Involvement Of The Autonomic Nervous System In Pd
PD is characterised by deposition of abnormally phosphorylated -synuclein. The aggregates are typically found in neurons as Lewy bodies. Alongside the hallmark degeneration of the substantia nigra in PD, Lewy bodies and cell loss are detected in: autonomic regulatory areas such as the hypothalamus, parabrachial nucleus, intermediate reticular zone of the medulla, locus coeruleus and raphe preganglionic parasympathetic regions, such as the EdingerWestphal nucleus and dorsal vagal motor nuclei preganglionic sympathetic neurons in the intermediolateral cell column and neurons in paravertebral and paravertebral autonomic ganglia. Histological loss of neurons and Lewy body accumulation in sympathetic ganglia, and cardiac sympathetic denervation in several studies are also evident. In addition, -synuclein pathology has been reported to be shown in the ventrolateral medulla and the enteric plexus in PD patients. The lesions in autonomic regulatory areas could be key causes of cardiovascular, sudomotor, bladder and bowel dysfunction. Evidence suggests that urinary dysfunction is also a process of degeneration in the substantia nigra as urinary dysfunction in PD appears to correlate with PD severity.
Autonomic Dysfunction And Parkinson’s
Autonomic dysfunction often occurs in Parkinsons due to the loss of dopamine-producing cells and the presence of microscopic protein deposits called Lewy bodies in the brain. As a result, a number of non-motor symptoms may be experienced. Research suggests that the peripheral nervous system may be affected long before such symptoms appear.
If autonomic dysfunction is severe, atypical parkinsonism, such as multiple system atrophy , should be suspected.
Please click on the links below for information on individual symptoms related to ANS dysfunction:
- bladder problems including urgency, frequency, incontinence and night time urination
- constipation and weight loss
- swallowing difficulties .
Scientists now recognise that many medications used to treat Parkinsons can affect the ANS and so make symptoms worse. It is important to monitor your medications and symptoms so that you can discuss these with your doctor. He or she may then be able to adjust medications to reduce the impact on the ANS and so improve symptom control. See Keeping a diary for more information on this and how it can help.
Research suggests that about 90% of people with Parkinsons experience autonomic dysfunction which may considerably reduce quality of life.
Content last reviewed: January 2020
Prevalence Of Autonomic Dysfunctions In Pd
The common cardiovascular autonomic dysfunctions in PD are orthostatic hypotension and its related symptoms. Senard et al. first carried out the epidemiological study of OH in PD in 1997 . The researchers measured the blood pressure of 91 PD patients who stood for 10 minutes after lying supinely for 15 minutes. The related symptoms, including dizziness, postural instability, vertigo, blurred vision, syncope, fatigue, and hearing loss, were also documented. The prevalence of OH in PD patients was 58.2% , of which 19.8% had corresponding symptoms. Jost and Augustis measured the blood pressure before and after the postural change of 106 PD patients, finding that the severity of OH, defined as maximal drop of systolic blood pressure after postural challenge, was not correlated with the course of disease . Similar studies have shown that the prevalence of OH in PD is 47% and that the prevalence of OH does not vary with the course and severity of the disease . A meta-analysis study, which included 25 studies and 5070 PD patients, estimated that the prevalence of OH in PD was 30.1% .
About 27% to 39% PD patients had symptoms of urinary system dysfunctions, which could be categorized into irritative and obstructive symptoms . The incidence of detrusor hyperreflexia was as high as 45 to 100%, while the incidence of obstructive symptoms was 27% .
Recommended Reading: What Medicine Do You Take For Parkinson’s Disease
Swallowing And Gastrointestinal Dysfunction
In patients with synucleinopathies gastrointestinal function is affected at all levels, from chewing to defecation.105, 106 Dysphagia in patients with PD and DLB is usually mild and occurs late in the disease course, whereas in patients with MSA it can be early and severe.107 Aspiration pneumonia, the most feared complication of dysphagia, is a common cause of death in patients with synucleinopathies.108 Upper gastrointestinal symptoms , and lower gastrointestinal symptoms, such as constipation, are virtually universal in patients with PD, DLB and MSA and contribute to decreased quality of life.109
Clinical Significance Of Autonomic Dysfunctions In Pd Early Diagnosis And Differential Diagnosis
The pathological study of 98 patients without mental and neurological diseases carried out by Bloch et al. showed that -synucleinopathy was detected in 17 patients . A further pathological study of these 17 idiopathic Lewy body disease patients showed that -synucleinopathy was found in brainstem, olfactory nerve, thoracic nucleus of the spinal cord, sacral parasympathetic nucleus, esophageal myenteric plexus, and sympathetic ganglion. This study suggests that, in addition to medulla oblongata and olfactory system, autonomic nervous system is also the first site where pathological changes occur . Another pathological study of abdominal and pelvic surgical specimens from 100 patients without neurological diseases showed that -synucleinopathy was positive and distributed in autonomic plexus in 6 patients . In the follow-up study of the six patients, it was found that the myocardial MIBG uptake was decreased and the recovery of blood pressure after Valsalva maneuver was slower in the six patients than in the control group. These two studies show that the pathological changes occur early in peripheral autonomic nervous system in iLBD, pathologically suggesting that autonomic dysfunctions may be a biomarker for early diagnosis of PD.
You May Like: Is Parkinson’s Easy To Diagnose
Autonomic Dysfunctions In Parkinsons Disease: Prevalence Clinical Characteristics Potential Diagnostic Markers And Treatment
Abstract
Parkinsons disease is a common neurodegenerative disease in the middle-aged and the elderly. Symptoms of autonomic dysfunctions are frequently seen in PD patients, severely affecting the quality of life. This review summarizes the epidemiology, clinical manifestations, and treatment options of autonomic dysfunctions. The clinical significance of autonomic dysfunctions in PD early diagnosis and differential diagnosis is also discussed.
1. Introduction
In this review, we will discuss the prevalence, clinical manifestations, and treatment of autonomic dysfunctions in PD, as well as the clinical significance of autonomic dysfunctions in early diagnosis and differential diagnosis of PD.
2. Prevalence of Autonomic Dysfunctions in PD
About 27% to 39% PD patients had symptoms of urinary system dysfunctions, which could be categorized into irritative and obstructive symptoms . The incidence of detrusor hyperreflexia was as high as 45 to 100%, while the incidence of obstructive symptoms was 27% .
3. Clinical Manifestations of Autonomic Dysfunctions in PD
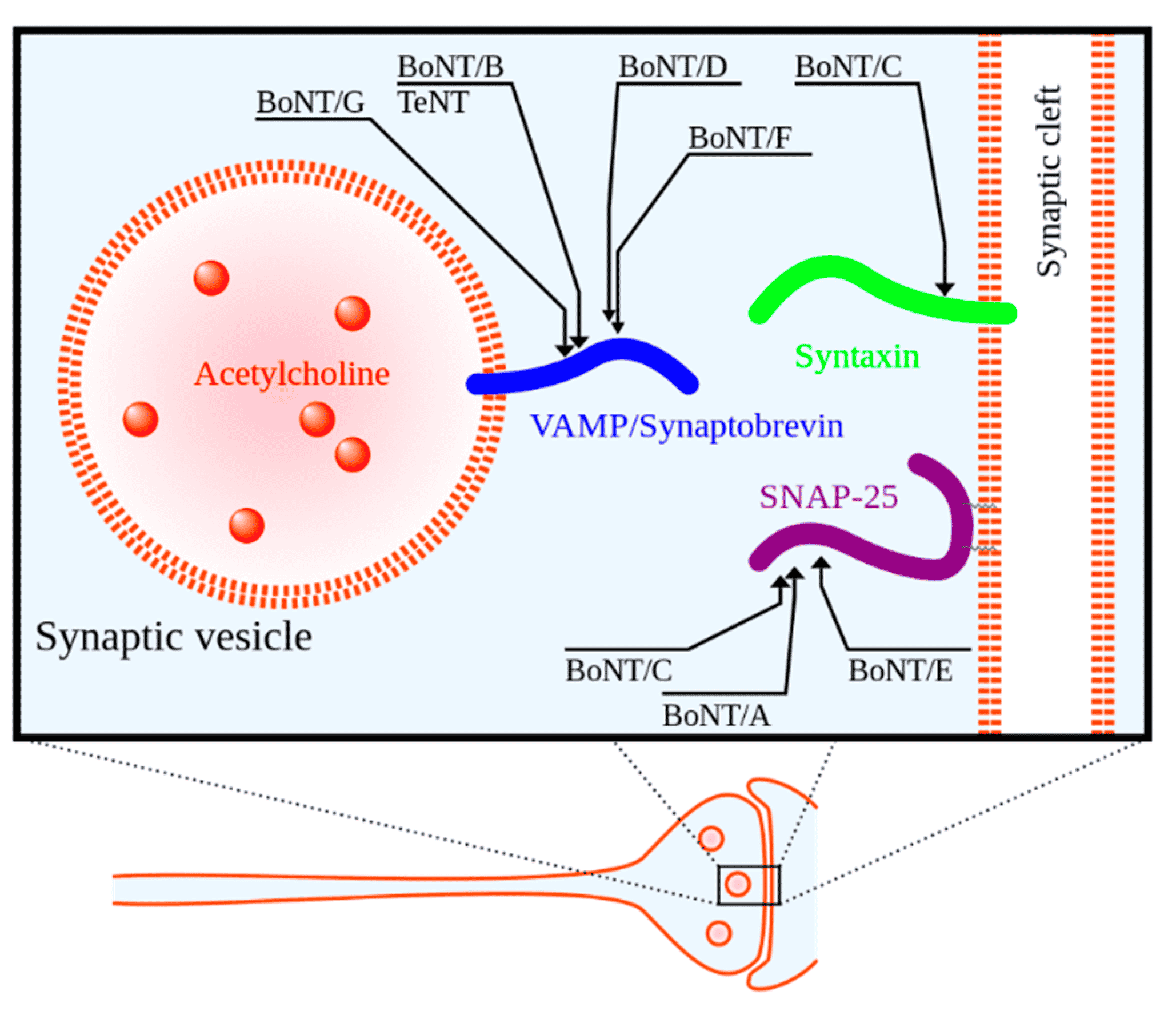
Autonomic dysfunctions in PD can involve the sympathetic noradrenergic system , the sympathetic cholinergic system , the sympathetic adrenomedullary system , the parasympathetic nervous system , and the enteric nervous system manifested as symptoms and signs of cardiovascular system, digestive system, urinary system, reproductive system and skin, and other systems .
3.1. Autonomic Dysfunctions of Cardiovascular System
Autonomic Dysfunctions Of Urinary System
The autonomic dysfunctions of urinary system can be manifested as irritative symptoms and obstructive symptoms. The most common irritative symptoms in PD patients include nocturia, followed by urinary urgency and frequency. Acute urinary incontinence is frequently seen in PD patients with obvious dyskinesia . The obstructive symptoms of urinary system in PD include urinary hesitation, urinary exertion, thinning of urine flow, and incomplete emptying. These symptoms need to be carefully differentiated from prostate hyperplasia, which is a common comorbidity in elderly PD patients. PD itself can also cause obstructive symptoms mainly due to decreased activity and sensation of detrusor, as well as delayed relaxation of urethral sphincter .
Read Also: Parkinson’s Carbidopa Levodopa Side Effects
Autonomic Dysfunction In Men With Parkinsons Disease
Log in to MyKarger to check if you already have access to this content.
Buy a Karger Article Bundle and profit from a discount!
If you would like to redeem your KAB credit, please log in.
Save over 20%
- Unlimited fulltext viewing Of this article
- Organize, annotate And mark up articles
- Printing And downloading restrictions apply
- Access to all articles of the subscribed year guaranteed for 5 years
- Unlimited re-access via Subscriber Login or MyKarger
- Unrestricted printing, no saving restrictions for personal use
The final prices may differ from the prices shown due to specifics of VAT rules.
Dont Miss: On-off Phenomenon
The Impact Of Autonomic Dysfunction On Survival In Patients With Dementia With Lewy Bodies And Parkinsons Disease With Dementia
-
Affiliation Clinical Memory Research Unit, Department of Clinical Sciences, Malmö, Lund University, Sweden
-
Affiliations Center for Age-Related Medicine, Stavanger University Hospital, Stavanger, Norway, Department of Neurobiology, Ward and Society, Alzheimers Disease Research Center, Karolinska Institutet, Stockholm, Sweden
-
Affiliation Clinical Memory Research Unit, Department of Clinical Sciences, Malmö, Lund University, Sweden
Don’t Miss: What Are The First Signs Of Parkinson’s Disease
Correlation Between Scale For Outcomes In Parkinsons Disease For Autonomic Symptoms And Clinical Factors
The presence and severity of AutD can be affected by diverse clinical factors as some autonomic phenotypes may occur simultaneously with other clinical symptoms. To thoroughly investigate the correlation between SCOPA-AUT and other PD clinical manifestations, we employed partial correlation analysis investigating the SCOPA-AUT total score and its six subdomains . The total SCOPA-AUT score was significantly and positively associated with the motor severity scales and some of the non-motor symptoms, such as ESS and RBD. Meanwhile, the overall score of AutD and almost all the subdomains of AutD, except for the sexual domains, showed a significant correlation with the HAMD, fatigue scale, and PDQ-39, all of which were commonly used methods for the assessment of the quality of life. The gastrointestinal domain turned out to be the most significant contributor among all the domains of the SCOPA-AUT scale. The PDSS, MMSE, and HRS scores, in which lower scores indicate more severe symptoms, were also significantly and negatively correlated with the AutD total score and most of the subdomains. Details are shown in Figure 2. Together these results emphasize that autonomic dysfunctions are a key factor affecting the quality of life of patients with PD.
Autonomic Problems In Parkinsons Disease
There have been current advances as well as the experience of doctors, the healthcare team, and family members when taking care of patients with Parkinsons disease. They have revealed that autonomic problems play a crucial role in the evaluation of patients and that the signs and symptoms that present are sometimes the cause of disability. Symptoms seen in Parkinsons disease include cardiovascular dysfunction, sweating, and gastrointestinal failure, among others.
What Is Orthostatic Hypotension?
The American Autonomic Society describes orthostatic hypotension as a change in orthostatic blood pressure, with its systolic value dropping to 20 points and the diastolic dropping to 10 points. It is measured in the standing position and within three minutes. Heart rate also increases to over 130 beats per minute, which is known as postural tachycardia. However, it is important to note that the effects of medication, dehydration, and intravascular volume depletion may also affect the changes seen in PD patients.
We are ashamed that we are ill and so we dont speak about it this silence surrounding illness feeds back into our shame, reinforcing our seeming inability to speak. Katie Willard Virant MSW, JD, LCSW
Are There Non-specific Symptoms Suggesting Hemodynamic Or Cardiovascular Autonomic Dysfunction?
What Other Dysautonomias Can Be Seen In PD Patients?
Which Gender Is More Affected?
How Is Erectile Dysfunction Seen In PD Patients?
How Can Sexual Issues Be Treated?
You May Like: Can Parkinson’s Affect Your Eyes
Treatment Of Neurogenic Orthostatic Hypotension
The goal of nOH treatment in patients with synucleinopathies is not to normalize standing BP, but to reduce symptom burden, improve quality of life, and reduce morbidity and mortality associated with nOH.35 Consensus guidelines for the treatment of nOH are available.36, 37 The steps of nOH management include: a) correcting aggravating factors, b) implementing non-pharmacological measures and c) drug therapies. When OH is asymptomatic, treatment may not be required or may be limited to non-pharmacological measures. When nOH is symptomatic pharmacological treatment is usually required .
Algorithm for the management of neurogenic orthostatic hypotension in patients with synucleinopathies
Correction of aggravating factors
Drugs that reduce intravascular volume , induce vasodilatation , or block norepinephrine release/activity at the neurovascular junction worsen nOH and symptoms. Levodopa and dopamine agonists may also lower BP and a dose adjustment may be considered based on an individual risk-benefit assessment.38–41 Anemia should be investigated and treated.42 Erythropoietin in conjunction with iron supplements may be beneficial in patients with nOH and anemia.43
Non-pharmacological treatment and patient education
Pharmacological management
Sites of action and mechanism of therapeutic agents used for the treatment of neurogenic orthostatic hypotension
Autonomic Dysfunction In Parkinsons Disease
Dysautonomia is a prominent non-motor complication of Parkinsons disease that may manifest many years prior to the onset of traditional motor symptoms. However, the nature of this dysfunction in PD remains poorly understood.
We are working with NYU Langones Dysautonomia Center to develop mechanistic understanding and develop biomarkers for these prodromal syndromes of synucleinopathies such as PD, dementia with Lewy bodies , and multiple system atrophy .
We also work with gastroenterologists to systematically study the physiological nature of constipation in PD patients. Using state-of-the-art methods to assess gastrointestinal function, we aim to determine whether PD constipation is unique in its etiology and requires specialized treatment modalities. We are also intensely interested in understanding the role of gut health in the pathogenesis of PD.
Read Also: Is Leg Pain A Symptom Of Parkinson’s Disease
Postural Orthostatic Tachycardia Syndrome
POTS affects anywhere from 1 to 3 million people in the United States. Nearly five times as many women have this condition compared to men. It can affect children, teenagers and adults. It can be also associated with other clinical conditions such as Ehlers-Danlos syndrome, an inherited condition of abnormal connective tissue.
POTS symptoms can range from mild to severe. Up to one out of four people with POTS have significant limitations in activity and are unable to work due to their condition.
Hereditary Sensory And Autonomic Neuropathies
HSAN is a group of related genetic disorders that cause widespread nerve dysfunction in children and adults. The condition can cause an inability to feel pain, temperature changes, and touch. It can also affect a wide variety of body functions. The disorder is classified into four different groups depending on age, inherited patterns, and symptoms.
Recommended Reading: Which Is Worse Huntington’s And Parkinson’s
Complications In Advanced Pd
While worsening of motor function and drug-induced motor complications represents a major challenge in patients with mid-stage to advanced disease, in the advanced stage of PD the most troublesome and distressful complications are usually nonmotor symptoms, including psychiatric and cognitive disorders, autonomic disturbances, and sleep disorders that significantly increase the need for supportive care. Unfortunately, these symptoms are frequently neglected in clinical practice due to limited consultation time, perception of the patient and caregivers that their symptoms are unrelated to the disease, or insufficient awareness of the clinicians, who generally focus on motor symptoms .
Proper supporting care becomes increasingly important in advanced PD. Rehabilitative and support services for patients and family become key interventions as the disease reaches its more debilitating stages and pharmacologic or surgical treatment becomes less relevant. Management of motor and nonmotor complications in advanced PD requires careful and ongoing assessment of whether symptoms are a side effect of medication or related to the progression of the disease .
Medication Issues
Read Also: Judy Woodruff Health Problems
Distinguishing Between Parkinsons Disease And Msa
It can be challenging to differentiate between PD and MSA. Early on in the course of the illness, MSA can manifest with mild parkinsonism and autonomic dysfunction. These clinical features are also often present in PD. Furthermore, in the beginning, the parkinsonism of MSA can be minimally responsive to levodopa, complicating the distinction between the diseases even more. Both diseases have a high rate of REM behavior sleep disorder . Therefore, it is very common for someone with MSA to initially receive a diagnosis of PD.
Over time, clinical features may develop that are not as common in PD and may suggest MSA as a diagnosis. However, although these features are not as common in PD, they can still be present in PD, so diagnosis remains difficult. The more features that are uncommon in PD that are present, the more the clinical situation warrants the consideration of MSA as the diagnosis. These red flags include:
- Poor levodopa response
Recommended Reading: Does Sam Waterston Have Parkinsons
You May Like: How To Care For A Person With Parkinson’s Disease
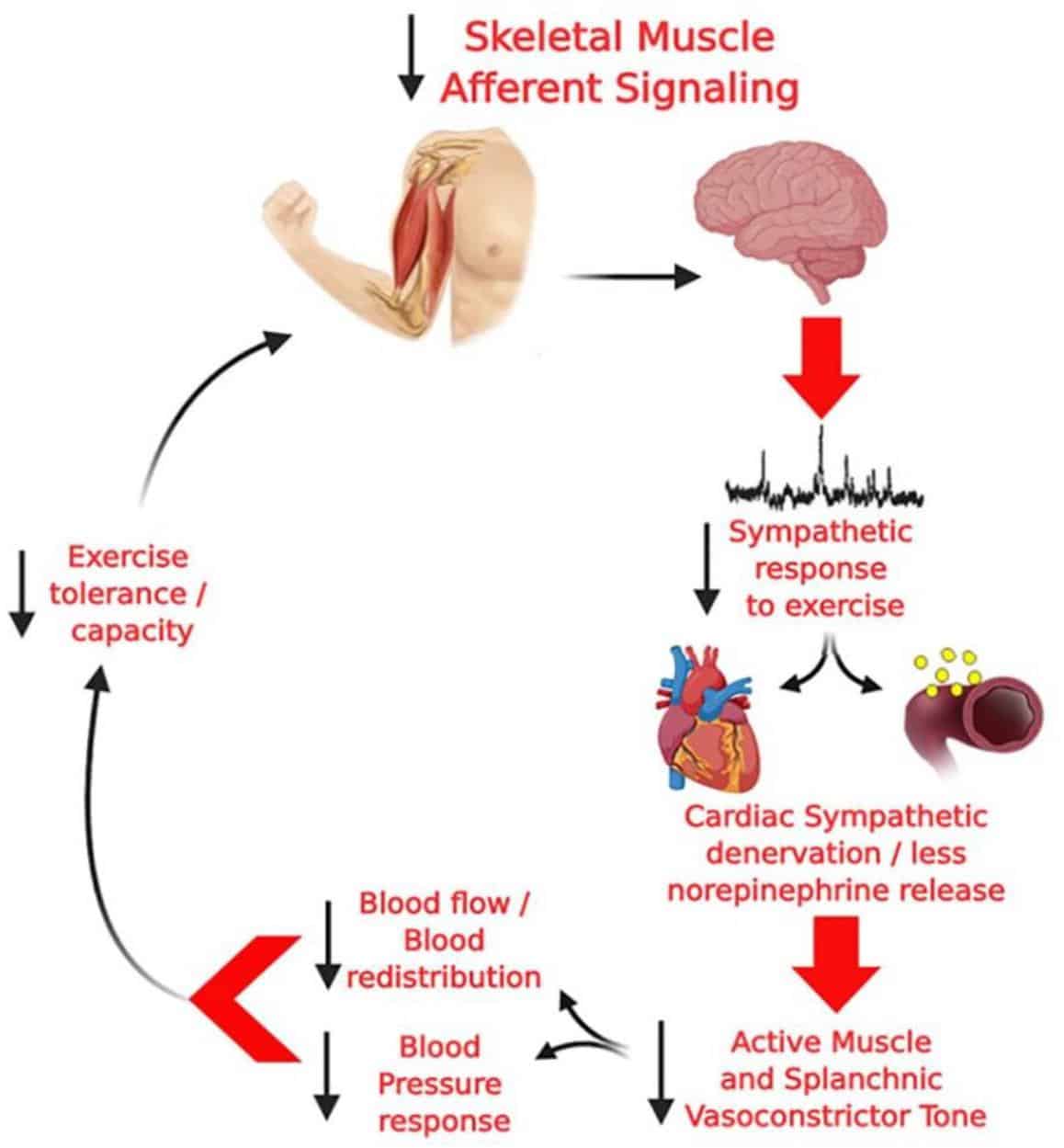
How Parkinsons Disease Affects The Autonomic Nervous System And The Heart
In PD, there are two major reasons why the automatic control of the cardiac system is impaired. First, areas of the brain that control this system often contain Lewy bodies and have undergone neurodegeneration. In addition, the autonomic nervous system itself is directly affected by Lewy body-like accumulations and neurodegeneration. This means, when the baroreceptors in the heart and carotid artery sense a drop in blood pressure and try to generate a signal to the heart and blood vessels to increase the blood pressure, the message may not get through. This results in neurogenic orthostatic hypotension , or drops in blood pressure upon standing due to autonomic nervous system dysfunction. There are no medications that can cure nOH by restoring the autonomic nervous system in PD. nOH however, can be treated. Read more about nOH and its treatments here.
Structural problems of the heart such as coronary artery disease or cardiomyopathy are not thought to be part of the pathology of PD, although of course, could co-exist with PD.
Autonomic Dysfunctions Of Other Systems
Autonomic dysfunctions of PD can also be manifested as thermoregulatory dysfunctions, such as high sensitivity to temperature, abnormal sweating, and abnormal body temperature. Temperature sensitivity includes cold intolerance and hot intolerance with the former one more common . Abnormal sweating can be manifested as decreased sweating of the trunk, increased sweating of head, face, and limbs, increased sweating of the affected side, and intermittent sweating . It has been shown recently that chronic hyperhidrosis was associated with higher rate of nonmotor symptoms, such as sleep disorders, anxiety, depression, dyskinesia , and worse quality of life . Abnormal body temperature in PD patients is typically paroxysmal high fever, especially in sudden withdrawal of anti-Parkinson’s drugs and in off-phase .
Recommended Reading: What Tests Diagnose Parkinson’s Disease
