What Are The Symptoms Of End
Stage four for Parkinsons disease is often called advanced Parkinsons disease because people in this stage experience severe and incapacitating symptoms. This is when medication doesnt help as much and serious disabilities set in.
Theres an increased severity in:
- How you speak a softer voice that trails off.
- Falling and trouble with balance and coordination.
- Freezing a sudden, but temporary inability to move, when you start to walk or change direction.
- Moving without assistance or a wheelchair.
- Other symptoms such as constipation, depression, loss of smell, low blood pressure when going to stand up, pain, and sleep issues.
Many times someone with advanced PD cant live on their own and needs help with daily tasks.
Stage five is the final stage of Parkinsons, and assistance will be needed in all areas of daily life as motor skills are seriously impaired. You may:
- Experience stiffness in your legs. It may make it impossible to walk or stand without help.
- Need a wheelchair at all times or are bedridden.
- Need round-the-clock nursing care for all activities.
- Experience hallucinations and delusions.
As Parkinsons disease progresses into these advanced stages, its symptoms can often become increasingly difficult to manage. Whether you or your loved one with end-stage Parkinsons lives at home, in an assisted living facility or a nursing home, hospice services can optimize your quality of life and that of your family members as well.
Biomarkers Influence On Parkinson’s Disease Progression Model
At the end of the study, the influence of biomarkers on Parkinson’s disease progression model was analyzed. First, we performed spearman correlation analysis between biomarkers and disease progression and found that the CSF amyloid and CSF α-synuclein were significantly associated with disease progression, of which the correlation coefficient were, respectively, â0.132, â0.160. The correlation analysis results of other variables are shown in Supplementary Table 1. After incorporating the two variables into feature combinations selected by feature selection based on clinical characters and scales scores and eliminating the missing data, a total of 441 cases were left. The models were reconstructed based on the feature combinations before and after the inclusion of biomarkers variables and the performance of two sets of models were compared by t-test. The P-value were 0.408 and 0.883 respectively, showing no significant difference and indicating that these biomarkers had no significant impact on the progression model within the data in the study. The R2 and RMSE of different regression models are shown in Supplementary Table 3.
What Can Be Done
The first step is to get a referral to a speechlanguage pathologist . This professional will take a medical history and interview you about eating and swallowing. Next you will probably have a swallowing evaluation, using either a video x-ray or an endoscopic exam. During this procedure, you will swallow different consistencies of food and liquids, and the SLP can observe the entire swallowing process: from your first sip and bite, through the mouth, down the throat and esophagus, and into the stomach. This is the best way to find out the extent and cause of swallowing problems. Then the SLP can recommend treatment.
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Is Parkinsons Disease Fatal
Parkinsons disease itself doesnt cause death. However, symptoms related to Parkinsons can be fatal. For example, injuries that occur because of a fall or problems associated with dementia can be fatal.
Some people with Parkinsons experience difficulty swallowing. This can lead to aspiration pneumonia. This condition is caused when foods, or other foreign objects, are inhaled into the lungs.
Rate Of Progression In Activity And Participation Outcomes In Exercisers With Parkinsons Disease: A Five
Stephanie A. Miller
1University of Indianapolis, Krannert School of Physical Therapy, 1400 E. Hanna Ave., Indianapolis, IN 46227, USA
2University of Indianapolis, Interprofessional Health and Aging Studies, 1400 E. Hanna Ave., Indianapolis, IN 46227, USA
3University of Indianapolis, Exercise Science, Department of Kinesiology, Health and Sport Sciences, 1400 E. Hanna Ave., Indianapolis, IN 46227, USA
Academic Editor:
Abstract
1. Introduction
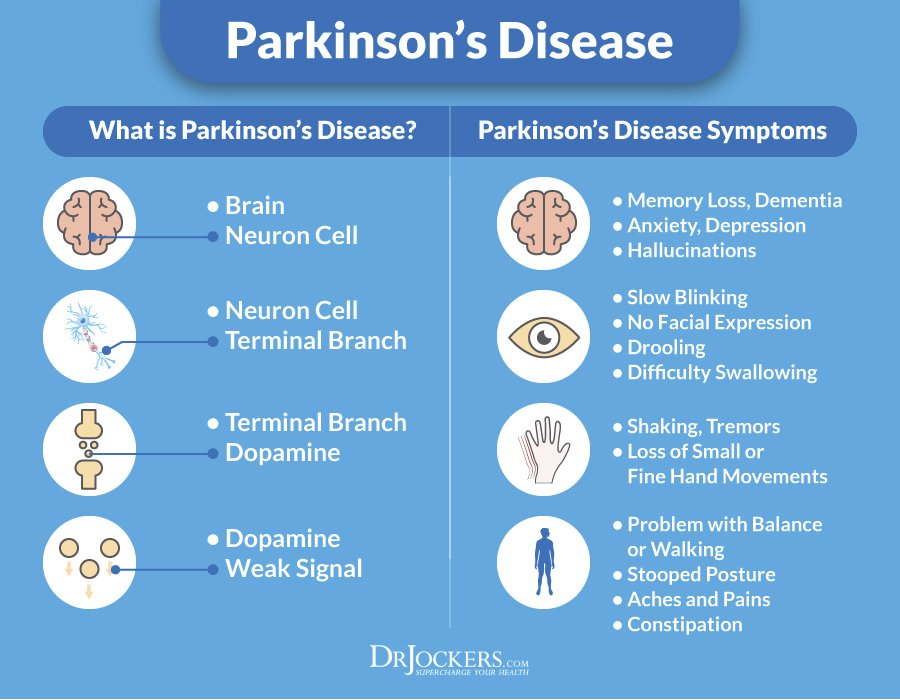
Parkinsons disease is the second most common degenerative neurologic disorder worldwide . It is characterized by progressive decline in motor and nonmotor symptoms leading to increased disability and reduced quality of life. Despite a gradual loss of function with time, variations in the clinical progression of PD exist .
2. Methods
2.1. Participants
For the purpose of this analysis, only participants who self-reported taking part in exercise on a regular basis over the course of the study were included in the analysis. Exercise was defined as any physical activity performed outside of normal daily activities. The Stages for Readiness to Exercise Scale was used to delineate regular participation in exercise. Regular exercisers scored a 4 or 5 on the stages for readiness to exercise scale . Self-reported stages of change in exercise behavior have strong construct validity and test-retest reliability in both healthy and disabled populations .
2.2. Procedures
2.3. Outcome Measures
2.4. Data Analysis
3. Results
Also Check: What Is The Life Expectancy Of Someone With Parkinson’s Disease
When To Seek Hospice Care
When you or your loved one have a life expectancy of six months or less, you become eligible for hospice care a type of comfort care provided at the end of life for someone living with end-stage Parkinsons disease. Hospice provides extra support so your loved one can live as comfortably as possible.
If you have experienced a significant decline in your ability to move, speak, or participate in activities of daily living without caregiver assistance, its time to speak with a hospice professional.
Read more: What is hospice care?
Some of the things that determine whether your loved one with end-stage Parkinsons is eligible for hospice include: difficulty breathing, bed bound, unintelligible speech, inability to eat or drink sufficiently, and/or complications including pneumonia or sepsis.
If you live in South Jersey, our nurse care coordinator can answer your questions and decide if your loved one is ready for hospice care. Call us 24/7 at 229-8183.
Living Well With Parkinson’s
While medication and DBS surgery are the most effective treatments for PD, individuals often choose to delay these treatments because of their adverse side effects. Until a therapy is developed that can halt the progression of PD, there is a significant need for strategies that provide symptom relief without causing negative side effects.
Diet, Exercise, and Stress Reduction
Findings from several studies suggest that exercise has the potential to provide relief from certain PD symptoms. Anecdotally, people with Parkinsons disease who exercise typically do better. However, many questions remain. Among them is whether exercise provides a conditioning effect by strengthening muscles and improving flexibility or whether it has a direct effect on the brain.
In an NINDS-funded trial comparing the benefits of tai chi, resistance training, and stretching, tai chi was found to reduce balance impairments in people with mild-to-moderate PD. People in the tai chi group also experienced significantly fewer falls and greater improvements in their functional capacity.
Technologies that Improve Quality of Life
Read Also: What Happens When You Stop Taking Carbidopa/levodopa
How Can Hospice Help Your Loved One In The Final Stages Of Parkinsons Disease
Hospice care is an extra layer of support to help you care for your loved one with end-stage Parkinsons disease. It is a special kind of care that provides comfort, support, and dignity at the end of life.
The comprehensive program focuses on physical, emotional, and spiritual quality of life through the help of a team of experts. The team includes a board-certified physician, nurse, social worker, certified home health aide , spiritual support counselor, and volunteer.
The nurse will explain the prognosis and what to expect in the upcoming days or weeks. They will also monitor pain and other symptoms. The CHHA helps with personal care needs like bathing and changing bed linens. The social worker helps address social, emotional and practical challenges including complex and inter-related needs. The spiritual support counselor helps explore spiritual concerns.
Most importantly, the hospice team will be there for you during this difficult time, bringing you peace of mind. The team is on call 24 hours a day even at 2:00 am.
Hospice is about making your final months and weeks as good as possible. This means focusing on what really matters to you.
Parkinson’s Disease Symptoms: Life Expectancy
Even though Parkinson’s disease is a serious, progressive condition, it is not considered a fatal illness. People who have Parkinson’s disease usually have the same average life expectancy as people without the disease.
But when the disease is in its advanced stages, Parkinson’s symptoms can lead to life-threatening complications, including:
- Falls that lead to fractured bones
- Pneumonia
- Choking
Thinking about the progression of Parkinson’s disease can be frightening. But proper treatments can help you live a full, productive life for years to come. And researchers hope to one day find ways to halt the progression of Parkinson’s and restore lost functioning.
Don’t Miss: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Stage One Of Parkinsons Disease
In stage one, the earliest stage, the symptoms of PD are mild and only seen on one side of the body , and there is usually minimal or no functional impairment.
The symptoms of PD at stage one may be so mild that the person doesnt seek medical attention or the physician is unable to make a diagnosis. Symptoms at stage one may include tremor, such as intermittent tremor of one hand, rigidity, or one hand or leg may feel more clumsy than another, or one side of the face may be affected, impacting the expression.
This stage is very difficult to diagnose and a physician may wait to see if the symptoms get worse over time before making a formal diagnosis.
We Compiled The Most Popular Parkinsons Questions And Answers In One Place
As your Parkinsons disease journey evolves, so do your questions about symptoms, treatment options, research and medications. Whether you live with Parkinsons or care for someone who does, you are not alone in looking for answers to your big PD questions.
The Parkinsons Foundation has recently released Frequently Asked Questions: A Guide to Parkinsons Disease, a new and improved booklet that provides answers to the most frequently asked questions our Helpline receives. Pro tip: every section in the booklet provides additional free resources you can check out to learn more. Order the free book now, read it online or check out some questions and answers below:
Q: Can Parkinsons be cured?
A: Not yet. However, many PD symptoms can be treated and researchers are making advances in understanding the disease, its causes and how to best treat it.
Q: What are the stages of Parkinsons?
A: The stages of Parkinsons correspond to the severity of movement symptoms and to how much the disease affects a persons daily activities. At all stages of Parkinsons, effective therapies are available to ease symptoms and make it possible for people with PD to live well.
Q: How can I find a doctor who can treat Parkinsons?
Q: Is it okay to drink alcohol?
A: Consult your doctor first. Generally, moderate consumption should be acceptable for people with PD, if there are no medical conditions or medications that prohibit alcohol use.
Q: Are there any new Parkinsons drugs on the horizon?
Recommended Reading: Parkinson’s Disease Alpha Synuclein
Unified Parkinsons Disease Rating Scale
The UPDRS contains four parts. The first part assesses intellectual function, mood, and behavior. The second one assesses activities of daily living. The third part assesses one motor function, and the fourth assesses motor complications.
Each part includes scores that altogether rate the severity of the disease. The maximum score is 199, reflecting total disability, whereas a score of zero means no disability.
Stage Three Of Parkinsons Disease
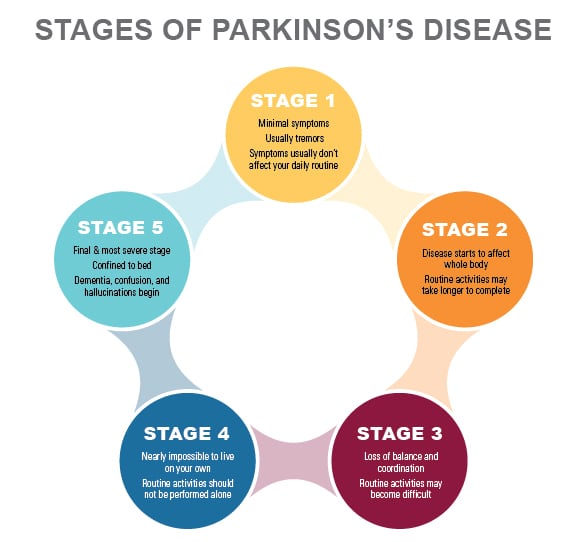
Stage three is considered mid-stage and is characterized by loss of balance and slowness of movement.
Balance is compromised by the inability to make the rapid, automatic and involuntary adjustments necessary to prevent falling, and falls are common at this stage. All other symptoms of PD are also present at this stage, and generally diagnosis is not in doubt at stage three.
Often a physician will diagnose impairments in reflexes at this stage by standing behind the patient and gently pulling the shoulders to determine if the patient has trouble maintaining balance and falls backward . An important clarifying factor of stage three is that the patient is still fully independent in their daily living activities, such as dressing, hygiene, and eating.
Don’t Miss: What Are Early Warning Signs Of Parkinson’s Disease
Predicting Progression In Parkinsons Disease Using Baseline And 1
Article type: Research Article
Authors: Chahine, Lana M.a * | Siderowf, Andrewb | Barnes, Janelc | Seedorff, Nicholasc | Caspell-Garcia, Chelseac | Simuni, Tanyad | Coffey, Christopher S.c | Galasko, Douglase | Mollenhauer, Britf | Arnedo, Vanessag | Daegele, Nicholeh | Frasier, Markg | Tanner, Carolinei | Kieburtz, Karlj | h | The Parkinsons Progression Markers Initiative
Affiliations: Department of Neurology, University of Pittsburgh, Pittsburgh, PA, USA | Departments of Neurology Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA | Department of Biostatistics, College of Public Health, University of Iowa, Iowa City, IA, USA | Department of Neurology, Northwestern University Feinberg School of Medicine, Chicago, IL, USA | Department of Neurology, University of California, San Diego, CA, USA | Department of Neurology, University Medical Center Goettingen, Goettingen, Germany and Paracelsus-Elena-Klinik, Kassel, Germany | The Michael J. Fox Foundation, New York, NY, USA | Institute for Neurodegenerative Disorders, New Haven, CT, USA | Department of Neurology, University of California San Francisco, San Francisco, CA, USA | Department of Neurology, University of Rochester Medical Center, Rochester, NY, USA
Correspondence: Correspondence to: Lana M. Chahine, Department of Neurology, University of Pittsburgh, 3471 Fifth Avenue, Pittsburgh, PA 15213, USA. Tel.: +1 412 692 4916 E-mail: .
DOI: 10.3233/JPD-181518
Abstract
Changes In Genetic Expression Revealed
The latest publication from this study reports the findings from whole-genome microRNA sequencing of the cerebrospinal fluid of the 75 participants before and after the first 12 months of treatment with nilotinib or the placebo.
Over the 12-month period, the scientists observed significant alterations in microRNAs that control genes and pathways that regulate the production of the blood-brain barrier, the removal of damaged cells, and the formation of new blood vessels.
The study authors argue that this reveals a mechanism that underlies the progression of Parkinsons disease.
Specifically, they discovered that the 300-mg dose of nilotinib reversed these effects by inactivating a protein called DDR1 that affects the ability of the blood-brain barrier to function correctly. On the inhibition of DDR1 by nilotinib, the normal transportation of molecules in and out of the brain filter resumed, and inflammation declined to the point that dopamine was being produced again.
Not only does nilotinib flip on the brains garbage disposal system to eliminate bad toxic proteins, but it appears to also repair the blood-brain barrier to allow this toxic waste to leave the brain and to allow nutrients in, Dr. Moussa explained.
Parkinsons disease is generally believed to involve mitochondrial or energy deficits that can be caused by environmental toxins or by toxic protein accumulation it has never been identified as a vascular disease.
Dr. Charbel Moussa, Ph.D.
Also Check: Parkinson’s And Dementia Life Expectancy
Extended Data Fig 3 Associations Between A Second Rims2 Variant Rs116918991 Tmem108 Rs138073281 And Wwox Rs8050111 With Cognitive Pd Progression
a,c,e, Covariate-adjusted survival curves for PD patients without the indicated variant and for those carrying the indicated variant are shown. P values Cox PH models with two-sided Wald test. b,d,f, Adjusted mean MMSE scores across time predicted from the estimated fixed-effect parameters of the LMM analysis are shown for cases carrying the variant and cases without the variant adjusting for covariates. Shaded ribbons indicate ± s.e.m. around predicted MMSE scores across time. Note that a second RIMS2 variant rs116918991 is shown in a and b, and that the HR and P values shown here for TMEM108 rs138073281 and WWOX rs8050111 are different from the HR and P values from the main analysis , where variant alleles were coded as 0, 1, 2. P values from LMM analysis with two-sided t-test.
Discovery Comes From Phase Ii Trial
The new discovery comes from the second part of a Phase II clinical trial that featured next generation whole genome sequencing of the cerebrospinal fluid of 75 Parkinsons patients, before and after treatment with a repurposed leukemia drug, nilotinib, or placebo.
This study lasted 27 months the initial trial was double-blinded and patients were randomized to either placebo, or 150mgs or 300mgs nilotinib for 12 months. The patients had severe Parkinsons disease all treated with optimal standard of care and many had also used the most sophisticated treatments possible, such as deep brain stimulation.
The second part of the study employed an adaptive design, and all participants had a 3-month drug washout period before re-randomization to either 150mgs or 300mgs for an additional 12 months. After 27 months, nilotinib was found to be safe, and patients who received nilotinib showed a dose-dependent increase of dopamine, the chemical lost as a result of neuronal destruction.
It appeared nilotinib halted motor and non-motor decline in the patients taking the 300mgs higher dose, says Moussa. The clinical outcomes of this study was published in Movement Disorders in March 2021.
The current part of the study just published, examined the cerebrospinal fluid of patients via epigenomics, which is a systematic analysis of the global state of gene expression, in correlation with continuing clinical outcomes. The new analysis helps explain the clinical findings.
Read Also: Can Parkinson’s Run In The Family
