Genetic Testing For Huntington Disease
|
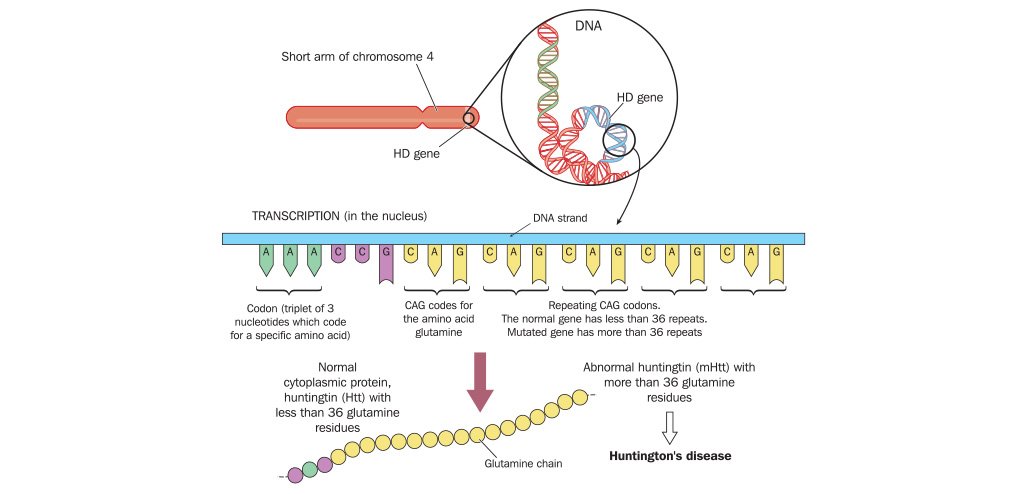
The genetic mutation that causes Huntington disease is located on chromosome 4. It involves repetition of a particular section of the genetic code in the DNA. The gene for Huntington disease is dominant. Thus, having only one copy of the abnormal gene, inherited from one parent, is sufficient to cause the disease. Almost all people with the disease have only one copy of the abnormal gene. Children of such people have a 50% chance of inheriting the abnormal gene and thus the disease. People who have a parent or grandparent with Huntington disease can find out whether they have inherited the gene for the disease by taking a genetic test. For the test, a blood sample is taken and analyzed. Such people may or may not want to know whether they have inherited the gene. This issue should be discussed with an expert in genetic counseling before genetic testing. |
Cause Signs And Symptoms Treatment And Management Age Of Onset Of Parkinsons And Huntingtons Disease:
Cause:
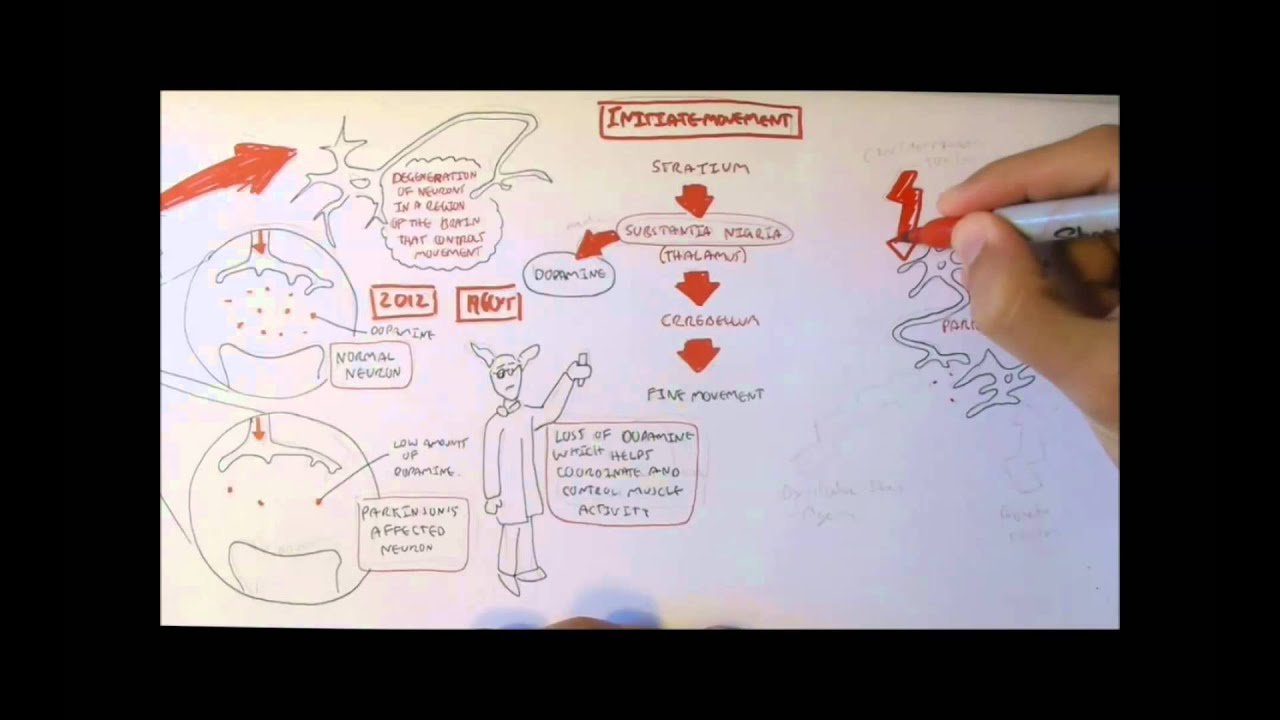
Parkinsons Disease: PD is caused by the degeneration of the neurons in Substantia nigra of the midbrain.
Huntingtons Disease: HD is caused by the mutations in the HTT gene.
Age of Onset:
Parkinsons Disease: PD usually occurs after the age of 50.
Huntingtons Disease: HD usually occurs in the thirties or forties.
Symptoms:
Parkinsons Disease: PD causes tremors, rigidity, slowing of movements and gait disturbances.
Huntingtons Disease: HD causes higher function abnormalities such as problems in thinking and reasoning together with characteristic chorea.
Treatment:
Parkinsons Disease: PD is treated with dopamine-enhancing drugs such as levodopa, dopamine agonists, etc.
Huntingtons Disease: HD has no curative treatment and main the treatment is supportive.
Life expediency:
Parkinsons Disease: PD doesnt have an effect on life expectancy. However, it reduces the quality of life.
Huntingtons Disease: HD patients live 15-20 years after the appearance of the first symptom.
Cellular Replacement Therapies For Pd And Hd
In 1967, in an important breakthrough, Cotzias et al. demonstrated that the administration of a precursor of DA, L-dopa, improved motor function in PD patients, leading to the thought that the cure for PD was discovered. Also in the 1960s, tetrabenazine was introduced as an antipsychotic but also showed beneficial effects for the treatment of hyperkinetic motor symptoms, like chorea in HD patients . To date, it is known that these drugs do not reverse disease progression and in many cases do not have the desired effects. This has brought the idea that local production of DA and GABA, and therefore the replacement of the neurons that produce it, would be the ideal treatment for these diseases. The fact that the major symptoms present in PD and HD patients are due to the loss of dopaminergic and GABAergic neurons in specific brain regions, respectively, means that replacing these specific cell types could help relieve some of the symptoms present in patients. This has given rise to different branches of investigations seeking cellular replacement-based therapies, which have shown promising results in animal models for these diseases as well as in affected patients .
You May Like: Can Parkinson’s Run In The Family
Living With Huntington Disease
As Huntington disease progresses, you will need constant assistance and supervision because of the debilitating nature of the disease. People usually die from the disease within 15 to 20 years of developing symptoms.
If you have been diagnosed with, or are at risk for Huntington disease, it is critical to maintain your physical fitness as best you can. People who exercise regularly and stay active tend to do better than those who dont.
A number of studies are currently under way to examine possible therapies for Huntington disease. Talk with your health care provider about whether any of these therapies may be helpful to you or a loved one with the disorder.
Som Biotech Announces A Presentation Of The Phase 2 Clinical Results Of Som3355 For The Treatment Of Chorea In Huntingtons Disease
SOM Biotech will present results from the Phase 2 clinical study of SOM3355 for the treatment of chorea symptoms in Huntington´s disease at the XXVI World Congress on Parkinsons Disease and Related Disorders, to be held May 1st 4th 2021.
The International Association for Parkinsonism and Related Disorders has accepted the abstract for the poster presentation at the IAPRD Congress 2021. The abstract is entitled Proof-of-concept study testing SOM3355 as a VMAT2 inhibitor to treat chorea symptoms in Huntingtons disease and outlines data demonstrating that SOM3355 reduces chorea safely and efficaciously.
Aileen Ferré, SOM3355 Project Leader at SOM Biotech highlights: We are pleased to share our findings on the efficacy of SOM3355 for the treatment of chorea movements in HD. Huntingtons chorea is a devastating condition. The involuntary abrupt movements mostly affect the arms and legs and facial muscles at even the early stages of the disease but also interferes with speech, swallowing, and other motor activities which adversely affects daily living and working. Finding an effective treatment for chorea is essential to help patients improve their quality of life.
You May Like: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Activation Pattern In Control Subjects
The pattern of brain activation induced by unilateral high-frequency passive vibratory stimulation in our control cohort is in keeping with previous PET data on elementary somatosensory function, as reviewed recently by Paulesu and colleagues . Our study confirms that this rather crude sensory stimulus produces strong activation in cortical areas S1 and S2. The pattern of normalized group rCBF increases in our study was markedly lateralized to the contralateral hemisphere, similar to previous reports . Transcallosal connections have, nevertheless, been demonstrated in posterior S1 , adjoining parietal cortex and secondary sensory cortical areas and, likewise, previous PET and functional MRI experiments have provided evidence for bilateral sensory cortical processing in humans. However, it remains an issue of further inquiry with higher temporal resolution imaging modalities, how ipsilateral sensory area recruitment is affected by habituation and/or other task-related issues. For instance, evoked potential recordings in cats indicate that habituation occurs more rapidly in S2 compared with S1 areas .
What Are The Complications Associated With Chorea
Depending on the cause of chorea, complications can be severe. Huntingtons disease is an ongoing disease that gets worse over time and has no cure. Although there is no cure for lupus, doctors can help you manage the disease with medications. Children who develop Sydenham chorea after rheumatic fever usually recover without long-term medical problems.
Also Check: Is Parkinson’s Deadly
Mechanism Of Injury / Pathological Process
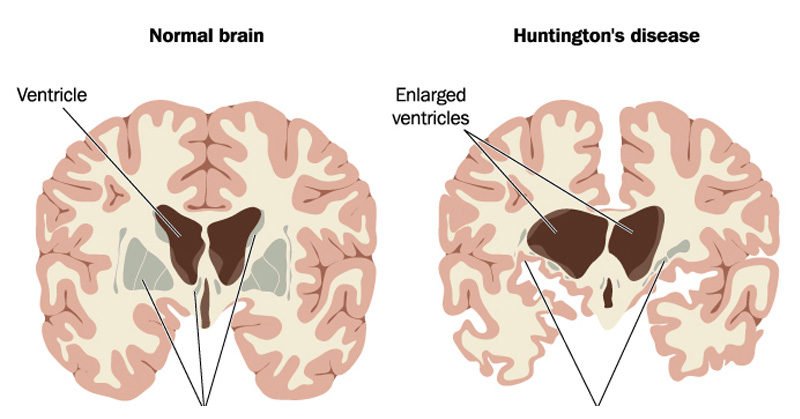
The most obvious neuropathology in HD occurs within the neostriatum , comprising gross atrophy of the caudate nucleus and putamen, accompanied by selective neuronal loss and astrogliosis . Marked neuronal loss also is seen in deep layers of the cerebral cortex. Other regions, including the globus pallidus, thalamus, subthalamic nucleus, substantia nigra, and cerebellum, show varying degrees of atrophy depending on the stage of the disease.
Human Fetal Tissue As A Source Of Progenitor Cells
The first study demonstrating that dopaminergic neurons could be replaced using fetal tissue was performed using 6-hydroxydopamine -lesioned rats that were implanted with DA-rich ventral mesencephalic tissue from rat fetuses . These studies were followed by the generation of the first non-human primates PD model: monkeys lesioned with 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine . This model manifested several of the patients symptoms, and transplanting primate fetal mesencephalic tissue into their striatum showed to alleviate these symptoms . These studies set foot for the first PD cell replacement therapy in humans. These clinical trials were performed using dopaminergic neuron precursors from human fetal tissue, which were transplanted into the striatum of PD patients . Transplanted tissue presented no negative effects at the transplantation site, was functional and survived in the transplanted brain region, but clinical benefits were variable .
Table 3. Common animal models of Parkinsons Disease.
Table 4. Common animal models of Huntingtons disease.
You May Like: What Is The Life Expectancy Of Someone With Parkinson’s Disease
What Is The Life Expectancy For People With Huntingtons Disease
The life expectancy of a person that has Huntington disease will depend on when do the symptoms start. Doctors estimate that it takes approximately 15 to 20 years for the persons death when they develop symptoms. It is important to note that the estimation does not take into account that the patient commits suicide before they suffer from a fatal condition.
Studies have also shown that patients that inherit the disease from their father have an earlier onset of symptoms. This would mean that those who got the gene from their fathers will probably have a lower life expectancy.
Professionals define another form of juvenile Huntingtons disease, which happens to people younger than 20 years old. This particular form has a shorter disease duration since the symptoms appear as early as eight years old or less. It also has a different progression of symptoms comparing it to the regular disease. Rigidity is the main symptom, instead of chorea, and seizures are another common thing for these patients. Besides, there is cognitive decline and dementia, sadly, at this very early age, showing the worse of the disease progression.
What Is The Difference Between Huntington’s Disease And Huntington’s Chorea
Chorea, which is sometimes a symptom of Huntingtons disease, but not deadly, is one of several known involuntary movements, which also include more common ones such as tremor and tics. To the untrained eye, it can be challenging to identify chorea, because its appearance varies from one individual to another.
Also Check: What Color Represents Cancer
What Is The Outlook For Patients Who Have Chorea
The outlook depends on whats causing the involuntary muscle movements. People with Huntingtons disease can live 15 to 25 years after they develop symptoms. The condition slowly gets worse over time and makes it very difficult to do everyday activities like dressing, bathing and eating.
Children who develop Sydenham chorea after rheumatic fever usually recover within 2 years. Some children may have lingering behavioral or emotional issues, such as obsessive compulsive disorder . These issues can last a lifetime.
Chorea itself usually can be managed with currently available treatments.
What Causes Huntingtons Disease
Huntingtons disease is caused by a mutation in the HTT gene. The HTT gene is responsible for making the huntingtin protein, which is thought to play an important role in nerve cells of the brain.
In Huntingtons disease, a DNA segment within this gene, called the CAG trinucleotide repeat, is repeated more often than is normal.
Also Check: What Color Represents Parkinson’s Disease
What Are The Risk Factors For Huntington Disease
If you have the Huntington disease gene, you will develop the disease at some point during your life. The age of onset of Huntington disease varies greatly from person to person, but most people develop it in their 30s or 40s.
Huntington disease is a rare disorder. More than 15,000 Americans currently have the disease, but many more are at risk of developing it.
Huntingtons Disease | Generations of Care and Search for a Cure
Finding Suggests That Treatment For One Disease Could Work For The Other Two
- Date:
- Loyola University Health System
- Summary:
- A study has found that abnormal proteins found in Alzheimer’s, Parkinson’s and Huntington’s diseases share a similar ability to cause damage when they invade brain cells. The finding suggests that an effective treatment for one neurodegenerative disease might work for other neurodegenerative diseases as well.
A Loyola University Chicago study has found that abnormal proteins found in Alzheimer’s disease, Parkinson’s disease, and Huntington’s disease all share a similar ability to cause damage when they invade brain cells.
The finding potentially could explain the mechanism by which Alzheimer’s, Parkinson’s, Huntington’s, and other neurodegenerative diseases spread within the brain and disrupt normal brain functions.
The finding also suggests that an effective treatment for one neurodegenerative disease might work for other neurodegenerative diseases as well.
The study by senior author Edward Campbell, PhD, first author William Flavin, PhD, and colleagues is published in the journal Acta Neuropathologica.
“A possible therapy would involve boosting a brain cell’s ability to degrade a clump of proteins and damaged vesicles,” Campbell said. “If we could do this in one disease, it’s a good bet the therapy would be effective in the other two diseases.”
Campbell stressed the study’s findings need to be followed up and confirmed in future studies.
Story Source:
Also Check: What Is The Life Expectancy Of Someone With Parkinson’s Disease
How Is Huntington Disease Diagnosed
Because many of these symptoms can be caused by other diseases, a detailed physical and neurological exam is usually needed. Not surprisingly, a family history of the disorder is often the biggest clue that you may have Huntington disease.
Special blood tests can help your healthcare provider determine your likelihood of developing Huntington disease. A computed tomography scan of the head can evaluate the scope and scale of brain cell damage and loss of brain tissue. A magnetic resonance imaging scan or a positron emission tomography scan may also be used.
Are You Having Symptoms Of It
This tool is a Huntington disease symptoms checker. It gathers the most important signs, symptoms, and risk factors for this condition. Therefore, it will aid anybody who uses it to determine the likelihood of having Huntington disease or developing it in the future. Besides, this tool is free and would only take you a few minutes to use it.
- 2shares
Recommended Reading: Cardinal Signs Of Parkinson’s
Pluripotent Stem Cells As A Source Of Differentiated Cell
Pluripotent stem cells are an unlimited source of cells with the potential to give rise to any type of cell of the body. Cells differentiated from embryonic stem cells and induced pluripotent stem cells are widely used as in vitro models for many diseases, including neurodegenerative diseases, and also as a source of cell-replacement therapies. Initial studies demonstrated that, when midbrain-derived dopaminergic neurons where grafted in the striatum of rodent models of PD , long-term survival of these cells was observed, which were tyrosine hydroxylase -positive neurons, completely reversed amphetamine-induced rotational behavior and lacked neuronal overgrowth . Importantly, midbrain human dopaminergic neurons grafted in MPTP-lesioned non-human primates survived in the grafted area, expressed TH, extended fibers to the surrounding striatum, and did not present neuronal overgrowth .
As highlighted previously, since HD is caused by a genetic mutation, and differentiated MSNs progenitors come from HD patients, it is imperative to correct the mutation present in these cells, along with the replacement of the target neurons and other cell types, like interneurons and glial cells, as they may provide a healthy and functional environment for the new neurons to integrate to the local circuitry and survive. Currently, no clinical trials are assessing the use of PSCs in HD patients.
Cerebral Dopamine Neurotrophic Factor And Mesencephalic Astrocyte
In 2003, a protein called mesencephalic astrocyte-derived neurotrophic factor was characterized and demonstrated to promote survival of embryonic dopaminergic neurons in vitro . Then, a homologous protein called CDNF was discovered with a protective role for dopaminergic neurons. Several studies evidence the protective role of CDNF and MANF in dopaminergic neurons against the injury caused by -syn oligomers . The intrastriatal injection of CDNF prevents the loss of TH-positive neurons in a 6-OHDA-lesioned rat model of PD , and protected dopaminergic neurons in 6-OHDA and MPTP mouse models of PD . MANF has been tested in the 6-OHDA-lesioned rat model showing beneficial effects . CDNF and MANF diffuse to the brain significantly better than GDNF, and CDNF was more efficient in reducing amphetamine-induced ipsilateral rotations in the 6-OHDA rat PD model in comparison with GDNF treatment . In 6-OHDA-lesioned monkeys, PET imaging showed a significant increase of DA transporter ligand-binding activity in lesioned animals treated with CDNF .
The first phase III clinical trial using CDNF in PD patients is being conducted since 2017. In this study, an implanted drug delivery system for Ipu of recombinant human CDNF is used in patients with idiopathic mild-advanced PD . Additionally, another phase III clinical trial to evaluate the beneficial effects of CDNF in PD patients is still on course . Currently, the delivery of CDNF for HD treatment has not been described.
Also Check: Is Parkinson’s Disease Fatal
Diagnosis Of Huntington Disease
-
A doctor’s evaluation, confirmed by genetic testing
-
Computed tomography or magnetic resonance imaging
Huntington disease may be difficult to recognize in the early stages because symptoms are subtle. The disease may be suspected based on symptoms and a family history. Doctors should be told about relatives who have had mental problems or have been diagnosed as having a neurologic disorder or a psychiatric disorder because they may have had Huntington disease that was not diagnosed.
Computed tomography or magnetic resonance imaging is done to check for the degeneration of the basal ganglia and other areas of the brain usually affected by the disease and to rule out other disorders.
Genetic testing is done to confirm the diagnosis. Genetic testing and counseling are important for people who have a family history of the disease but no symptoms because people are likely to have children before symptoms appear. For such people, genetic counseling should precede genetic testing. They are referred to centers that have expertise in dealing with the complex ethical and psychologic issues involved.
Sleep Pattern Disorders In Hd
A typical sleep pattern in adults includes non-rapid eye movement sleep divided into three stages : the sleep gradually deepens from N1 to N3, followed by rapid eye movement sleep , during which suppression of postural muscle tone is normally observed. NREM lasts about 6090 min, REM lasts about 1015 min, and the whole sleep cycle consisting of NREM and REM is repeated four or five times during a nights sleep.
Reports presenting research concerning sleep disorders during the REM stage in HD patients are ambiguous. Some authors report a lack, shortening, or delay of the REM stage , but no REM sleep disorders were detected in other studies on HD patients .
HD patients also demonstrate behavioral disorders related to the REM sleep stage . Skeletal muscle atonia is one of the characteristic features of REM sleep, and its absence can lead to sudden body movements, e.g., hitting, kicking, tossing, and turning during sleep these phenomena are accompanied by realistic dreams, often provoking a sense of danger .
Some authors suggest that in HD a mutant form of huntingtin may accumulate in areas that control muscle atonia during REM sleep, thus leading to their failure. These areas include the dorsolateral pons, the locus coeruleus, the reticular formation of the medulla, the pedunculopontine tegmental nucleus, and the hypothalamus. Cell loss in the locus coeruleus and in the hypothalamus in HD has been confirmed in studies.
Read Also: Freddie Roach Medical Condition

