How Physical Therapy Can Help
A physical therapist will complete a thorough evaluation of your mobility including balance, walking, strength, and endurance. In-person and virtual sessions will be scheduled to help assist with your rehabilitation journey.
A physical therapist can help with:
- education and self-management advice
- exercise routines to improve balance, walking, prevention of falls and what to do if you fall
- mobility around the house and community
- using assistive devices for mobility such as canes, walkers, or hiking poles
- Freezing what to do and prevention
- cognitive executive function
Recommended Reading: Young Onset Parkinsons Support Group
What Can You Do About Trigger Points That Might Be Interfering With Respiration
Muscle trigger points are unpredictable and mysterious: exactly what they are and how to treat them is controversial. Sometimes they seem to melt as easily as ice cream in the sun, and so the first thing to try is just a little simple self-massage, or a warm bath, or both. The problem could be solved by a self-treatment as simple as digging with your thumbs into some aching muscles between your ribs. Voila no more shortness of breath! Ive seen it go like that many times, and even experienced it myself
My story: I am generally prone to muscle pain, and one of the most persistent specific challenges Ive had is with breathing pain not shortness of breath in my case, but breathing limited by pain. For about twenty years, I had routine episodes of strong pain that choked off my breath. Once every few days, I would be nearly paralyzed by it for several minutes, and sometimes nightmarish episodes of an hour or more. The pain would ease when I relaxed for long enough but its hard to relax when you cant breathe.
I recovered! I experimented with self-massage of my intercostals, discovered that I could easily stop any attack of this pain within a minute just by rubbing between the ribs near the pain.11 It was a revelation. Ive probably never been so happy to learn anything! Over a year or two, I massaged my intercostals regularly until I stopped having these episodes at all, and that benefit has now persisted for many years.
Recommended Reading: Diseases Similar To Parkinsons
Could This Be Due To Parkinsons Disease Uncommon Non
It is common for a person with Parkinsons disease to attribute every new symptom that develops to PD. That is largely because the list of non-motor symptoms commonly associated with PD is so varied, it can seem that almost anything is a symptom of PD! But if you take a closer look, there are some symptoms that are very commonly associated with PD, others that are virtually never associated with PD, and some in between.
Lets divide up non-motor symptoms into the following categories:
You May Like: Parkinson’s And Sleep Disorders
Breathing Problems And Parkinsons Disease
Usually, trouble breathing is not thought of as a symptom of PD. Those with PD who complain of this will typically have testing of their heart and lung function. This is necessary since, as we continue to emphasize, a person with PD can develop medical problems unrelated to PD and needs every new symptom evaluated like someone without PD. However, often the testing does not reveal a cardiac or pulmonary abnormality. Could difficulty breathing be a symptom of PD itself?
There are a number of ways in which difficulty breathing may be a symptom of PD:
Shortness of breath can be a wearing-OFF phenomenon
Some non-motor symptoms can fluctuate with brain dopamine levels, which means that they change as a function of time from the last levodopa dose. For some people, shortness of breath can be one of the non-motor symptoms that appears when medication levels are low. However, shortness of breath can be due to anxiety which can also be a wearing-OFF phenomenon. Sometimes it is not possible to determine whether the key symptom is anxiety or shortness of breath. Treatment involves changing medication dosing and timing so that OFF time is minimized. You can view this webinar which discusses the concept of wearing OFF and potential treatments.
Abnormal breathing can be a type of dyskinesia
Restrictive lung disease
Aspiration pneumonia
Sleep apnea
Origins Of Breathing Disorders
The book by Leon Chaitow and co-authors cited above explains how breathing disorders are intrinsically linked to chronic stress and anxiety. The shallow, fast chest breathing through the mouth is a hallmark of the body preparing itself for the exertion of flight or fight due to a stress response. While this adaptive in acute stress situations, when stress is chronic and the body is spending a lot of time in fight or flight, the associated pattern of breathing becomes habitual, and eventually the system gets stuck in the new equilibrium of the CO2 intolerant state. However, the vicious circle work both ways, because overbreathing itself puts the body into a stress response state and feeds anxiety. A very good tutorial about the two way links between anxiety and breathing patterns is given by Robert Litman in the video below.
It is not surprising therefore that people with PD can present with disordered breathing associated with chronic stress and anxiety, since there are very significant overlaps between the other symptoms of chronic stress and those of Parkinsons Diseases, and ingrained fight or flight behaviours are common to the pre-diagnosis background histories of people with PD. Conversely, it is important to note that techniques which have been developed to treat breathing disorders should also help to decrease the symptoms of PD, including reduction of anxiety and increasing resilience to stress.
Read Also: What Does Idiopathic Parkinson’s Disease Mean
The Issue Of Pneumonia In Parkinson’s Disease
Aspiration pneumonia represents a dramatic complication that may explain the acute/subacute onset of fever and respiratory insufficiency in a PD patient. Physiologically, swallowing requires adequate coordination between pharyngeal and respiratory musculature, but this mechanism is frequently impaired in PD . Dysphagia is typical in the advanced stages of disease, on average 1011years after motor symptoms onset , when bradykinesia, rigidity and dyskinesias are predominant however, a cough dysfunction in more than 50% of asymptomatic PD patients has been demonstrated and this may also contribute to silent aspiration and increased risk of pneumonia . Moreover, in these patients the cough mechanism becomes weak because of cough reflex impairment and chest wall rigidity, further increasing the risk of aspiration . A blunted urge to cough , a respiratory sensation that precedes the cough reflex, is also present and correlates with the severity of dysphagia and consequently, with an increased risk of aspiration .
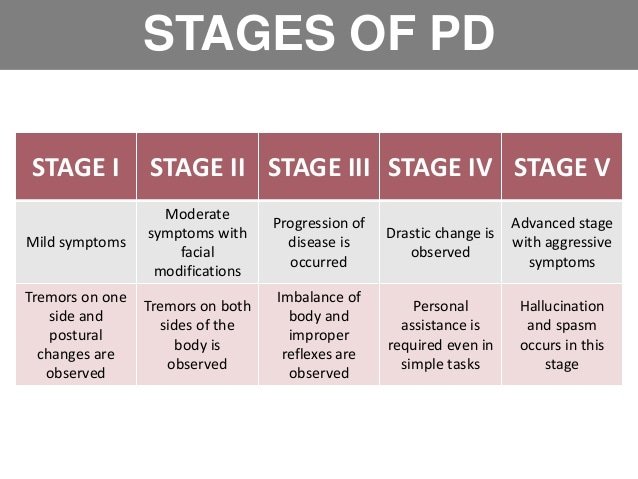
Parkinsons Diseasesigns And Symptoms
Parkinsons generally progresses slowly, sometimes taking years for symptoms to appear. The disease usually strikes adults over age 50, although it has been diagnosed as early as age 20. About 15 percent of Parkinsons patients have a family history of the disease.
Because it develops gradually, most people have many years of productive living after being diagnosed.
Some of the first symptoms commonly experienced with Parkinsons include the following:
- Rigidity Arms and legs become stiff and hard to move
- Tremors Rapid shaking of the hands, arms or legs
- Slowed movements Difficulty starting or completing movements, called bradykinesia
- Impaired balance Lack of balance or difficulty adjusting to sudden changes in position
These symptoms may make it difficult for you to walk, pick up and hold things, eat, write, or react quickly to prevent injury if you fall.
Other symptoms include difficulty speaking or swallowing, drooling, stooped posture, inability to make facial expressions, oily skin, cramped handwriting, shortness of breath, constipation, increased sweating, erectile dysfunction, difficulty sleeping, problems urinating and anxiety.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Read Also: What Are The Main Symptoms Of Parkinson’s Disease
Strength Training Helps Build Muscle Mass
Strength training can involve lifting weights, using machines at the gym, using your own body weight for resistance, or even using common household items like a milk jug filled with sand, the Parkinsons Foundation notes. Your strength training should focus on the following muscle groups:
- Hands and wrists
In general, strength training should be done two to three times per week, but scheduled so that youre not targeting the same muscles on consecutive days, as your muscles need to rest and recover, the foundation advises.
As with stretching exercises, strength training can be performed while standing, sitting, or while on the ground.
The Wisconsin Parkinson Association recommends several exercises to help strengthen your grip and improve your reach. Tasks such as handwriting and reaching for items on higher shelves can be a challenge for people with Parkinsons disease, and hand exercises can help minimize these issues.
In general, resistance training helps build and maintain muscle mass, Subramanian says. The stronger you are, the more independent youll be.
Respiratory Disorders Of Parkinsons Disease
Parkinsons disease is characterized by the progressive loss of dopaminergic neurons in the substantia nigra, mainly affecting people over 60 yr of age. Patients develop both classic symptoms and nonclassical symptoms . Thus, patients with PD can have a significantly impaired quality of life, especially when they do not have multimodality therapeutic follow-up. The respiratory alterations associated with this syndrome are the main cause of mortality in PD. They can be classified as peripheral when caused by disorders of the upper airways or muscles involved in breathing and as central when triggered by functional deficits of important neurons located in the brainstem involved in respiratory control. Currently, there is little research describing these disorders, and therefore, there is no well-established knowledge about the subject, making the treatment of patients with respiratory symptoms difficult. In this review, the history of the pathology and data about the respiratory changes in PD obtained thus far will be addressed.
Read Also: Does Sugar Affect Parkinson Disease
Deep Brain Stimulation And Respiratory Failure
DBS is an effective strategy for the treatment of advanced PD, thus improving motor fluctuations and bradykinesia.
Nonetheless, the classical target of the subthalamic nucleus -DBS reserves stimulation-induced side effects in the long-term period, comprising gait and speech impairment, as well as a progressively worsening of tremor. In this scenario, only few papers have specifically investigated respiratory failure. In particular, STN-DBS may increase the risk of a fixed epiglottis and modify velopharyngeal control these effects seem to strictly depend on frequency parameters, with low-frequency stimulation leading to a clinical improvement, whereas higher frequencies are associated with a detrimental effect on velopharyngeal control .
In support of this view, Hammeret al. have recently found that in STN-DBS patients, respiratory changes do not correlate with limb function, but speech-related respiratory and laryngeal control may benefit when the stimulation is delivered at low frequencies and shorter pulse width . In addition to stimulation frequency, other factors may account for these correlations, including variability in localisation of the active DBS electrodes, individual variability in somatotopic organisation of STN, stimulation fields and potential current spread beyond the STN target . Data on the relationship between respiratory changes and novel DBS targets, such as the pedunculopontine nucleus , have not been extensively reported so far.
What Are The Causes
People with Parkinsons may experience varied respiratory symptoms, ranging from shortness of breath without exertion to acute stridor, the sudden onset of high-pitched breathing sounds when taking a breath.1,3
Dysfunction can be caused by a variety of factors including physiological restrictive changes in the lungs, upper airway obstruction, and response to medications.1,3
Read Also: What Happens When Parkinson’s Medication Stops Working
Relaxation With Guided Imagery
During guided imagery, a person is given ideas and images to mentally focus on while they are relaxing and breathing deeply.5
One study evaluated the benefit of relaxation with guided imagery in people with PD. Researchers found that the tremor from PD is more pronounced during stress. During the study, some people were given guided imagery meditations. Others listened to relaxing music. A third group was encouraged to self-relax.5
The group of people who experienced the guided meditation all had a decrease in their tremor. The improvement continued for several hours. The group of people who listened to relaxing music had a slightly reduced tremor. The group who self-relaxed had no significant effect on their tremor. These findings suggest that guided imagery can supplement traditional medical treatment for tremor in people with PD.5
You May Like: Zhichan Capsule
Shortness Of Breath Could Indicate Early Signs Of Parkinsons Disease Say Experts

Home»BlogHome » Shortness of breath could indicate early signs of Parkinsons disease, say experts
Changes in the way you breathe, such as shortness of breath and shallow breathing, could be an early sign of Parkinsons disease, experts have warned.
The symptom which may be confused with a symptom of the coronavirus forms one of the major indicators of the disease which progressively damages the brain over a period of time.
According to the Parkinsons Foundation, shortness of breath could be attributed to respiratory dyskinesia, anxiety, or aspiration pneumonia, which are all associated with the disease.
Some people with Parkinsons disease may experience shortness of breath. There is no clear cause underlying respiratory dysfunction in PD, its frequency or the effect that medications have on respiration, says the Foundation.
Shortness of breathing may be accompanied by a number of other early indicators, the charity warns. These include tremors in your finger, thumb, hand, or chin, smaller handwriting, loss of smell, trouble sleeping, trouble moving or walking, dizziness or fainting, or poor posture.
It can be hard to tell if you or a loved one has Parkinsons disease , said the Foundation.
No single one of these signs means that you should worry, but if you have more than one sign you should consider making an appointment to talk to your doctor.
For advice on the care and support of a loved one, please get in touch with our expert team today.
You May Like: What Is Parkinsons Disease Nhs
Hazel Cavanagh Traumatic Brain Injury
The right support at the right time can make a huge difference to someone with complex care needs. Thats something that Hazel Cavanagh knows from first-hand experience, after Almond Care provided round the clock support during the last four months of her husband Johns life. She says: The support given by Almond Care helped toRead moreHazel Cavanagh Traumatic brain injury
Central Case Management Brain Injury
Central Case Management has a clear focus: ensuring brain injury clients have the support that will help them work towards achieving their own goals and a better quality of life. The company, based in Duffield, Derbyshire, works with a range of brain injury professionals in creating and delivering bespoke support and rehabilitation to its clientsRead moreCentral Case Management Brain injury
Also Check: How Long Can A Person Live With Parkinson’s Disease
Medical Recognition Of Breathing Disorders
The existence of these breathing disorders have been known about, but largely ignored, in medical circles, for decades. Indeed, L.C. Lum, a cardiologist at Papworth & Addenbrookes Hospitals, Cambridge, UK, wrote an article on this entitled Hyperventilation: the Tip of the Iceberg in 1975. Here are some relevant excerpts:
“…this syndrome… shows up in medical clinics under many other guises. This is merely the tip of the iceberg the body of the iceberg, the ninety nine per cent who do not present , presents a collection of bizarre and often apparently unrelated symptoms, which may affect any part of the body, and any organ or any system. The many organs involved are often reflected in the number of specialists to whom the patient gets referred, and my colleagues have variously dubbed this the multiple doctor or the fat folder syndrome. Indeed the thickness of the case file is often an important diagnostic clue.”
Lum lists many symptoms, many of which are also common in PD: palpitations, disturbance of consciousness/vision, shortness of breath. “asthma” chest pain, dysphagia, muscle pains, tremors, tension, anxiety, fatigability, weakness, exhaustion, sleep disturbance nightmare, constipation, diarrhea, twitching eyelids, headache, giddiness, difficulty in breathing, weak limbs, painful limbs, vague pain, weakness, irritability, insomnia.
Effects Of Dopaminergic Therapy: Risk Or Protection
Studies have provided controversial results about the therapeutic effects of dopaminergic stimulation, and the role of drugs commonly used in the treatment of PD is still debated, strictly depending both on disease stage and administration modality.
Most papers strengthen the role of anti-Parkinsonian drugs as a protective factor against the development of respiratory failure. Levodopa increases inspiratory muscle function in anaesthetised dogs , and dopamine improves diaphragm function during acute respiratory failure in patients with COPD . In early stages, the levodopa equivalent daily dose does not correlate with pulmonary functional testing as the disease progresses, anti-Parkinsonian medications may be responsible for the maintenance of the maximal inspiratory mouth pressure and sniff nasal inspiratory pressure . Accordingly, bedtime controlled-release levodopa is associated with less severe obstructive sleep apnoea in PD . Because dopamine is not known to increase muscle strength, it may ameliorate respiratory function by improving muscle coordination by a central activity .
Many authors have investigated the effect of dopaminergic therapy on aforementioned respiratory dysfunction, especially on obstructive and restrictive patterns .
Main findings of major studies we considered about the effects of dopaminergic drugs on respiratory parameters and respiratory dysfunctions
Dont Miss: Parkinsons Hallucinations Commercial
You May Like: Tell Me About Parkinson’s
Other Symptoms To Spot For Potential Early Warning Signs
A telltale sign you have Parkinson’s is slight shaking or tremor in your thumb, finger, hand or chin, the health site says.
It adds: “A tremor while at rest is a common early sign of Parkinson’s disease.”
It is worth noting that a person with Parkinson’s disease can also experience a wide range of other physical and psychological symptoms.
According to the NHS, these include depression and anxiety, balance problems , loss of sense of smell , problems sleeping and memory problems.”
