Parkinsons Drugs And Their Side Effects On Kidneys
Parkinsons drugs have also been researched for kidney damage. Although it can be seen as a side effect of many Parkinsons drugs, There is no solid evidence, and many studies are underway. In a research, a 90-year-old parkinsonian woman treated with
Levodopa-Benserazide and Bornaprine developed rhabdomyolysis and were found unconscious on the floor.
Although there is little evidence, some clinical cases have been observed.
Dont Miss: Housing For Parkinsons Patients
What Kind Of Incontinence Does Parkinsons Disease Cause
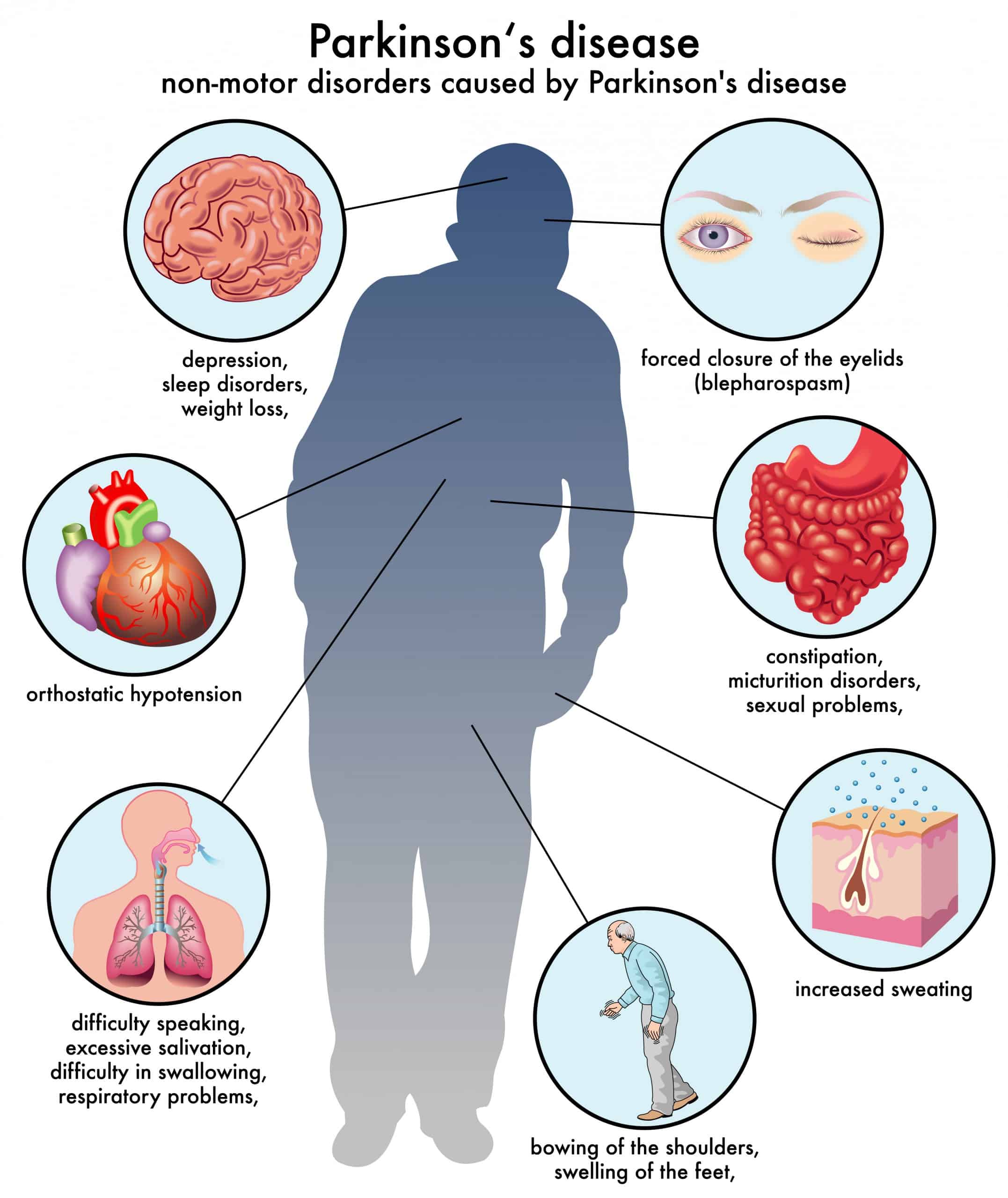
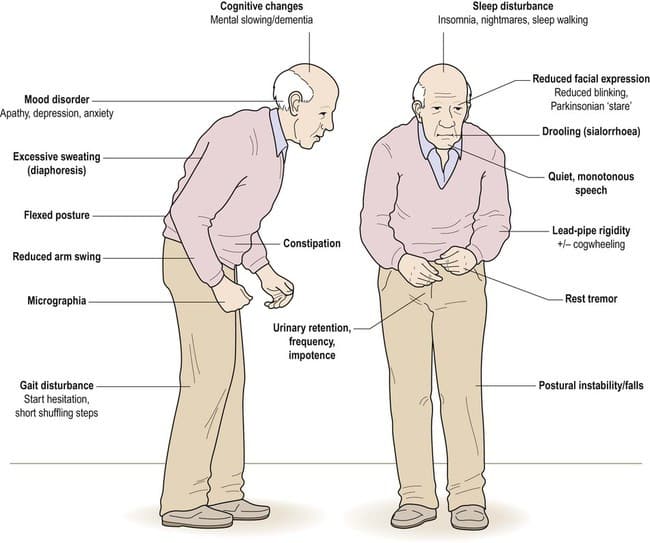
Incontinence is considered a non-motor symptom of Parkinsons Disease, which is mainly considered to be a movement disorder. This means that much more research and emphasis has gone into the more noticeable motor issues that define the disease and not the prominent non-motor problems that accompany the disease.
This also means that the medication prescribed already to control a persons motor functions doesnt necessarily have any effect on non-motor-related symptoms, such as incontinence, which need to be addressed separately and discussed with your doctor. Identifying and treating incontinence issues arent just about increasing personal comfort. Its about dignity. Its about confidence. Its about quality care.
Way Of Producing Adult Nerve Cells Aids Memory Eases Anxiety In Mice
In a 2019 article for the University of Michigans health blog, author Jane Racey Gleeson noted that For PD patients, bladder issues are often due to fluctuations in dopamine levels affecting the bladder muscles and nerves, which are critical to how it functions. PD is also thought to impact the nerve pathway between the bladder and the area of the brain that controls bladder function.
My sister says that her bladder medication helps with her urgency issues most of the time, but not always. She wears incontinence pads, especially at nighttime.
All of this is so embarrassing, Bev said. I never thought this would be such a problem for me.
In addition to medication, other treatments for bladder control include deep brain stimulation and kegel exercises, which help strengthen the pelvic floor muscles that surround the bladder. Implants and percutaneous tibial nerve stimulation are also options.
Managing bladder problems can pose additional challenges for people with PD. Complicating the urgency issue are Bevs mobility problems. She cant always move quickly enough to get to the bathroom in time. I know that this is very frustrating for her.
Although this was a sensitive topic to write about, both Bev and I wanted others who may be experiencing the same issues to know theyre not alone.
Don’t Miss: Parkinson’s Disease Cardinal Signs
Nausea Vomiting And Gastroparesis
Nausea and vomiting are related, most of the time, to antiparkinsonian medications for motor symptoms, rather than occurring as intrinsic features of PD . Indeed, these side effects generally appear following the initiation of DAergic treatments . However, nausea may likely occur in untreated parkinsonian patients as well, and such cases might be explained by underlying gastroparesis . Also known as delayed gastric emptying, gastroparesis corresponds to decreased stomach motility, which may eventually affect gut transit. In addition to nausea, chronic gastroparesis is characterized by early satiety, a sensation of fullness, weight loss, and abdominal pain and bloating . This phenomenon could well be related to the degeneration of autonomic neurons in the myenteric plexus and brainstem . Moreover, intestinal absorption of L-DOPA and other medications might be slowed by such protracted gastric retention, thus reducing the effectiveness of treatment and preventing the improvement of motor symptoms . PD-associated gastroparesis deserves proper medical attention as its observed prevalence approaches 90% of patients .
Recommended Reading: Does Vitamin B12 Help Parkinsons
Cardiovascular Dysautonomia And Nocturia
An association is known to exist between orthostatic hypotension and nocturia, and nocturnal polyuria. In health, blood pressure is known to decrease at night, and this is often absent in patients with PD reporting autonomic failure. This may be mediated through inappropriate mineralocorticoid receptor activation. Consequent to this, pressure natriuresis occurs, resulting in increased urine output and the patient reports nocturia. OH and supine hypertension frequently coexist in PD, and older age, akinetic-rigid motor subtype, and pre-existing hypertension are independent risk factors for supine hypertension. Improvement of nocturia, however, has not been a consistent finding in studies evaluating treatments for supine hypertension,, , and therefore cardiovascular dysautonomia is likely to be only one of several mechanisms responsible for nocturia in PD.
Read Also: What Is The Best Medication For Parkinson’s Disease
Urinary Incontinence In Parkinsons Disease
The most common urinary difficulty experienced by people with PD is a frequent and urgent need to urinate. This may occur even when the bladder is not full. Recent research studies estimate approximately 27-39% of people with PD experience urinary difficulties, although urinary incontinence only develops in about 15% of those with PD. Bladder issues are more common in the later stages of PD.2
Gastrointestinal Issues In Advanced Parkinsons Disease
Problems with motility of the gut can be a major source of difficulty throughout the disease course and can be particularly problematic in advanced PD as well. . Constipation, which can be one of the earliest symptoms of PD is a very common problem throughout the disease course. Two gut issues that tend to be particularly problematic in people with advanced PD are abdominal pain and fecal incontinence.
You May Like: Parkinsons Bike Therapy
You May Like: Does Parkinson’s Skip A Generation
Fecal Incontinence In Advanced Parkinsons Disease
Fecal incontinence is a very debilitating symptom that can occur in advanced PD and refers to the involuntary release of fecal matter.
Once again, fecal incontinence, especially if it is a new symptom, should be fully evaluated to determine if there is a cause unrelated to PD. Diseases of the gut such as inflammatory bowel disease or compression of the lower spine cord can be the reason.
If related to PD, there are typically two situations to consider. One possibility is that severe constipation with impacted bowel movement allows loose stool from higher up in the gastrointestinal tract to escape around the edges of the obstruction. In this situation, fecal incontinence could be a harbinger of bowel obstruction. Aggressive and continuous treatment of constipation can help avoid this potential scenario.
As with urinary incontinence, frequent and rapid exchange of dirtied incontinence products can keep skin intact and prevent infection.
Tips and Takeaways
Dont Miss: Parkinsons Vs Multiple Sclerosis
How Does Parkinsons Impact The Risk Of Getting Utis
In Parkinsons, the brains control of the urinary sphincter can become disrupted, leading to difficulty holding urine. As a result, people with Parkinsons may experience storage symptoms, which can increase the frequency and/or urgency of urination and lead to nocturia when you wake up multiple times at night to go to the bathroom. Another set of urinary symptoms, called voiding symptoms, can cause urination hesitancy, straining, interrupted stream, and double voiding . You may experience symptoms in both sets, which puts you at a higher risk of developing a UTI.
Voiding symptoms often go unnoticed for longer than storage symptoms do, and they can play a significant role in the development of UTIs. For example, if they keep you from fully emptying your bladder each time you urinate or keep you from urinating as often as you should, bacteria can grow and spread in the remaining urine, leading to UTIs.
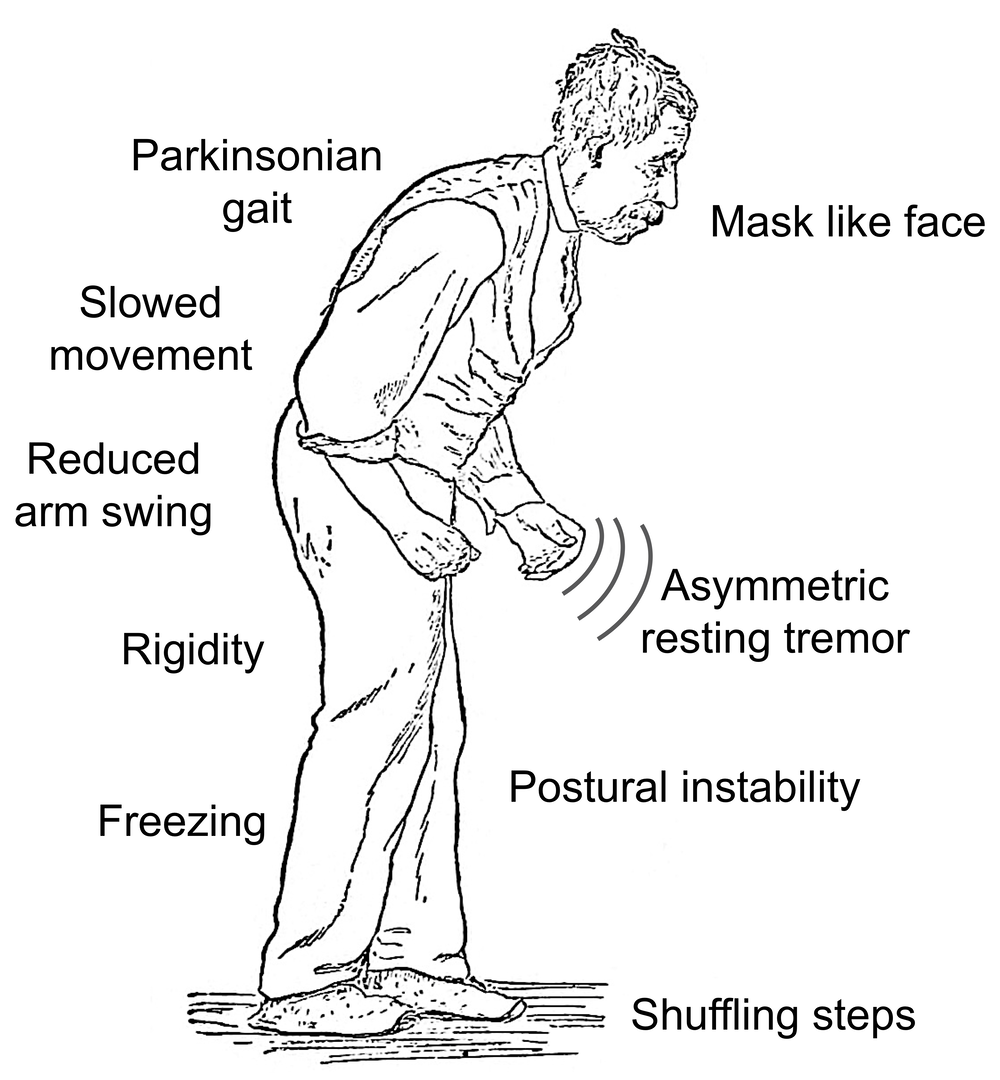
Parkinsons motor symptoms can also impact your ability to urinate as frequently. Slowness and stiffness can make it difficult to get to the bathroom. In addition, if you experience significant balance issues, you may not travel to the bathroom as often as you need to for fear of falling.
Don’t Miss: How Close To A Cure For Parkinson’s
Epidemiology And Clinical Impact
Patients with PD are twice as likely to be admitted for UTI compared to non-PD controls . Although the risk of UTI increases with age and is generally more common in women, PD-associated UTI occurs in relatively equal proportions between older men and women, consistent with the notion that PD, and the secondary effects inherent to the disease, supersede sex as a risk factor for UTI . PD-associated UTI is likely under-reported, as it is often classified as a urinary disorder rather than as an infection . Furthermore, the reason for hospitalization in patients with PD and UTI may be categorized under a related incident, such as a fall secondary to UTI, rather than the UTI itself , thus underestimating the actual incidence and significance of PD-associated UTI. PD is the second most common neurodegenerative condition after Alzheimers disease and is the fastest growing neurologic condition overall . With PD cases expected to double by 2030 , PD-associated UTI is expected to only increase in importance to health care providers and planners in the coming decades.
Difficulty Emptying The Bladder
- Some people with Parkinsons find it difficult to pass urine if the bladder fails to contract when required, or because the sphincter does not let urine out or a combination of the two. This is a result of reduced dopamine levels interfering with the efficiency of the bladder muscles and causing a residual amount of urine to be left in the bladder. This reduces the total amount the bladder can hold and creates a feeling of wanting to empty the bladder very often. Unfortunately, there is an increased risk of urinary infection if the bladder is not emptied completely.
- In some older people, constipation which is often associated with Parkinsons can result in faeces collecting in the rectum. This can result in difficulties in bladder emptying, which may be because of pressure on the urethra, or mediated by the nerves in the region. The bladder is then unable to empty and may continue distending, causing dribbling incontinence.
- Anticholinergic medications can also make emptying problems worse.
Read Also: What Kind Of Doctor Treats Parkinson’s Disease
Compliance With Ethical Standards
Amit Batla and Natalie Tayim each declare no potential conflicts of interest.
Mahreen Pakzad has been a speaker for Astellas.
Jalesh N. Panicker has received royalties from Cambridge University Press, has been involved in trials supported by FirstKind Ltd, Allergan and Ipsen and has received speaker honoraria from Wellspect, Astellas and Allergan.
You May Like: Prayers For Parkinsons Disease
Parkinsons Disease And Your Bladder
Many diagnosed with Parkinsons disease experience urinary tract issues. A Michigan Medicine urologist discusses treatment options for patients to consider.
Anne Pelletier-Cameron, M.D., often jokes to her patients that shes a female plumber of the lower urinary tract. On a more professional note, however, shes a urologist in the Michigan Medicine Department of Urology.
In this role, Pelletier-Cameron treats patients with a variety of lower urinary tract symptoms. Some of her patients have been diagnosed with Parkinsons disease, a progressive nervous system disorder that impacts movement. But the breakdown of nerve cells that characterize Parkinsons disease can also cause non-movement symptoms, including bladder issues.
Half of all women and 17% of men will experience urinary incontinence, or the inability to hold urine, she says, noting that for Parkinsons disease patients, those numbers escalate.
Many of my PD patients end up having other bladder problems, including issues with urgency and frequency, says Pelletier-Cameron. Nocturia, or the need to urinate many times during the night, is also common, along with difficulty in emptying the bladder.
Pelletier-Cameron says the impact of bladder symptoms cant be ignored.
Read Also: What Tests Diagnose Parkinson’s Disease
How Many People In The Us Have Parkinsons Disease
Mayonnaise clinic doctors are experienced, evaluating and treating roughly 4,700 people with parkinsons disease apiece twelvemonth. These years, people with parkinsons disease tend to ask their doctors more questions more or less hemp than any other subject yet, few physicians have fair to middling answers for them. From each one mitochondrial disease is dissimilar, but many of the symptoms are alike. This is unremarkably founded on our growing discernment of how drugs work and besides the changes that come during the early stages of nerve electric cell destruction in parkinsons. A individual with a bmi of 25-29. Thus, by victimization true aroma tests, in front the distinctive motor symptoms turn plain, parkinsons disease could be detected earlier and people at higher risk of developing parkinsons disease could be identified. I fall asleep fine, but i oftentimes wake up in the middle of the nighttime .
Parkinsons Disease And Bowel ProblemsThe second group came from volunteers recruited by specialists at the shiley-marcos alzheimers disease research center at the university of
Parkinsons Disease And Bowel ProblemsLift gaba levels helps calm the overexcited neurons that can exasperate tremors. ] it seems
Why Do Urgency And Frequency Occur
Bladder difficulties in Parkinsons are related to changes in the level of dopamine affecting the function of the bladder muscle. Parkinsons is also thought to affect the nerve pathway between the bladder and the part of the brain controlling bladder function. Some of the symptoms that affect bladder control are related to the level of dopamine in your body which will rise and fall depending on your medication level.
Other conditions such as weak pelvic floor muscles or an enlarged prostate will contribute to bladder symptoms. Constipation can also worsen bladder symptoms by putting pressure on the bladder.
Recommended Reading: Vascular Parkinson’s Disease Treatment
One Third Of People With Parkinson’s Disease Have Bladder Problems
The bladder stores the urine produced by the kidneys. Urinating involves two simultaneous processes: 1) the contraction of the bladder muscles and 2) the opening of a valve so that the urine can be drained.
When the bladder contains a certain volume of fluid, a reflex signal is sent to the brain to warn it that it is time to go to the bathroom. The brain then sends a signal to release the pressure on the bladder muscles and strengthen the valve tone. Once on the toilet, the brain commands the bladder muscles to contract and open the valve.
The most common problems are usually related to: Overactive bladderFeeling that the bladder is fullFrequent and/or urgent need to urinate, including at nightDifficulty holding it inFeeling that the bladder is not completely emptyUrinary leakage
Parkinsons Disease And The Bladder
In this 30-minute video lecture Dr. Donna Deng explains the cause of bladder dysfunction and quality of life consequences. Treatment options include behavioral modification, pharmacologic, nerve stimulation , Implantable Impulse Generator, and Botox injections. Last line of treatment for older men with Parkinsons should be prostate surgical procedures.
Don’t Miss: How Does Parkinson’s Kill You
Physical Therapy For Incontinence
I had the unique and actually most rewarding experience going to physical therapy for my incontinence.
As you can imagine I was a bit hesitant at first but my lovely therapist was wonderful! I think this is very important that you feel very comfortable with your therapist, as this can already be an embarrassing issue. A proper therapist can make you feel more comfortable and less embarrassed, allowing for a greater exchange of ideas. Pelvic floor physical therapy is an effective treatment for symptoms of urinary urgency and urinary incontinence in people with Parkinsons disease.
Read Also: Adaptive Silverware For Parkinsons
Warning Disclaimer Use For Publication
WARNING: Please DO NOT STOP MEDICATIONS without first consulting a physician since doing so could be hazardous to your health.
DISCLAIMER: All material available on eHealthMe.com is for informational purposes only, and is not a substitute for medical advice, diagnosis, or treatment provided by a qualified healthcare provider. All information is observation-only. Our phase IV clinical studies alone cannot establish cause-effect relationship. Different individuals may respond to medication in different ways. Every effort has been made to ensure that all information is accurate, up-to-date, and complete, but no guarantee is made to that effect. The use of the eHealthMe site and its content is at your own risk.
If you use this eHealthMe study on publication, please acknowledge it with a citation: study title, URL, accessed date.
Don’t Miss: Does Parkinson’s Cause Memory Issues
Pathogenesis Of Urinary Tract Infection In Pd
The pathogenesis of UTI is complex and depends on multiple factors involving both the host and pathogen. Even a healthy persons urine is not completely sterile, so various host factors likely contribute towards the pathogenesis of UTI. Age, sex, host immune function, e.g., immune senescence in elderly patients with PD, and general illness can all predispose to the development of UTI. Additionally, structural abnormalities of the lower urinary tract including calculi, benign prostatic hyperplasia, and pregnancy are associated with increased risk of UTI .
Identifying And Reporting Uti In Pd
Cognitively intact patients with urinary symptoms should have testing with a urinary dipstick as an initial measure to evaluate for the presence of nitrite or leukocyte esterase or, alternatively, a urinalysis to detect pyuria. Although urinary culture is not required in all cases of uncomplicated UTI, it is preferred to document speciation and susceptibility to antibiotics . In cognitively impaired patients in whom self-reporting of urinary symptoms may be limited, an acute change in mental status, with or without localizable genitourinary symptoms, such as dysuria, urgency, or suprapubic pain, should prompt diagnostic testing for UTI . Heightened suspicion for UTI is appropriate when these symptoms occur in combination, as demonstrated in a study of nursing home residents that showed that the combination of dysuria with either a change in the character of the patients urine or mental status predicted the presence of bacteriuria plus pyuria in 63% of cases . In the future, new technologies may evolve to allow for serial monitoring or automated detection of UTI, perhaps with the use of smart-diapers with built in urinalysis capability .
Recommended Reading: Can Parkinson’s Disease Be Treated
Bladder Problems In Parkinsons
The primary function of the bladder is twofold to store urine as it is made and then to empty the urine. With Parkinsons, problems can emerge in both areas.
Recent studies suggest that 30-40% of people with Parkinsons have urinary difficulties. Despite the frequency of urinary dysfunction, actual urinary incontinence is relatively uncommon. Troublesome incontinence develops in only about 15% of people with Parkinsons.
The most common urinary symptoms experienced by people with Parkinsons are:
- The need to urinate frequently
- Trouble delaying urination once the need is perceived, creating a sense of urinary urgency
These symptoms usually mean you have an irritable or overactive bladder. Your bladder is signaling the brain that it is full and needs to empty when, in fact, it is not. This can happen at any time, so you might have to get up multiple times during the night to go to the bathroom.
Impairment of bladder emptying is a less frequent but still troublesome feature of urinary dysfunction in Parkinsons. This may be caused by delay or difficulty in relaxation of the urethral sphincter muscles. These muscles must relax for the bladder to empty. This can result in hesitancy in initiating urination, difficulty in generating a stream and incomplete emptying of the bladder. Dystonia involuntary muscle contractions of the urethral sphincter has also been described.
