What Organs Does Parkinson Disease Affect
Parkinsons disease is characteristical, a movement disorder responsive to dopaminergic medication. But it does not only affect the movement or body motor system. It changes as well the autonomic nervous system that controls the involuntary actions of the body.
These automatic actions of the body include some like a heart beating, sweating, swallowing, and bowel movements for digestion. The autonomic nervous system has two subdivisions, the sympathetic system, and the parasympathetic system.
The sympathetic system functions apply when the body enters in an alert state and the parasympathetic when the body relaxes. Of course, both are in balance through a typical day accomplishing physiological functions of the body.
There is mounting evidence that PD patients have affection in neurons of the autonomic pathways. Consequently, autonomic physiology may serve as a window into non-motor PD onset and progression of the disease. These are the most common systems that Parkinsons disease affects:
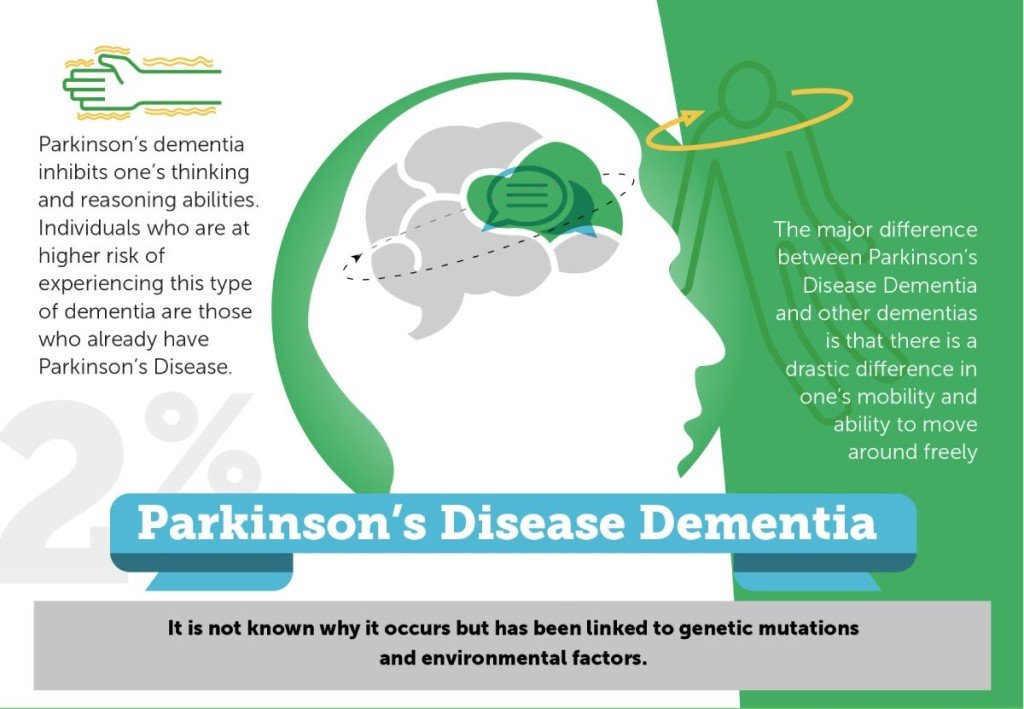
Comparison With Other Dementias
Dementia is the result of physical changes in the brain that can lead to memory loss and an inability to think clearly.
Several types of dementia exist, including:
PD dementia has different symptoms to other types.
Alzheimers dementia, for example, impairs memory and language. PD dementiam on the other hand, affects problem-solving, the speed at which thoughts occur, memory, and mood, alongside other important cognitive functions.
Dementia with Lewy bodies and Parkinsons disease dementia are similar in that the Lewy Bodies might be present in both forms.
However, whether the disease causes Lewy bodies or if Lewy bodies cause the disease symptoms is unclear. Researchers also believe that the way the Lewy bodies form in Parkinsons disease dementia is different from those in Lewy body dementia.
Parkinson’s Disease Dementia Surgery And Gene Therapy
- Great strides have been made in the surgical treatment of Parkinson’s disease. Several different procedures are now available, and they are successful in many patients in relieving movement symptoms. Unfortunately, surgery has no effect on cognitive symptoms. In fact, most people with dementia are not candidates for surgery.
- Gene therapy is in its infancy there are ongoing human and animal trials with various methods to insert genes into neuronal cells to reduce or stop Parkinson’s disease symptoms by causing cells to produce dopamine coded by the newly inserted genes. Early results with the treatment termed ProSavin are encouraging. However, it is not clear if such therapy could prevent or reverse Parkinson’s disease dementia.
You May Like: Is Parkinsons An Autoimmune Disorder
Why Do Parkinsons Patients Lose Weight
Several causes may induce weight loss. Weight loss is a non-specific symptom and could be a sign of a wide variety of medical problems, including cancer. Therefore, acute weight loss is an entity that a physician should examine to identify its cause.
Suppose the patient suffers from Parkinsons disease, and the physician does not find any other possible cause. In that case, the weight loss shall be attributed to Parkinsons.
Among PD patients, many possible causes may lead to weight loss. The reasons vary from people to people, but each one can contribute to developing weight loss. People with Parkinsons disease have a decrease in appetite, and it has various possible causes.
- The alteration, in the sense of smell, disables them from tasting food and reducing the amount of food.
- Apathy and depression
- Nausea due to medications
Asides from the appetite loss, other possible causes go along with the motor symptoms of the disease. These motor symptoms may induce an increase in energy expenditure.
- Dyskinesias are pointless and involuntary movements that can be a side effect of the treatment with levodopa.
- Essential tremor, resting tremor, and as well as muscle stiffness can be causes of excessive energy consumption and subsequent weight loss.
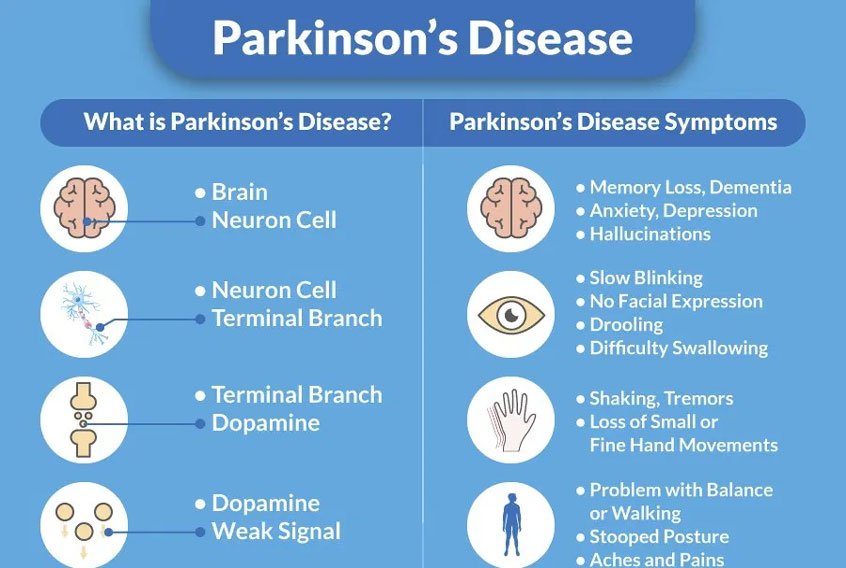
What Is Parkinson Disease
Parkinson disease is a movement disorder. It can cause the muscles to tighten and become rigid This makes it hard to walk and do other daily activities. People with Parkinsons disease also have tremors and may develop cognitive problems, including memory loss and dementia.
Parkinson disease is most common in people who are older than 50. The average age at which it occurs is 60. But some younger people may also get Parkinson disease. When it affects someone younger than age 50, it’s called early-onset Parkinson disease. You may be more likely to get early-onset Parkinson disease if someone in your family has it. The older you are, the greater your risk of developing Parkinson disease. It’s also much more common in men than in women.
Parkinson disease is a chronic and progressive disease. It doesn’t go away and continues to get worse over time.
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
What Are The Types Of Lewy Body Dementia
There are two types of LBD: dementia with Lewy bodies and Parkinson’s disease dementia.
Both types cause the same changes in the brain. And, over time, they can cause similar symptoms. The main difference is in when the cognitive and movement symptoms start.
Dementia with Lewy bodies causes problems with thinking ability that seem similar to Alzheimer’s disease. Later, it also causes other symptoms, such as movement symptoms, visual hallucinations, and certain sleep disorders. It also causes more trouble with mental activities than with memory.
Parkinson’s disease dementia starts as a movement disorder. It first causes the symptoms of Parkinson’s disease: slowed movement, muscle stiffness, tremor, and a shuffling walk. Later on, it causes dementia.
How Is Lewy Body Dementia Diagnosed
There isn’t one test that can diagnose LBD. It is important to see an experienced doctor to get a diagnosis. This would usually be specialist such as a neurologist. The doctor will
- Do a medical history, including taking a detailed account of the symptoms. The doctor will talk to both the patient and caregivers.
- Do physical and neurological exams
- Do tests to rule out other conditions that could cause similar symptoms. These could include blood tests and brain imaging tests.
- Do neuropsychological tests to evaluate memory and other cognitive functions
LBD can be hard to diagnose, because Parkinson’s disease and Alzheimer’s disease cause similar symptoms. Scientists think that Lewy body disease might be related to these diseases, or that they sometimes happen together.
It’s also important to know which type of LBD a person has, so the doctor can treat that type’s particular symptoms. It also helps the doctor understand how the disease will affect the person over time. The doctor makes a diagnosis based on when certain symptoms start:
- If cognitive symptoms start within a year of movement problems, the diagnosis is dementia with Lewy bodies
- If cognitive problems start more than a year after the movement problems, the diagnosis is Parkinson’s disease dementia
Also Check: Parkinson’s Disease Survival Rate
How Does Parkinsons Disease Develop
As the disease progresses people who have Parkinsons are increasingly likely to have a tremor, shaking, slowness of movement and rigidity. It can also cause problems with balance, sleep, swallowing, speech and increase the risk of falls. This can cause embarrassment, distress, discomfort and social isolation.
Research has indicated that in Parkinsons disease the persons cognitive processes can also be affected and these may get progressively worse over the years, with some people going onto develop dementia in the later stages of Parkinsons. The cognitive changes could include:
- forgetfulness
- a reduction in reasoning, judgement, planning and decision-making abilities
- difficulty learning new things
The person may also show signs of depression or anxiety.
What’s The Difference Between Memory Loss And Parkinson’s Dementia
Alzheimer’s dementia and Parkinson’s disease can both affect a person’s memory, but not in the same way.
Generally speaking, Parkinson’s dementia is not associated with the sort of memory loss that comes with Alzheimer’s, the most common form of dementia. Put differently: It doesn’t typically impact a person’s ability to absorb and store new memories or information the way Alzheimer’s does.
“You can learn , but it’s difficult to retrieve the information that you have in your brain,”Irene Litvan, MD, director of the Movement Disorder Center at the University of California, San Diego, tells Health. “You may not know where the cassette is, but if somebody asks you, ‘Where were you when you lost it?’ You can say, ‘Oh, I was there.'”
RELATED: Here’s How a Doctor Explains the Difference Between Alzheimer’s and Dementia
But that’s not to say Parkinson’s disease dementia doesn’t affect memory at all. On the contrary, some people with Parkinson’s dementia do indeed experience short- and long-term memory loss. They might also forget how to perform simple tasks, like how to run the dishwasher. And since Parkinson’s can affect people in different ways, there’s no way to tell whether someone with the disease will experience memory loss related to dementia.
Recommended Reading: How Long Does Someone With Parkinson Live
Living With Parkinson Disease
These measures can help you live well with Parkinson disease:
- An exercise routine can help keep muscles flexible and mobile. Exercise also releases natural brain chemicals that can improve emotional well-being.
- High protein meals can benefit your brain chemistry
- Physical, occupational, and speech therapy can help your ability to care for yourself and communicate with others
- If you or your family has questions about Parkinson disease, want information about treatment, or need to find support, you can contact the American Parkinson Disease Association.
Degeneration In The Mesocortical Dopamine Network Contributes To Executive Dysfunction
However, dopamine-dependent neural circuitry underlying executive deficits in Parkinsons disease may not be limited to the fronto-striatal network alone. The mesocortical dopamine network originates in the midbrain ventral tegmental area and projects diffusely to neocortical areas, particularly prefrontal, insular and cingulate cortices . Release of dopamine from this network modulates prefrontal D2 receptors and thereby facilitates cognitive flexibility, a core feature of executive processing . Insular cortex in particular is considered to mediate such flexibility, acting as a hub to recruit other cognitive circuits such as the fronto-parietal network . In support of this, insular lesions in human patients have been shown to impair performance on tasks requiring cognitive flexibility .
You May Like: Is Parkinson’s Disease Fatal
What Is Parkinsons Disease Dementia
Parkinsons disease dementia is a brain disorder that occurs in somebut not allpeople living with Parkinsons disease. The brain cell damage caused by the disease can lead to a loss of memory and other cognitive functions such as problem solving and speed of thinking. These changes in thinking and behavior can impact your daily living, independence, and relationships.
In those who do develop Parkinsons disease dementia, there is at least one yearand usually 10 to 15 yearsbetween the Parkinsons diagnosis and the onset of dementia. According to estimates by the Alzheimers Association, 50% or more of people with Parkinsons disease eventually experience dementia, although there are a number of risk factors that impact the likelihood of developing symptoms:
- Parkinsons patients who experience hallucinations, excessive daytime sleepiness, and more severe motor control problems are at higher risk for dementia.
- Dementia is more common in people who are older at onset of Parkinsons.
- Dementia is a bigger risk factor in non-tremor predominant Parkinsons.
- Overwhelming stress, cardiovascular disease, and adverse reactions to the Parkinsons disease drug levodopa can also indicate an increased risk for developing dementia.
- Dementia is relatively rare in people who develop Parkinsons before age 50, no matter how long they have had the disease.
Executive Dysfunction Is Due To Disruption Of The Fronto
The prefrontal cortices are implicated in executive function , and distinct areas of prefrontal cortex have strong functional connections with the striatum via parallel dopamine-dependent cortico-striatal loops . Functional MRI imaging in patients with Parkinsons disease relates executive impairments on set shifting and working memory tasks to hypo-activation within the fronto-striatal loops connecting dorsolateral and ventrolateral prefrontal cortices, striatum and thalamus . However, such hypo-activation was only present during task phases that specifically required co-activation with the striatum in controls, indicating that striatal dysfunction was the determining factor in executive impairment in Parkinsons disease rather than frontal dysfunction. Both the globus pallidus internus and caudate are heavily affected by dopaminergic degeneration , and PET studies have specifically implicated dysfunction of these two structures in interruption of normal processing in the fronto-striatal network for example, patients with Parkinsons disease demonstrating executive impairments on tasks involving planning or random number generation show significantly altered outflow activity from the pallidum to the frontal cortices. In addition, other studies have shown strong correlations between dopamine depletion in the head of the caudate and deficits on executive tasks such as object alternation and the Stroop Test .
Also Check: Parkinson’s Disease Environmental Factors
Slowed Cortical Rhythms On The Eeg Reflect Impaired Vigilance And Underlie Cognitive Fluctuation
As mentioned above the onset of impaired vigilance and fluctuating attention/cognition is particularly characteristic of progression to PDD . In tandem with its role in enhancing processing of salient stimuli, the NBM cholinergic network also plays a key role in the ascending arousal network. The NBM receives noradrenergic afferents from the locus coeruleus and glutamatergic afferents from the reticular formation and acts as an extra-thalamic relay to the cortex and limbic system . Its cholinergic projections can directly desynchronize the neocortical EEG, replacing slow synchronized delta waves with fast beta and gamma waves .
In addition, have shown that patients with PDD with significant cognitive fluctuations demonstrate pseudocyclic patterns of slow wave activity on the EEG in the delta-theta-pre-alpha range , whereas patients with PDD without fluctuations do not . This therefore implies that development of slow EEG rhythms cycling between relatively greater and lesser states of cortical arousal may represent the pathophysiological basis of cognitive fluctuation in PDD. However, further work is needed to establish the mechanisms underlying generation of such rhythms, and why some patients with PDD develop them while others do not.
What Are The Parkinson’s Disease Dementia Criteria
Many people with Parkinson’s disease experience cognitive changes , but not all of them develop full-blown dementia. So at what point does Parkinson’s disease cause dementia?
On average, Parkinson’s disease dementia happens about 10 years after a person first starts having movement problems.
“It happens many, many years after someone has developed Parkinson’s,”Lynda Nwabuobi, MD, assistant professor of clinical neurology at Weill Cornell Parkinson’s Disease and Movement Disorders Institute, tells Health. “It can be around 10 to 15 years.”
In fact, if someone shows signs of dementia early on in their Parkinson’s diagnosis , it could be that they were misdiagnosed out of the gate. “They might have dementia with Lewy bodies,” Dr. Nwabuobi explains.
Timing is the main factor in Lewy body dementia versus Parkinson’s disease dementia. While the two can look very similar, the dementia symptoms occur before motor symptoms in Lewy body dementia, and in Parkinson’s disease the reverse is true.
“If you look at the brain, it’s difficult to distinguish them,” Dr. Litvan says. “But clinically, they are different.”
Recommended Reading: Does Diet Soda Cause Parkinson’s
How Is Age Related To Pdd
Both PD and PDD are more common with increasing age. Most people with PD start having movement symptoms between ages 50 and 85, although some people have shown signs earlier. Up to 80% of people with PD eventually develop dementia. The average time from onset of movement problems to the development of dementia is about 10 years.
Lewy Body Dementia: A Common Yet Underdiagnosed Dementia
While its not a household word yet, Lewy body dementia is not a rare disease. It affects an estimated 1.4 million individuals and their families in the United States. Because LBD symptoms can closely resemble other more commonly known disorders like Alzheimers disease and Parkinsons, it is often underdiagnosed or misdiagnosed. In fact, many doctors or other medical professionals still are not familiar with LBD.
Recommended Reading: Parkinsons Life Expectancy
Memory: Medial Temporal Lobe And Corticopetal Cholinergic Networks
Memory is an all-encompassing term for the cognitive processes involved in the encoding, storage and retrieval of information. As with the other cognitive domains it is not a pure process, and is interdependent upon a person being able to orient attention to a stimulus , and use executive processes to allow retrieval in a particular context. As discussed above, patients with Parkinsons disease and PDD exhibit deficits in each of these latter processes, which means that apparent memory impairments have a multifactorial basis here. For example, patients with Parkinsons disease exhibit impaired free recall but benefit substantially from cueing, demonstrating that externally triggered retrieval is intact . Recognition memory is also intact at this stage although there is some debate about this . Overall, this indicates that memories are encoded and stored, but not independently retrieved. Performance on free recall in this group is significantly predicted by scores on executive tests, indicating that executive dysfunction contributes to retrieval failure , and is responsible for the apparent mnemonic deficit rather than a dysfunction of storage . This contrasts with Alzheimers disease where both recall and recognition are equally impaired from early on, implicating a temporal-limbic storage deficit .
Dementia Caused By Huntingtons Disease
Huntingtons disease is an inherited degenerative brain disease that affects the mind and body. It usually appears between the ages of 30 and 50, and is characterised by intellectual decline and irregular involuntary movement of the limbs or facial muscles. Other symptoms include personality change, memory disturbance, slurred speech, impaired judgement and psychiatric problems.There is no treatment available to stop the progression of this disease, but medication can control movement disorders and psychiatric symptoms. Dementia occurs in the majority of people with Huntingtons disease.
Also Check: Is Gabapentin Used For Parkinson’s Disease
Behaviors Seen In Parkinsons Disease Dementia
As dementia progresses, managing disorientation, confusion, agitation, and impulsivity can be a key component of care.
Some patients experience hallucinations or delusions as a complication of Parkinsons disease. These may be frightening and debilitating. Approximately 50 percent of those with the disease may experience them.
The best thing to do when giving care to someone experiencing hallucinations or delusions from Parkinsons disease dementia is to keep them calm and reduce their stress.
Take note of their symptoms and what they were doing before they exhibited signs of hallucinating and then let their doctor know.
This element of the disease can be particularly challenging for caregivers. Patients may become unable to care for themselves or be left alone.
Some ways to make caregiving easier include:
- sticking to a normal routine whenever possible
- being extra comforting after any medical procedures
- limiting distractions
- using curtains, nightlights, and clocks to help stick to a regular sleep schedule
- remembering that the behaviors are a factor of the disease and not the person

