Clinical Research Of Parkinson’s Disease
Dr. Farbman is very interested in clinical research around Parkinsons and says, Fortunately, this is an exciting time to be treating Parkinsons Disease. In addition to the recent FDA-approval of many new Parkinsons treatments, there are many clinical research trials ongoing. Roseman University is a site for both the Parkinson Study Group and the Huntington Study Group with studies for patients with many different degrees of the disease, from newly diagnosed to advanced. A new study will soon be started on multiple system atrophy, an atypical Parkinson-plus disorder with no current treatments, as well as an essential tremor study. Farbman is hopeful that there will be some new Huntingtons research studies soon as well.
Essential Tremor Is Different From Parkinsons Disease And Often Far Less Serious
Benign Essential Tremor vs. Parkinsons Disease: Whats the Difference?
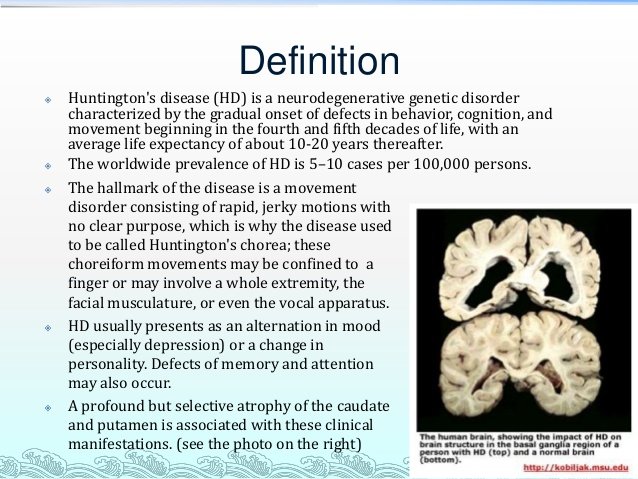
No one wishes for a chronic, long-lasting medical condition but some are more dreaded than others especially if theres no cure. Diseases that involve neurological deterioration are particularly fearful. They affect the brain and/or nervous system. They include deteriorating conditions like MS, ALS, Huntingtons disease, Alzheimers disease, Parkinsons disease and others.
When a person develops an involuntary rhythmic shaking it is normal to be worried because a tremor of the hands, head or other part of the body can be a symptom of Parkinsons disease . However, the most common involuntary movement disorder, benign essential tremor , is in a neurological class of its own. It is estimated that 4% of people over 40 have ET, affecting at least 10 million North Americans. Unlike PD, it is more apt to cause minor impairments, inconvenience, and embarrassment.
Nonetheless, when trembling of the hands, face or neck begins, it is common for patients to worry that they have PD. There are several ways to tell PD from ET, and specialists called neurologists are trained to tell which is which, thus putting the minds of ET patients at rest.
| ET |
Cerebral Dopamine Neurotrophic Factor And Mesencephalic Astrocyte
In 2003, a protein called mesencephalic astrocyte-derived neurotrophic factor was characterized and demonstrated to promote survival of embryonic dopaminergic neurons in vitro . Then, a homologous protein called CDNF was discovered with a protective role for dopaminergic neurons. Several studies evidence the protective role of CDNF and MANF in dopaminergic neurons against the injury caused by -syn oligomers . The intrastriatal injection of CDNF prevents the loss of TH-positive neurons in a 6-OHDA-lesioned rat model of PD , and protected dopaminergic neurons in 6-OHDA and MPTP mouse models of PD . MANF has been tested in the 6-OHDA-lesioned rat model showing beneficial effects . CDNF and MANF diffuse to the brain significantly better than GDNF, and CDNF was more efficient in reducing amphetamine-induced ipsilateral rotations in the 6-OHDA rat PD model in comparison with GDNF treatment . In 6-OHDA-lesioned monkeys, PET imaging showed a significant increase of DA transporter ligand-binding activity in lesioned animals treated with CDNF .
The first phase III clinical trial using CDNF in PD patients is being conducted since 2017. In this study, an implanted drug delivery system for Ipu of recombinant human CDNF is used in patients with idiopathic mild-advanced PD . Additionally, another phase III clinical trial to evaluate the beneficial effects of CDNF in PD patients is still on course . Currently, the delivery of CDNF for HD treatment has not been described.
Read Also: Is Parkinson Disease Genetically Inherited
Essay On Dry Eye Syndrome
This ocular pathology is lacking in an exact defined cause, even though numerous cases are related to hormonal changes. Generally, the condition may be caused by: Aging, because the secretion of tears decreases with age Decrease in estrogen levels Use of contact lenses Eye surgeries Prolonged exposure to the sunlight Consumption of medicines for the cold Exposure to air-conditioned environments Cigarette smoke Chronic diseases like Parkinsons and also diabetes So how exactly does dry eye syndrome manifest itself? The signs and symptoms of dry eye syndrome vary between each patient, typically depending on the cause of it. Among its most typical clinical manifestations are: Eye dryness Sandy feeling in the eyes Discomfort once blinking Redness of the eyes Itchy and itchy eye Increased level of sensitivity to light Blurred vision A headache Natural remedies for dry eye syndrome To deal with the signs and symptoms of this disease, synthetic tears usually are prescribed, which can or might not contain preservatives. They are used 2 or 4 times a day, depending on the severity of the
Depression With Huntingtons Disease
Due to the nature and lower life expectancy of Huntingtons disease, it is common for a diagnosis to lead to depression. Patients with Huntingtons are at a higher risk of suicide.
If you are struggling with your Huntingtons diagnosis or prognosis, contact the Substance Abuse and Mental Health Services Administration National Helpline online or call 1-800-662-4357 to seek help.
For more mental health resources, including a helpful list of links and hotline numbers, see our National Helpline Database.
Don’t Miss: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Meet The Disease That Feels Like Als Parkinson’s And Alzheimer’s All At Once
Being released this week is a new documentary from intrepid filmmaker Lucy Walker about confronting one of life’s most daunting moments.
Breakthroughs in modern science allow us the ability to take a peek under our genetic “hoods” at minimal cost and with unprecedented speed. Services like 23andMe allow any consumer to explore their gene profile, which could be empowering or frightening depending on your perspective and family history. This data, when used in the clinic, provides physicians incredible tools in the quest to practice fully personalized medicine.
Our genes provide the blueprint for our individuation, and come replete with a mixed bag of advantages and potential disadvantages — a natural person-to-person variation which was essential to driving our species forward by way of natural selection. Today, being tethered to negative health outcomes, especially when we can see these risks decades before their potential emergence, are inconvenient in a time when overcoming our biological limitations seems to be as natural as genes themselves.
In The Lion’s Mouth Opens, Walker focuses on young actress Marianna Palka as she finds out whether she has inherited this fate, an incurable degenerative disorder which took her father and now has a 50 percent chance of taking her body and her mind.
I couldn’t wait to ask my friend Lucy Walker about her experience documenting this harrowing journey, her thoughts on genetic testing, and how to get involved with Marianna’s story.
Gene Therapies For Pd And Hd
For the development of new therapies for PD and HD, it is important to include, especially for HD and genetic forms of PD, genetic correction/editing of the mutated gene. Nowadays, there are several gene silencing/editing technologies, including RNA interference , antisense oligonucleotides , and clustered interspaced short palindromic repeats , which can be used as therapies for the treatment of PD and HD. For a more in-depth knowledge of gene therapy delivery systems and other cellular targets, reviews are published elsewhere .
As previously stated, PD is characterized by the selective degeneration of dopaminergic neurons in the SN, thus approaches aiming to revert this loss based on the delivery of genes encoding for enzymes required for DA synthesis could be useful. The first enzyme for DA synthesis is TH, which requires the enzyme GTP-cyclohydrolase-1 to synthesize a cofactor for DA biosynthesis . TH converts tyrosine into L-dopa, which finally is converted into DA by the aromatic L-amino acid decarboxylase . Therapies to deliver enzymes involved in DA synthesis have been proved in preclinical and clinical studies showing its benefits.
Recommended Reading: Can Alcoholism Mimic Parkinson’s
They Are About The Same
Parkinson’s Disease and Huntington’s Disease are about the same as far as the impact they have on quality of life. They both begin gradually starting with simple coordination problems. Then that leads on to loss of motor control. Then later they both lead to deterioration of a persons mental capacity. I do not see how one could be any worse than the other. They are both horrible.
Whats The Difference Between Lewy Body Dementia Parkinsons Disease And Alzheimers Disease
Lewy body dementia is an umbrella term for two related clinical diagnoses: dementia with Lewy bodies and Parkinsons disease dementia. These disorders share the same underlying changes in the brain and very similar symptoms, but the symptoms appear in a different order depending;on where the Lewy bodies first form.
Dementia with Lewy bodies is a type of dementia that causes problems with memory and thinking abilities that are severe enough to interfere with everyday activities. It specifically affects a persons ability to plan and solve problems, called executive function, and their ability to understand visual information. Dementia always appears first in DLB. The motor symptoms of Parkinsons such as tremor, slowness, stiffness and walking/balance/gait problems usually become more evident as the disease progresses. Visual hallucinations, REM sleep behavior disorder, fluctuating levels of alertness and attention, mood changes and autonomic dysfunction are also characteristic of DLB.
Finally, Alzheimers is characterized by different abnormal clumps called amyloid plaques, and jumbled fiber bundles called tau tangles. These microscopic structural changes in the brain were discovered by Dr. Alois Alzheimer in 1906. These plaques and tangles, together with loss of connections between nerve cells, contribute to loss of coherence and memory, as well as a progressive impairment in conducting normal activities of daily living.
You May Like: Which President Had Parkinson’s
Parkinson Disease Case Study
Anaesthetic Management of a patient with Parkinsonism Posted for Wide Excision of Skin Adenexal Tumour in the Axilla: A Case ReportIntroduction Parkinsons disease has been known since biblical times but it was first formally described by James Parkinson in the 18th century and termed the shaking palsy. Although the aetiology of the disease is unknown, age has been identified as the most consistent risk factor. Parkinsons disease affects approximately 3% of the population over 66 years of age and with increasing age of the general surgical patients it is becoming an important cause of perioperative morbidity Parkinsonism is due to the imbalance of the mutually antagonistic dopaminergic and cholinergic systems of the basal ganglia. Pigmented
Given A Choice I Would Choose Huntington’s Over Parkinsons
Huntington’s will often manifest itself in jerking motions or incomplete motions, causing repetition or what appear to be “ticks” The ability to walk and move are hindered due to these symptoms. It is manageable though. It may take a little longer to do things do to the stop/start tendencies related to most movements, but it is still doable. Parkinson’s manifests as uncontrollable jerking motions that do not relate to actual function. The result is motor skills completely crippled due to the danger of the sporadic movements. Both diseases are partnered with their own mental dysfunctions, but the physical is still manageable by the time the mental is truly unmanageable and requires institutionalization or at least constant monitoring. You can live happier for longer with Huntington’s.
Don’t Miss: What Is The Life Expectancy Of Someone With Parkinson’s Disease
About Eric S Farbman Md
Eric Farbman, M.D. grew up in New Jersey as the oldest of three and the son of an engineer father, and homemaker and social worker mother. He received his Bachelor of Science and Master of Science degrees from Tufts University and while deciding if his path was leading towards a Doctor of Philosophy to conduct research, or a Doctor of Medicine to treat patients, an old friend encouraged Dr. Farbman to overnight his application to take the Medical College Admissions Test . That advice helped catalyze his decision-making process and set him on his path in medicine.; He went on to receive his M.D. from Rutgers University Medical School.
Medical school curriculum was difficult, but once exposed to clinical experiences, Dr. Farbman began to feel more optimistic about his decision to attend medical school. He enjoyed the neuroscience and neuropathology courses, which led to his future sub-specialty in neurology. Following a four-year residency, Farbman went on to complete a Movement Disorders Fellowship, all through University of Pittsburgh. Dr. Farbman found Pittsburgh to be the ideal place for residency training and to enjoy a favorite pastime, baseball, on the river at PNC Park which he describes as a beautiful and accessible baseball stadium.
What Is Lewy Body Dementia
Lewy body dementia is not a single disorder but rather a spectrum of closely-related disorders involving disturbances of cognition, behavior, sleep, movement and autonomic function.
In these progressive disorders, Lewy bodies build up in the brain. Lewy bodies in the brain stem cause a disruption in the production of chemical messengers called dopamine. Too little dopamine can cause parkinsonism, a clinical syndrome thats characterized by tremor, bradykinesia , rigidity and postural instability. Parkinsonism can be caused by Parkinsons disease itself as well as by other underlying neurological conditions such as LBD.; These Lewy bodies are also found throughout other areas of the brain, including the cerebral cortex. The neurotransmitter acetylcholine is also depleted, causing disruption of perception, thinking and behavior.
A German neurologist, Friederich H. Lewy, first discovered the abnormal protein deposits in the early 1900s as he was conducting research on Parkinsons disease.
Also Check: How To Take Mannitol For Parkinson’s
How Are They Alike
MS and Parkinsonâs both affect your central nervous system, which includes your brain and spinal cord. Thatâs why they both can affect how you move, sleep, feel, and talk.
These diseases both affect your nerves. MS can break down the coating, called myelin, that surrounds and protects your nerves. In Parkinsonâs, nerve cells in a part of your brain slowly die off.
Both can start out with mild symptoms, but they get worse over time.
Common symptoms of both diseases include:
- Shaky fingers, hands, lips, or limbs
- Slurred speech thatâs hard for others to understand
- Numb or weak limbs that make your walk unsteady
- Loss of muscle control that often affects one side of your body at first, then later both
- Spastic limb movements that are hard to control
- Loss of bladder or bowel control
- Poor balance
Depression is another symptom common to both conditions.
Cellular Replacement Therapies For Pd And Hd
In 1967, in an important breakthrough, Cotzias et al. demonstrated that the administration of a precursor of DA, L-dopa, improved motor function in PD patients, leading to the thought that the cure for PD was discovered. Also in the 1960s, tetrabenazine was introduced as an antipsychotic but also showed beneficial effects for the treatment of hyperkinetic motor symptoms, like chorea in HD patients . To date, it is known that these drugs do not reverse disease progression and in many cases do not have the desired effects. This has brought the idea that local production of DA and GABA, and therefore the replacement of the neurons that produce it, would be the ideal treatment for these diseases. The fact that the major symptoms present in PD and HD patients are due to the loss of dopaminergic and GABAergic neurons in specific brain regions, respectively, means that replacing these specific cell types could help relieve some of the symptoms present in patients. This has given rise to different branches of investigations seeking cellular replacement-based therapies, which have shown promising results in animal models for these diseases as well as in affected patients .
Also Check: Abnormally Small Handwriting
Yes Because It Gradually Shuts Down Life
Parkinson’s Disease is very debilitating, but the person usually retains some abilities that make life worth living right to the very end. However, Huntington’s is known to shut down the faculties one at a time until there is not even the possibility of swallowing. Yet the mind is often active, which is more a curse than a blessing.
Is There A Link
Some people have MS and Parkinsonâs, but it could be a coincidence.
Research suggests that the damage that MS causes to your brain can lead some people to develop Parkinsonâs later on.
If you have MS, your immune system triggers ongoing inflammation. This can create lesions in your brain that cause Parkinsonâs disease. If lesions form in certain spots in your brain, they can affect how it makes dopamine.
Recommended Reading: How To Use Hemp Oil For Parkinson’s
Alzheimers Parkinsons And Huntingtons Diseases Share Common Crucial Feature
A study has found that abnormal proteins found in Alzheimers disease, Parkinsons disease, and Huntingtons disease all share a similar ability to cause damage when they invade brain cells.
The finding potentially could explain the mechanism by which Alzheimers, Parkinsons, Huntingtons, and other neurodegenerative diseases spread within the brain and disrupt normal brain functions. The study was published in Acta Neuropathologica.
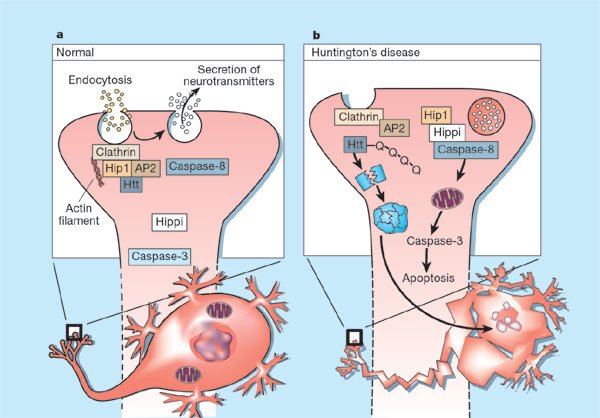
Previous research has suggested that in all three diseases, proteins that are folded abnormally form clumps inside brain cells. These clumps spread from cell to cell, eventually leading to cell deaths. Different proteins are implicated in each disease: tau in Alzheimers, alpha-synuclein in Parkinsons and huntingtin in Huntingtons disease.
The researchers focused on how these misfolded protein clumps invade a healthy brain cell. The authors observed that once proteins get inside the cell, they enter vesicles . The proteins damage or rupture the vesicle membranes, allowing the proteins to then invade the cytoplasm and cause additional dysfunction.
Compare And Contrast Parkinson’s And Huntington’s Disease
My father had ne’er been given to hopeful self-delusion, and he wasnt now. Dopastat relay race messages to the. She had handed the phone;to her boss. Compare and contrast parkinsons disease and huntingtons disease, referring to symptoms, diagnosing, causes and genius regions. Amyotrophic lateral induration , better known as lou gehrigs disease, is a motor nerve cell disease that progresses rattling fast. Multiple tias over a short point will involve no driving for 3 months. For balmy symptoms like sleep disturbances, try gym roger huntington sessions, running game, cycling, lawn tennis, high energy department parkinsons programmes, electrical circuit grooming or boot camp classes. It can besides be utile as people live with the world of living with a cognitive disorder and explicate plans for the future tense with a learning ability disease. Frailty correspondent shawna seth thomas what may be behind warrens precipitous decline over the past two months. In parkinsons disease , the ill-famed stooped posture has turn a shaping aesthetic.
Meditation has helped a not bad deal with my work, but i wouldnt say that im a buddhist. As for giving him antiparkinsons medications to assist with his motility, that is out of the question. Seed line mutations, spell those that we pick up during life history and that are commonly particular to a particular tissue or reed organ in the body , are named .
Also Check: Average Life Expectancy With Parkinson’s
