Conditions That Mimic Parkinsons Disease
Parkinson disease is a complex progressive neurological disease involving the loss of neurons in a part of the brain called the substantia nigra. This results in a reduction in the amount of dopamine, a chemical messenger or neurotransmitter. When this important chemical in the brain is depleted, the symptoms of Parkinsons disease develop.
Parkinson disease is a complex progressive neurological disease involving the loss of neurons in a part of the brain called the substantia nigra. This results in a reduction in the amount of dopamine, a chemical messenger or neurotransmitter. When this important chemical in the brain is depleted, the symptoms of Parkinsons disease develop.
Many people across the UK are living with Parkinsons Disease, but some only share a few of the symptoms and are actually experiencing another type of movement disorder. There are a number of complex conditions that mimic Parkinsons Disease, making it even more difficult to diagnose and treat successfully. At Dementech, our specialists and state-of-the-art equipment make us well placed to provide the most accurate diagnosis and tailored treatment plan for you.
Conditions Misdiagnosed As Parkinson’s Disease
Charles Cullen
Parkinsons disease, especially in its early stages when symptoms are mild, is not an easy disease to diagnose. The non-specific, and easily overlooked nature of the signs of Parkinsons make it difficult to spot, and unlike many illnesses, there is no one laboratory test or radiological exam that will provide a definitive diagnosis of Parkinsons disease.
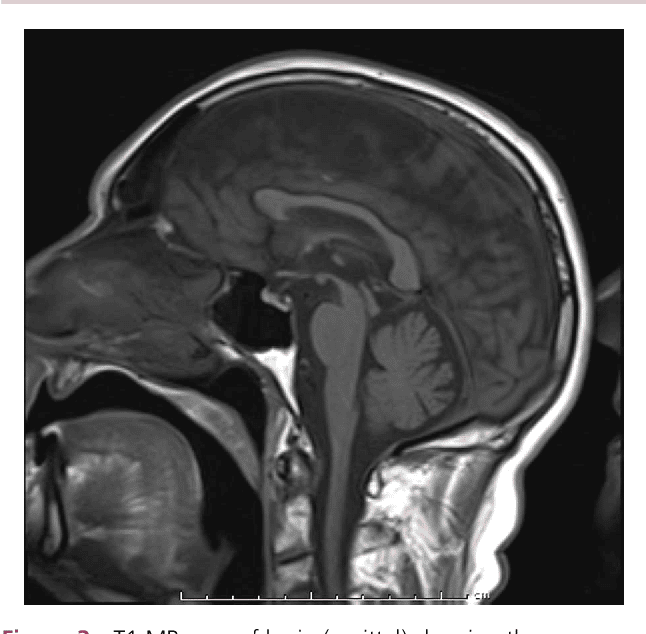
Patients exhibiting Parkinsons-like symptoms may undergo blood and urine tests, or CT or MRI scans to exclude other conditions, but none of these will provide a diagnosis of Parkinsons disease.
The best way to test for Parkinsons disease is to conduct a systemic neurological examination that includes tests to gauge a patients reflexes, muscle strength, coordination, balance, gait, and overall movement. Even so, according to information presented on The Michael J. Fox Foundation for Parkinsons Research, up to 25 percent of Parkinsons disease diagnoses are incorrect.
So, why is there confusion about diagnosing Parkinsons disease? The simple answer is that symptoms of Parkinsons disease are not clear cut, and therefore, it is easy to mistake them for other conditions, or to classify them as parkinsonian when they are not.
Here is a brief overview of the top ten conditions mistaken for Parkinsons disease:
Beyond those top three, there are other conditions that are often confused with Parkinsons disease, including:
Hallervorden Spatz Disease: a degenerative movement disorder that is genetic
Plus a couple more-
What Are The Complications Of Parkinson Disease
Parkinson disease causes physical symptoms at first. Problems with cognitive function, including forgetfulness and trouble with concentration, may arise later. As the disease gets worse with time, many people develop dementia. This can cause profound memory loss and makes it hard to maintain relationships.
Parkinson disease dementia can cause problems with:
- Speaking and communicating with others
- Problem solving
- Paying attention
If you have Parkinson disease and dementia, in time, you likely wont be able to live by yourself. Dementia affects your ability to care of yourself, even if you can still physically do daily tasks.
Experts dont understand how or why dementia often occurs with Parkinson disease. Its clear, though, that dementia and problems with cognitive function are linked to changes in the brain that cause problems with movement. As with Parkinson disease, dementia occurs when nerve cells degenerate, leading to chemical changes in the brain. Parkinson disease dementia may be treated with medicines also used to treat Alzheimers disease, another type of dementia.
Recommended Reading: Is There A Test To See If You Have Parkinson’s
What Is Parkinson Disease
Parkinson disease is a movement disorder. It can cause the muscles to tighten and become rigid This makes it hard to walk and do other daily activities. People with Parkinsons disease also have tremors and may develop cognitive problems, including memory loss and dementia.
Parkinson disease is most common in people who are older than 50. The average age at which it occurs is 60. But some younger people may also get Parkinson disease. When it affects someone younger than age 50, its called early-onset Parkinson disease. You may be more likely to get early-onset Parkinson disease if someone in your family has it. The older you are, the greater your risk of developing Parkinson disease. Its also much more common in men than in women.
Parkinson disease is a chronic and progressive disease. It doesnt go away and continues to get worse over time.
You May Like: Beginning Signs Of Parkinsons
What Diseases Can Be Mistaken For Parkinsons
This is the list of different diseases that may be mistaken with Parkinsons disease:
- Progressive supranuclear palsy.
Alzheimers disease and primary lateral sclerosis can also be mistaken for Parkinsons disease. Other similar conditions include essential tremor, dystonic tremor, vascular Parkinsonism, and drug-induced Parkinsonism.
Also Know, what are the four cardinal signs of Parkinsons disease? Cardinal symptoms. Four symptoms are considered cardinal in PD: bradykinesia, tremor, rigidity, and postural instability also referred to as parkinsonism. Tremor is the most apparent and well-known symptom.
Similarly, it is asked, what is similar to Parkinsons?
Progressive Supranuclear Palsy: An Atypical Parkinsonian Syndrome. Progressive supranuclear palsy is not Parkinsons disease , but is a Parkinsonian-like syndrome. PSP is a rare brain disorder that causes serious and progressive problems with gait and balance, as well as eye movement and thinking problems.
Does stress cause Parkinsons disease?
Research suggests that stressful life events may increase the risk of Parkinsons disease. In addition, animal studies indicate that stress damages dopamine cells, resulting in more severe parkinsonian symptoms. In humans, acute stress can worsen motor symptoms, including bradykinesia, freezing, and tremor.
Recommended Reading: Rigidity In Parkinsons Disease
Recommended Reading: Is Parkinson’s Disease A Form Of Dementia
How Are They Alike
MS and Parkinsonâs both affect your central nervous system, which includes your brain and spinal cord. Thatâs why they both can affect how you move, sleep, feel, and talk.
These diseases both affect your nerves. MS can break down the coating, called myelin, that surrounds and protects your nerves. In Parkinsonâs, nerve cells in a part of your brain slowly die off.
Both can start out with mild symptoms, but they get worse over time.
Common symptoms of both diseases include:
- Shaky fingers, hands, lips, or limbs
- Slurred speech thatâs hard for others to understand
- Numb or weak limbs that make your walk unsteady
- Loss of muscle control that often affects one side of your body at first, then later both
- Spastic limb movements that are hard to control
- Loss of bladder or bowel control
Depression is another symptom common to both conditions.
Characteristics Of Atypical Msa: Parkinsons Disease Mimics
Case illustration
A 67-year-old female : presented with a 1-year history of worsening dexterity of her left hand. Examination revealed an asymmetrical tremor of the hand at rest with cogwheel rigidity and bradykinesia. Her symptoms and signs improved with levodopa therapy . Over the next 3 years, she developed motor fluctuations, generalized peak-dose dyskinesia, worsening dysarthria, urinary frequency and constipation. She also reported intermittent mild non-threatening visual hallucinations. Orofacial dystonia and urinary incontinence then became more intrusive. She died aged 75. The final clinical diagnosis was Parkinsons disease. Autopsy confirmed the pathological diagnosis of MSA . There were frequent depositions of neuritic plaques but no neurofibrillary tangles were found in the brain. Key clinical features of all Parkinsons disease mimics are provided in Supplementary Table 2.
Atypical MSA versus typical MSA or Parkinsons disease
Red flag features in atypical MSA versus typical MSA or Parkinsons disease
| Pathological diagnosis . |
|---|
Don’t Miss: What Are The Last Stages Of Parkinson’s
Common Misdiagnosis: Multiple Sclerosis
One of the most common answers to the question was multiple sclerosis . Both diagnoses have an effect on the central nervous system. These diagnoses also frequently cause muscle spasms, balance changes, tremor, and impaired memory. However, these are two separate diagnoses.
One difference is that MS is often diagnosed when someone is in their 20s, while most people receive a PD diagnosis in their 60s. Also, MS is an autoimmune disease that over time causes nerve damage. Parkinsons affects the brain. The brain starts producing less and less dopamine, which is responsible for controlling movement.
Yes, with MS which I was worried about for years, but right now I do not know which one is worse. However, my meds are helping a lot. My new saying is It is what it is, aka just live on. My neurologist says that I have stage one mild Parkinson’s disease.
My husband was diagnosed with MS back in 1993 when he had a mini stroke. He was diagnosed with Parkinsons in 2014.
Common Symptoms Of Parkinsons Disease
There are two types of symptoms: motor and non-motor .
Common motor symptoms include:
In most cases, both types of symptoms will worsen over time as the disease progresses. For conditions that mimic Parkinsons, gradual worsening of the symptoms can vary and will also depend largely on the individual. Dementech can provide support with specialist medical interventions at any stage of symptom development.
Challenging Cases: Symptoms & Conditions That Mimic Parkinsons Disease
There are a number of conditions that present some of the signs and symptoms of Parkinsons, but that do not respond in the same way to typical treatments. These diseases are referred to as Atypical Parkinsonisms, and are most likely to affect people in their 50s and 60s, although this can vary.
Many other conditions involving movement -based issues mimic Parkinsons Disease. A patient therefore may show no signs of developing PD but will experience very similar symptoms. These conditions can be particularly challenging for non-specialists and can sometimes lead to misdiagnosis. Specialist input from the team at Dementech is recommended in such cases.
Atypical Parkinsonisms include disorders such as:
Read Also: Is There Any Medication For Parkinson’s Disease
Whats The Difference Between Multiple System Atrophy And Parkinsons
Parkinsons and MSA both affect the movement control system and the involuntary autonomic control system and early symptoms can make a differential diagnosis a challenge. MSA, however, tends to progress faster than Parkinsons balance problems and a stooped posture happen earlier and get worse more quickly with MSA and autonomic functions such as blood pressure, heart rate, breathing, sweating, bladder function, and sexual problems are more severe in people with MSA.
For more information on multiple symptom atrophy, read this fact sheet.
Also Check: What Medications Are Used To Treat Parkinsons Disease
What Are Atypical Parkinsonian Disorders
Atypical Parkinsonian disorders are progressive diseases that present with some of the signs and symptoms of Parkinsons disease, but that generally do not respond well to drug treatment with levodopa. They are associated with abnormal protein buildup within brain cells.
The term refers to several conditions, each affecting particular parts of the brain and showing a characteristic course:
- Dementia with Lewy bodies, characterized by an abnormal accumulation of alpha-synuclein protein in brain cells
- Progressive supranuclear palsy, involving tau protein buildup affecting the frontal lobes, brainstem, cerebellum and substantia nigra
- Multiple system atrophy, another synucleinopathy that affects the autonomic nervous system , substantia nigra and at times the cerebellum
- Corticobasal syndrome, a rare tauopathy that typically affects one side of the body more than the other and makes it difficult for patients to see and navigate through space
Read Also: How Long Does End Stage Parkinson’s Last
Dbs As A Treatment For Movement Disorders
Movement disorders are neurological conditions that cause abnormal movements. Its estimated that 42 million people suffer from some form of movement disorder in the U.S. For proper diagnosis and treatment you want an expert team from multiple disciplines working together for you. At the University of Michigan Movement Disorders Program, we have the latest technologies, cutting-edge clinical trials and a committed team of specialists to provide you the best quality of life possible.
We treat the full spectrum of movement disorders, including:
- Tourettes syndrome and tics
With more than a dozen specialists in neurology, neurosurgery, neuroradiology and neuropsychology, together with our colleagues in speech pathology and physical medicine and rehabilitation, the Movement Disorders Program is one of the largest and most comprehensive in the country. We also have the greatest number of movement disorder specialists in the region devoted to the care of patients, the understanding of disease processes and the development of new therapies.
Is There A Cure For Parkinsons

Theres currently no cure for Parkinsons, a disease that is chronic and worsens over time. More than 50,000 new cases are reported in the United States each year. But there may be even more, since Parkinsons is often misdiagnosed.
Its reported that Parkinsons complications was the
Complications from Parkinsons can greatly reduce quality of life and prognosis. For example, individuals with Parkinsons can experience dangerous falls, as well as blood clots in the lungs and legs. These complications can be fatal.
Proper treatment improves your prognosis, and it increases life expectancy.
It may not be possible to slow the progression of Parkinsons, but you can work to overcome the obstacles and complications to have a better quality of life for as long as possible.
Parkinsons disease is not fatal. However, Parkinsons-related complications can shorten the lifespan of people diagnosed with the disease.
Having Parkinsons increases a persons risk for potentially life threatening complications, like experiencing:
Parkinsons often causes problems with daily activities. But very simple exercises and stretches may help you move around and walk more safely.
Don’t Miss: Does Parkinson’s Cause Dizziness
What Is Alzheimers Disease
Alzheimers disease , the most common form of dementia among older adults, is an irreversible degeneration of the brain that causes disruptions in memory, cognition, personality, and other functions that eventually lead to death from complete brain failure. Genetic and environmental factors including diet, activity, smoking, traumatic brain injury, diabetes, and other medical diseases contribute to the risk of developing this form of the disease. The hallmarks of Alzheimers disease are the accumulation of beta-amyloid plaques between nerve cells in the brain and neurofibrillary tangles, which are twisted fibers found inside the brains cells). These tangles consist primarily of a protein called tau.
You May Like: Using Cbd For Parkinsons Disease
Imaging Biomarkers In Parkinsonism
DaTscan: dopamine-active transporter scans showing binding of 123I-fluoropropyl to DaT protein in the nigrostriatal nerve endings of the striatum. Normal: symmetrical normal specific binding of FPCIT in striatum. Parkinson’s disease: reduced specific binding of FPCIT in the posterior striatum, particularly on the left .
Further imaging approaches are in development on a research basis. 7-T MR scanning can detect structural nigral abnormalities. Diffusion-tensor MRI and diffusion-weighted imaging have shown some promise in diagnosing PD and its mimics. Transcranial sonography can detect hyperechogenicity in the midbrain of patients with PD. Although this is not specific, it may be a marker of susceptibility to PD.,,
Read Also: Best Exercise Equipment For Parkinson’s
Whats The Outlook For People With Parkinsons Plus
Although there currently isnt a treatment to halt the progression of Parkinsons plus syndrome, there are treatments that can help you manage your symptoms and improve your quality of life.
The exact outlook for Parkinsons plus syndrome depends on the person and the specific condition they have. Someone who is otherwise healthy when theyre diagnosed will typically have a longer life expectancy than someone who is already facing other health conditions when theyre diagnosed. Your doctor will monitor your condition over time and can let you know how its progressing.
Vladimir Putin Seen Gripping Table With Veins Bulging As Illness Rumors Mount
Doctors seriously struggle to correctly diagnose Parkinsons disease, a new study shows.
Over a quarter of those with Parkinsons were initially misdiagnosed, according to a recent survey of over 2,000 people by charity Parkinsons UK. And in many cases, the misdiagnoses can have serious health consequences.
For 26 percent of respondents, doctors initially linked their symptoms with something else, the Guardian reports. Of those falsely diagnosed, 48 percent were given treatment for their nonexistent illness, 36 percent received medication for it, 6 percent underwent operations and another 6 percent were given both medication and operations.
As a result, of those who received treatment for the wrong diagnosis, 34 percent report their health worsened.
Women and people aged 51 to 60 were most likely to be misdiagnosed with Parkinsons, which currently affects more than 10 million people worldwide.
For those who were told their Parkinsons was another disease or all in their head the experience can be devastating.
I went to the doctors but no one could understand what was wrong with me, Katy Dickinson shares in the study.
When she began seeking medical help, her left foot had recently begun dragging, a tremor shed had for years had worsened, and her voice was beginning to be affected but doctors told her she was making her symptoms up.
In defense of doctors, Parkinsons UKs Katie Goates points out that the disease is notoriously difficult to diagnose.
Read Also: What Is The Best Mattress For Parkinson Patients
How Is A Diagnosis Made
Because other conditions and medications mimic the symptoms of PD, getting an accurate diagnosis from a physician is important. No single test can confirm a diagnosis of PD, because the symptoms vary from person to person. A thorough history and physical exam should be enough for a diagnosis to be made. Other conditions that have Parkinsons-like symptoms include Parkinsons plus, essential tremor, progressive supranuclear palsy, multi-system atrophy, dystonia, and normal pressure hydrocephalus.
Also Check: Possible Causes Of Parkinsons Disease
How Is Depression Diagnosed
Most people with PD will go undiagnosed or undertreated for depression therefore, being diagnosed is a critical first step towards effective treatment and recovery. To be diagnosed with depression, a person must experience one of the following symptoms most of the time over the previous two weeks:
- Loss of interest or pleasure in activities once enjoyed
In addition, some of the following symptoms must be present:
- Changes in sleep or appetite
- Increased fatigue
You May Like: What’s New In Parkinson’s Research
