What Research Is Being Done
The National Institute of Neurological Disorders and Stroke , a component of the National Institutes of Health, is the primary funder of research on the brain and nervous system. NIH is the leading funder of biomedical research in the world.
PSP is one of the diseases being studied as part of the NINDS Parkinsons Disease Biomarkers Program. This major NINDS initiative is aimed at discovering ways to identify individuals at risk for developing Parkinsons disease and related disorders, and to track the progression of these diseases. NINDS also supports clinical research studies to develop brain imaging that may allow for earlier and more accurate diagnosis of PSP.
Genetic studies of PSP may identify underlying genetic causes. Previous studies have linked regions of chromosomes containing multiple genes, including the gene for the tau protein , with PSP. Researchers hope to identify specific disease-causing mutation and are also studying how genetics and environment interaction may work together to contribute to disease susceptibility.
Animal models of PSP and other tau-related disorders, including fruit fly and zebrafish models, may identify basic disease mechanisms and lead to preclinical testing of potential drugs. Other studies in animal models focus on brain circuits affected by PSP, such as those involved in motor control and sleep, which may also yield insights into disease mechanisms and treatments.
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
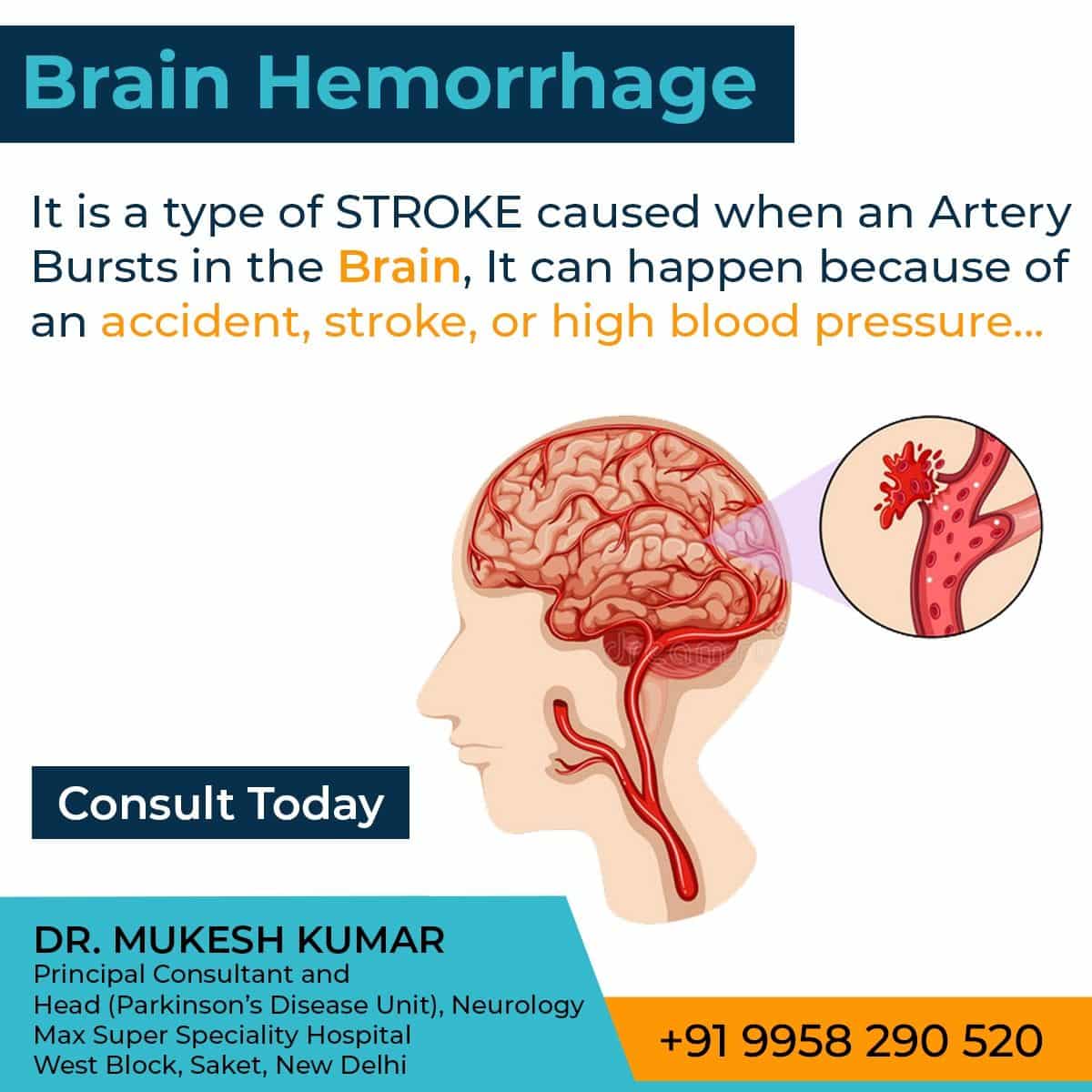
Parkinsons Disease Caused By Stroke: Vascular Parkinsonism
A stroke involving the substantia nigra or basal ganglia is called vascular Parkinsonism. Similar to other strokes, damage is caused primarily by a lack of blood supply to these regions of the brain. Generally, the strokes associated with Parkinsonism are termed small vessel strokes as they arent normally catastrophic. Diagnosis of small vessel strokes can be confirmed with diagnostic tests such as CT or MRI of the brain.
It typically takes several small strokes to produce the symptoms of vascular Parkinsonism. In some cases, small vessel strokes can also produce a type of dementia called vascular dementia. As such, it is not unusual for people who have vascular Parkinsonism to also have vascular dementia.
Read Also: Does Parkinson’s Affect Balance
Symptoms Of Peripheral Neuropathy
The symptoms of PN can be non-specific, and a person therefore may not be able to distinguish on their own whether his/her symptoms are due to PN or another condition. PN, however, often results in specific findings on a neurologic exam, such as decreased sensation to pin prick or vibration or the lack of ability to discern which way a toe is being pointed without looking. Other tests such as Electromyogram and Nerve conduction studies may be necessary to confirm the diagnosis. Small fiber neuropathy which typically causes pain, burning, tingling and/or numbness in the feet, may have normal EMG and NCS and a skin biopsy may be necessary to confirm the diagnosis. With the appropriate examination and supportive tests however, a neurologist should be able to distinguish the symptoms of peripheral neuropathy from other conditions, including PD, that may cause similar symptoms.
There are many known causes of PN including diabetes, vitamin deficiencies, certain infections, and autoimmune diseases. Many of these causes can be treated, so it is important to know if you do have PN and what the cause is. There are those people however, who have the signs and symptoms of PN, but no known cause can be identified.
Recommended Reading: What Systems Are Affected By Parkinsons Disease
Classification Of Movement Disorders
MDs can be classified into four broad categories based on phenomenological features, clinical pharmacology, and neuropathology: 1) hypokinetic disorders, which are identical with the syndrome of parkinsonism 2) hyperkinetic/choreic movement disorders 3) tremors and 4) myoclonus.
|
Table 2. Classification of MovementDisorders |
| Hypokinetic MD/ Parkinsonism |
| Uncontrollable, rapid, large amplitude flinging movements | Generally a limb | Basal ganglia Subthalamic nucleus or striatum of a limb |
|
Used with permission from: Shah S, Albin R. Movement Disorders. In: Shah S, Kelly K, eds.Emergency Neurology: Principles and Practice. New York:Cambridge University Press 1999. |
Also Check: When Was Ozzy Osbourne Diagnosed With Parkinson’s
Relationship Between Neurological Diseases And Seizures
Because epileptic seizures can often be subtle, particularly with focal onset seizures, it is unclear precisely how common they are in neurological disease patients. However, the statistics, along with supporting research, suggest that both Alzheimers disease and Parkinsons disease may be risk factors for seizures.
Epilepsy Drug May Treat Parkinsons
The epilepsy drug zonisamide may help curb the tremors and other movement problems of Parkinsons, a Japanese study shows.
Jan. 4, 2007 The epilepsy drug zonisamide may help curb the tremors and other movement problems of Parkinsons, a Japanese study shows.
Zonisamide is sold in the U.S. generically and under the brand name Zonegran.
In Parkinsons disease, the brain cells that make dopamine, a chemical that helps control the bodys movements, gradually falter and die. Symptoms include tremor, movement problems, and unsteady balance.
The disease usually starts between the ages of 50 and 65. There is no cure, but medications can help manage Parkinsons symptoms.
The new study on zonisamide for Parkinsons comes from researcher Miho Murata, MD, PhD, of Japans National Center of Neurology and Psychiatry, and colleagues. It appears in the Jan. 2 issue of Neurology.
Don’t Miss: How Does Parkinson’s Affect The Brain
Risk Of Seizures In Mds
Among the hypokinesias, Parkinsons disease is one of the most prevalent neurodegenerative disorders worldwide. The relation between PD and seizures has been controversial, with small studies showing a positive correlation, but generally with a low prevalence of seizures in patients with PD. However, a more recent study demonstrated that patients with PD who did not have any seizure-provoking comorbidity had an adjusted OR of epileptic seizures of 2.24 compared with PD-free individuals without any seizure-provoking comorbidity. Although the association between PD and seizures remains unclear, superimposed brain disorders such as cerebrovascular disease, infections, surgery and trauma tend to be more strongly associated with seizures in patients with PD.
DYT-ATP7B or Wilsons disease is a hepatolenticular degeneration due to mutations in the ATP7B gene leading to an impaired copper metabolism. Majority of patients exhibit neurological and hepatic symptoms. DYT-ATP7B may display hypokinetic or hyperkinetic movements. Seizures can occur in approximately 10% of patients, including generalised tonic-clonic and focal onset seizures. Patients with seizures more often have white matter changes than those without .
Recommended Reading: Sam Waterston Tremor
Which Medications Can Make Confusion And Hallucinations Worse
As PD progresses, non-motor symptoms including psychosis and hallucinations become more prominent both for the patient and caregivers.9 Dopaminergic medication can exacerbate these symptoms and this can be reduced through a last in, first out approach. 27,28 Medications that have an anticholinergic effect also may cause or worsen acute confusion and the anticholinergic burden in the patients medication history should be considered.29
Recommended Reading: How To Slow Parkinson’s Disease
Monitoring Changes In Neurocognitive Function To Inform Patient Care
There is a clear connection between neurological diseases and seizures, particularly between Alzheimers disease and seizures. While more research is needed to understand the true impact seizures may have on Alzheimers disease progression, it appears prolonged or recurrent seizures may lead to increased rates of cognitive decline.
Because of this, it is crucial to measure and monitor the neurocognitive function of patients who have experienced Alzheimers disease-related seizures, as this may impact patient treatment and care needs. Understanding at a detailed level how a patients function and ability to complete Activities of Daily Living are changing over time can help ensure patients care plans are effectively updated to provide the most effective care possible for each patient.
Parkinsons Disease And Cryptogenic Epilepsy
Milton C. Biagioni
1The Marlene and Paolo Fresco Institute for Parkinsons & Movement Disorders, NYU Langone Medical Center, New York University School of Medicine, New York, NY, USA
2Department of Neurology, Baylor Scott & White Healthcare, Austin, TX, USA
Abstract
Epilepsy is an uncommon comorbidity of Parkinsons disease and has been considered not directly associated with PD. We present five patients who had concomitant PD and cryptogenic epilepsy. Although rare, epilepsy can coexist with PD and their coexistence may influence the progression of PD. While this may be a chance association, an evolving understanding of the neurophysiological basis of either disease may suggest a mechanistic association.
1. Introduction
Parkinsons disease is traditionally considered primarily a subcortical disorder with late cortical involvement. There is, however, mounting evidence of considerable cortical involvement, even in the early stages of PD . The damage seems to involve, at least in part, the simultaneous processes of both the diffuse progressive deposition of alpha-synuclein and the secondary biological changes that disrupt neural connectivity . These processes reinforce the concept of dysfunctional neural networks as a potential basis of symptomatology in PD .
2. Methods
Competing Interests
Recommended Reading: How Soon Will There Be A Cure For Parkinson’s
Alzheimers Disease As Risk Factors For Seizures And Epilepsy
Typically, Alzheimers-related seizures occur in the later stages of Alzheimer’s disease . Additionally, seizures are more likely to occur in those with early-onset Alzheimers, particularly when a familial presenilin I mutation is present.
The precise mechanism that triggers seizures in Alzheimers disease patients is not yet clear. However, damage and structural changes in the brains of those with Alzheimers disease are likely to play a role in the increased seizure risk. Additionally, researchers have hypothesized that the buildup of amyloid and tau proteins in the brain may make neurons more excitable, as they are known to interfere with neuron-to-neuron communication. When nerve cells become hyper-excitable, they can behave uncontrollably, causing epileptic seizures.
Parkinsons Disease Risk Factors
Hypertension and Type 2 diabetes were associated with an increased risk of developing Parkinsons disease in East London a stronger association was found between memory complaints in this group than previously observed. East London has one of the highest proportions of Black, South Asian, and other mixed/ethnic groups, which comprise 45% of residents in the area, compared to 14% in the rest of the UK. Furthermore, 80% of the studys participants were from low-income households.
Lead study author Dr Cristina Simonet, neurologist and PhD student at the Queen Mary University of London, commented: This is the first study focusing on the pre-diagnostic phase of Parkinsons in such a diverse population with high socioeconomic deprivation but universal access to health care. People from minority ethnic groups and deprived areas have largely been underrepresented in Parkinsons research up till now, but to allow us to get a full picture of the condition, we need to ensure research is inclusive and represents all those affected.
This study confirms that many of the symptoms and early features of Parkinsons can occur long before a diagnosis. Through our ongoing PREDICT-PD research, were hoping to identify people at high risk of Parkinsons even before obvious symptoms appear which means that we could do more than just improve quality of life for patients, and perhaps be in the position to slow down or cure Parkinsons in the future.
Read Also: Novo Nordisk Parkinson’s Disease
New Signs Risk Factors For Parkinson’s Disease
The goal of the study, conducted by researchers at the Queen Mary University of London, was to investigate risk factors and prediagnostic symptoms in an ethnically diverse population since most Parkinson’s research has been done in predominantly white, affluent populations.
To do this, scientists analyzed the medical records of over 1 million people living in East London between 1990 and 2018. The researchers chose East London, specifically, because it offered a highly diverse population with “high socioeconomic deprivation,” the study said. In East London, about 45% of residents are Black, South Asian, mixed, or belonging to another ethnic group.
One of the most “notable” findings, according to researchers, was that having epilepsy was associated with a higher risk of developing Parkinson’s. Though researchers said drug-induced Parkinson’s could not be ruled out in this case, this isn’t the first time epilepsy has been linked to Parkinson’s disease: Case reports from 2016 found that Parkinson’s and epilepsy can coexisteither by predating a Parkinson’s diagnosis or developing after one.
Though study authors agree that more research is needed regarding hearing loss and its link to Parkinson’s, they suggest it’s part of the impairment in sensory processing that occurs with Parkinson’s disease. That impairment may manifest in different ways: through sight, hearing, or even sense of smell, researchers said.
Parkinsons Disease As Risk Factors For Seizures And Epilepsy
A 2018 cohort study with a nested case-control analysis found that among 23,086 individuals with incident Parkinsons disease and 92,343 individuals without Parkinsons disease, 898 patients with incident epileptic seizures were identified. This suggests that incident Parkinsons disease is associated with an increased risk of incident epileptic seizures.
The mechanism that triggers seizures in Parkinsons disease is not yet clear. However, decreased cortical inhibition and increased cortical excitability have been reported in both Parkinsons and epilepsy patients, meaning this hyperexcitable state may contribute to the onset of epileptiform activity in Parkinsons disease patients.
Read Also: Does Parkinson’s Show Up On A Ct Scan
How Is Tremor Diagnosed
Tremor is diagnosed based on a physical and neurological examination and an individuals medical history. During the physical evaluation, a doctor will assess the tremor based on:
- whether the tremor occurs when the muscles are at rest or in action
- the location of the tremor on the body
- the appearance of the tremor .
The doctor will also check other neurological findings such as impaired balance, speech abnormalities, or increased muscle stiffness. Blood or urine tests can rule out metabolic causes such as thyroid malfunction and certain medications that can cause tremor. These tests may also help to identify contributing causes such as drug interactions, chronic alcoholism, or other conditions or diseases. Diagnostic imaging may help determine if the tremor is the result of damage in the brain.
Additional tests may be administered to determine functional limitations such as difficulty with handwriting or the ability to hold a fork or cup. Individuals may be asked to perform a series of tasks or exercises such as placing a finger on the tip of their nose or drawing a spiral.
The doctor may order an electromyogram to diagnose muscle or nerve problems. This test measures involuntary muscle activity and muscle response to nerve stimulation.
Also Check: Can A Blood Test Detect Parkinsons
Causes Of Parkinsons Disease
Parkinsons disease typically occurs when nerve cells in the basal ganglia either die or become impaired. The nerve cells in the basal ganglia hold paramount significance as they produce an essential brain chemical known as dopamine.The death of nerve cells results in a decrease in dopamine production, which causes several movement disabilities that are commonly seen in PD patients. Despite extensive research, scientists have been unable to root out the reasons that cause the dopamine-producing cells to die.
Patients with Parkinsons disease also lose the nerve endings that are responsible for producing norepinephrine. Norepinephrine is the primary chemical messenger of the sympathetic nervous system and controls several body functions, including blood pressure and heart rate.However, a loss of norepinephrine can be considered the reason behind the non-movement symptoms that line PD. These include irregular blood pressure, a sudden drop in blood pressure at the slightest movements such as when a person stands up from a laying down or sitting position, and diminished movement of food through the digestive tract.
Recommended Reading: Does Exercise Slow The Progression Of Parkinson’s
Other Reasons For Cognitive Symptoms
Besides PD, there are other important causes of cognitive dysfunction to keep in mind. Medical illnesses such as thyroid disease or vitamin B12 deficiency can cause cognitive symptoms. Urinary tract infections or pneumonia can acutely cause confusion or hallucinations. In these settings, the cognitive symptoms are generally reversible after the infection or medical condition is treated. One should be aware that some medications for pain or bladder problems may cause sedation/sleepiness or confusion, and, thereby, impair cognitive function.
Recommended Reading: Parkinsons Foundation Miami Florida
Epilepsy Could Be A Risk Factor For Developing Parkinsons Disease Study Suggests
Epilepsy and hearing loss are among some of the risk factors for developing Parkinsons disease later in life, according to a new study in JAMA Neurology.
Dr Christina Simonet and colleagues aimed to investigate common risk factors for Parkinsons disease and how early these can occur before a Parkinsons disease diagnosis is made. The research wanted to focus on an ethnically diverse group of people from less affluent backgrounds.
The study used the electronic health records from GP practices in East London of over a million people between 1990 and 2018. They compared people with Parkinsons disease stated in their medical record to those without. People with neurological diseases that get worse with time, such as dementia and multiple sclerosis , were not included in the study.
The researchers found that people with Parkinsons disease tended to be older and more often male, compared to the group without. Loss of hearing and epilepsy were found to be risk factors for Parkinsons disease, which havent been well reported before.
According to the NHS website, Parkinsons disease is thought to affect around one in every 500 people. The researchers found that people with epilepsy are 2.5 times more likely to be diagnosed with Parkinsons disease than the general population. This means for every 500 people with epilepsy, two or three people will go on to have a diagnosis of Parkinsons disease.
There is more information on this study on the JAMA Neurology website.
You May Like: Can Mold Cause Parkinson’s Disease
Relationship Between Disrupted Neuronal Connectivity And Epileptic Seizures
Epilepsy is considered a disease of network dysfunction.47,48 At a microscopic level, both simple and complex partial seizures involve disruptions in the excitatory interactions between cerebral cortex pyramidal cells.49 From a neurophysiology view, the EEG-graphic representation of an epileptic event is characterized by the paroxysmal onset of hyper-synchronized sharp waves disrupting the neuronal background activity. This activity is often multifocal, reflecting a broader network dysfunction.50,51 Moreover, TMS studies demonstrate similar neurophysiologic features between epilepsy and PD characterized by a state of increased cortical excitability as indicated by reduced intra-cortical inhibition and increased intra-cortical facilitation observed in both patient populations.25,52â55 As mentioned before, in PD, cortical neurons innervating the basal ganglia become hyperexcitable, possibly as a compensatory mechanism following the incremental rise in the output threshold of striatal dopaminergic neurons. As such, it would not be surprising if this putatively maladaptive phenomenon may eventually lead to the generation of epileptiform activity. While epidemiologically, epilepsy-increased comorbidity in patients with PD remains questioned,13,56 our group published the largest case series of patients with PD with concomitant epilepsy57 raising the possibility that epileptic activity in these patients may indeed be under-diagnosed and under-recognized.
