenth century, Parkinson recommended venesection, specifically advocating bloodletting from the neck, followed by vesicatories to induce blistering and inflammation of the skin. Small pieces of cork were purposefully inserted into the blisters to cause a sufficient quantity of purulent discharge . All these efforts were designed to divert blood and inflammatory pressure away from the brain and spinal cord, and in this way, decompress the medulla that Parkinson considered the seat of neurological dysfunction.
Mri In Parkinson’s Testing
One of the more common tests done during a neurologic workup is an MRI scan and one may think that in the investigation of a disease that affects the brain such as Parkinsons, this imaging test would be a necessity. In the context of Parkinsons disease, however, an MRI is not particularly helpful. It looks at the structure of the brain which, for all intents and purposes, appears normal in this disease. An MRI may, however, be indicated when symptoms appear in younger people or if the clinical picture or the progression of symptoms is not typical for Parkinsons. In these situations, MRI can be used to rule out other disorders such as stroke, tumors, hydrocephalus , and Wilsons Disease .
Recommended Reading: Parkinson’s Symptoms Mayo
Foster A Good Relationship
Lastly, maintaining your relationship and communication with the person with Parkinsonâs can be the most challenging and rewarding aspect of caregiving. As Parkinsonâs disease progresses, the roles change and the person with Parkinsonâs may go from being an independent head of the household to a very dependent person requiring a significant level of care. However, research shows that despite high levels of strain, caregivers with good quality relationships have reduced depression and better physical health. Remember, as a caregiver your service to your loved one is beyond measure in terms of love, depth of care, and concern.
Obtaining A Parkinson’s Disease Diagnosis
During the exam, the neurologist will look for cardinal symptoms of the disease. Facial expressions and features will be assessed. The doctor will look for signs of tremor while the patient is at rest. The doctor may watch how easily the patient stands up from sitting in a chair. The doctor may also stand behind the patient and gently pull back on the patients shoulders and look for how easily the patient can regain balance. Good responsiveness to levodopa also helps support the diagnosis of PD. However, taking levodopa may exclude patients from clinical studies that need to recruit recently diagnosed patients who have not yet had treatment . Participation in a clinical trial should be discussed with the doctor.
PD can be challenging to accurately diagnose, particularly in early stages of the disease, which is why a neurologist trained in movement disorders is critical. Approximately 5-10% of patients with PD are misdiagnosed, as many of the symptoms of PD are similar to other diseases. If the patient thinks that he or she has been misdiagnosed, a second opinion may help.1,2
Also Check: Wehaveparkinsons
If Its Not Parkinsons Disease What Could It Be
Here are some possibilities:
Side effects of medication: Certain drugs used for mental illnesses like psychosis or major depression can bring on symptoms like the ones caused by Parkinsonâs disease. Anti-nausea drugs can, too, but they typically happen on both sides of your body at the same time. They usually go away a few weeks after you stop taking the medication.
Essential tremor: This is a common movement disorder that causes shaking, most often in your hands or arms. Itâs more noticeable when youâre using them, like when you eat or write. Tremors caused by Parkinsonâs disease usually happen when youâre not moving.
Progressive supranuclear palsy: People with this rare disease can have problems with balance, which may cause them to fall a lot. They donât tend to have tremors, but they do have blurry vision and issues with eye movement. These symptoms usually get worse faster than with Parkinson’s disease.
Normal pressure hydrocephalus : This happens when a certain kind of fluid builds up in your brain and causes pressure. People with NPH usually have trouble walking, a loss of bladder control, and dementia.
How Do I Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
You May Like: Parkinson’s Short Term Memory Loss
Living A Full Life With Parkinsons With Comprehensive Care
Susan had just celebrated her 61st birthday with her husband, Bob, daughter and close friends when she got the call that would change their lives forever. She was diagnosed with Parkinsons, a degenerative disorder that affects the central nervous system and progresses over time.
According to the Parkinsons Foundation, Susan is one of an estimated 1 million Americans currently living with the disease and, because Parkinsons is more common in people over the age of 60, the incidence of diagnosis it is expected to rise as baby boomers age.
Initially, Susan barely noticed any changes in her motor skills and was determined to live life to the fullest. Though she and Bob knew that the disease would eventually progress to the point where Susan would need more assistance and care, they decided they would wait to put any concrete plans in place.
My Fall Was Our Wake-Up CallTwo years later, Susan and Bob were beginning to struggle. Susans appetite had disappeared, despite Bobs efforts to prepare enticing meals, and she was losing weight. Her mobility had been impacted to the point where it was no longer safe for her to drive. With her husband working full-time and their daughter in graduate school two hours away, Susan was feeling lonely and depressed by her loss of independence.
Susan was not sleeping well and had begun losing her balance more frequently. Suddenly, Susan had a terrible fall on her backyard patio and had to be hospitalized during her recovery.
Gait & Balance Abnormalities
Parkinsons Disease Exam
Patients with Parkinsons disease can develop an alteration of the postural reflexes that causes instability in gait and balance control. Such alterations usually develop later in the course of the illness and are a major cause of disability, especially because of the high risk for falls that derives.
Using the exam to pick up postural instability is of the utmost importance for the management of patients with PD, since it will trigger either a medication adjustment or a physical therapy intervention both aimed at falls prevention.
We have three tests for this part of the PD exam:
1) Standing up from a chair
2) Free walking
3) Provoked pull test maneuver for balance
Recommended Reading: Early Onset Parkinson’s Life Expectancy
Drug Therapy And Research
If the disease progresses beyond minor symptoms, drug treatment may be indicated. Drug therapy for Parkinsonâs typically provides relief for 10â15 years or more. The most commonly prescribed medication is L-dopa , and this helps replenish some of the depleted dopamine in the brain. Sinemet, a combination of levodopa and carbidopa, is the drug most doctors use to treat Parkinsonâs disease. Recent clinical studies have suggested, in the younger person, the class of drugs called âdopamine agonistsâ should be used prior to levodopa-carpidopa except in patients with cognitive problems or hallucinations. In those older than 75, dopamine agonists should be used cautiously because of an added risk of hallucinations.
Other drugs are also used, and new drugs are continually being tested. It is common for multiple drugs to be prescribed because many of them work well together to control symptoms and reduce side effects. Contrary to past beliefs, starting Sinemet in newly diagnosed people does not lead to early symptoms of dyskinesia . Current knowledge is that the disease progression causes dyskinesias, not a âresistanceâ to the drug.
Quality of life studies show that early treatment with dopaminergic medications improves daily functioning, prevents falls, and improves a personâs sense of well-being.
What Is Essential Tremor And How Is It Different To A Parkinsons Tremor
A tremor is a rhythmical, involuntary movement that affects a part of the body, such as the hand.
Essential tremor is the most common type of tremor. Its most noticeable when your hands are doing something and it usually affects both the right and left sides of the body equally. Essential tremors often lessen when your body is resting.
Unlike an essential tremor, a Parkinsons tremor is most obvious when the affected body part is resting and tends to be less noticeable with movement. It usually starts on one side of the body and may progress to the other side as Parkinsons develops.
The time it takes to get a diagnosis can vary from person to person. Some people may receive a diagnosis of Parkinsons quite quickly, but for others it may be a long process. This can be due to a number of things, including your medical history, your age and what symptoms you have.
Your specialist may wish to rule out other causes of your symptoms first and see how you respond to treatment. This may take some time, and, as already mentioned, there is currently no definitive test for Parkinsons.
How you respond to treatment may help your specialist make a diagnosis. Keeping a diary or record of your symptoms will give the specialist more information to guide their decision.
Because the symptoms of Parkinsons are sometimes similar to other forms of parkinsonism, people can sometimes be misdiagnosed.
You May Like: How Do Most Parkinson’s Patients Die
Can Parkinsons Disease Be Diagnosed By How You Smell
Theres evidence that people with Parkinsons disease may emit a specific type of scent, which is related to increased sebum production. However, doctors have not developed a way to use this odor to diagnose the disease. More research is being done to see how the finding can help with diagnosis and treatment.
Early Signs Of Parkinson’s
Early physical signs include the common motor symptoms: tremor, muscle rigidity and slowness. They may also include the following:
- Symptoms starting on one side of the body
- Change in facial expression
- Failure to swing one arm when walking
- Stooped posture
- Loss of sense of smell
- Depression or anxiety
Some of these symptoms are quite common and by no means exclusive to Parkinsons, so if you have some of them, it does not mean you have Parkinsons.
Read Also: Mortality Rate Of Parkinson’s Disease
Other Challenges Of Diagnosing Parkinsons Disease
Parkinsons disease progresses slowly, often with non-motor symptoms appearing months or years before motor symptoms. This can make it challenging for doctors to diagnose you in the early stages, especially since the diagnostic criteria is based mostly on motor symptoms. You may have to wait until your symptoms progress for you and your doctor to confirm your diagnosis.14
Age and gender can be another issue. Since Parkinsons is associated more with older men, doctors may not think their younger or female patients have Parkinsons.5 On the other hand, since the disease is associated with aging, your symptoms may be blamed on getting older.
Remember that movement disorder specialists are extremely knowledgeable about Parkinsons disease and can help put the pieces together where other more generalized doctors may not. Never hesitate to fight for the care you deserve.
Related: Heres whats important to remember if you were just diagnosed with Parkinsons disease.
Who Gets Parkinsons Disease
Parkinsonâs disease, documented in 1817 by physician James Parkinson, is the second most common neurodegenerative disease after Alzheimerâs disease. Estimates regarding the number of people in the United States with Parkinsonâs range from 500,000 to 1,500,000, with 50,000 to 60,000 new cases reported annually. No objective test for Parkinsonâs disease exists, so the misdiagnosis rate can be high, especially when a professional who doesnât regularly work with the disease makes the diagnosis.
Also Check: Parkinson Disease Genetic Link
