Is Parkinson’s An Autoimmune Disease
- Date:
- Columbia University Medical Center
- Summary:
- The cause of neuronal death in Parkinson’s disease is still unknown, but a new study proposes that neurons may be mistaken for foreign invaders and killed by the person’s own immune system, similar to the way autoimmune diseases like type 1 diabetes, celiac disease, and multiple sclerosis attack the body’s cells.
The cause of neuronal death in Parkinson’s disease is still unknown, but a new study proposes that neurons may be mistaken for foreign invaders and killed by the person’s own immune system, similar to the way autoimmune diseases like type I diabetes, celiac disease, and multiple sclerosis attack the body’s cells. The study was published April 16, 2014, in Nature Communications.
“This is a new, and likely controversial, idea in Parkinson’s disease but if true, it could lead to new ways to prevent neuronal death in Parkinson’s that resemble treatments for autoimmune diseases,” said the study’s senior author, David Sulzer, PhD, professor of neurobiology in the departments of psychiatry, neurology, and pharmacology at Columbia University College of Physicians & Surgeons.
The new hypothesis about Parkinson’s emerges from other findings in the study that overturn a deep-seated assumption about neurons and the immune system.
The researchers then confirmed that T cells recognized and attacked neurons displaying specific antigens.
Story Source:
Journal Reference:
Cite This Page:
Early Signs Of Autoimmunity
The authors of the present study report the case of a male whose blood contained T cells that reacted to alpha-synuclein at least a decade before doctors diagnosed him with Parkinsons disease.
This tells us that detection of T cell responses could help in the diagnosis of people at risk or in early stages of disease development, when many of the symptoms have not been detected yet, says LJI professor Alessandro Sette, a corresponding author of the new study.
Importantly, we could dream of a scenario where early interference with T cell responses could prevent the disease from manifesting itself or progressing.
The male began to experience motor symptoms in 2008 and received a diagnosis of Parkinsons disease in 2009, at the age of 47.
He contacted the scientists at LJI after reading about their earlier study and offered to donate samples of his blood that had been taken between 1998 and 2018 for an unrelated purpose.
The samples revealed that as far back as 1998, T cells in his blood were targeting alpha-synuclein.
In other words, there was autoimmune reactivity at least 10 years before he began to develop motor symptoms.
Genetic Regulation Of Autoimmunity In Pd
In addition to these observations, DJ-1 has also been reported to affect the development of natural Tregs and induced Tregs . Mature Tregs with normal function, which modulate not only adaptive immunity but also innate immunity, are pivotal for maintaining thymic function, peripheral immune self-tolerance and immune system homeostasis. nTregs are generated in the thymus, while iTregs are derived from naïve CD4+ T cells encountering antigens in the peripheral organs. Both cell types are generally immunosuppressive through the suppression or downregulation of effector T cell proliferation . Their self-check function successfully prevents excessive effector cell reactions. On the other hand, the abnormal proliferation of both types of Tregs leads to the failure of self-/non-self-discrimination, resulting in autoimmune disease . Evidence reported by Singh et al. has demonstrated that DJ-1, one of the most classical key players responsible for PD pathogenesis, is strongly linked with neuroimmunology and multiple autoimmune responses in PD . In addition, DJ-1-deficient animal models have shown compromised iTreg induction, cell cycle progression, and cell survival and proliferation. DJ-1/ iTregs are more proliferative, more susceptible to cell death signals and deficient in cell division compared with wild type counterparts, as analyzed by flow cytometry and Western blotting.
Don’t Miss: Does Parkinson’s Cause Memory Issues
Changes In T Cell Subpopulations And Cytokines
Consistent with the systemic view that PD involves multiple systems and tissues, several studies have shown general alterations in cytokines and immune cell populations.
Proinflammatory cytokines are elevated in the blood of PD patients, including increased levels of IL-2 6 8 , MCP-1 , MIP-1 , RANTES , TNF , and IFN . Increased levels of proinflammatory cytokines and chemokines are indicative of an immune system responding to tissue damage and/or foreign molecules. The levels of cytokines and chemokines correlate with the clinical stage of the disease, highlighting a role for peripheral inflammation in PD progression . Altered T cells populations can also contribute to the changes in circulating cytokines. Th1 and TH17+ CD4+ cells can contribute to the increased levels of IFN, TNF, and IL-17 .
Investigating Parkinsons As An Autoimmune Disease
At the University of Montreal, Professor Louis-Eric Trudeau investigates the earliest potential causes of Parkinsons disease, at the cellular level. His project is funded by the Saucier-van Berkom Parkinson Quebec Research Fund with contributions from Parkinson Newfoundland & Labrador, in the amount of $49,748.00 for 1 year. He is exploring the possibility that Parkinsons is a form of autoimmune disease, caused when the immune system attacks the axon terminals in our brain cells. Those extremities release the chemical messengers that communicate with other cells, and damage to such terminals may disrupt the dopamine-producing brain cells that are key to Parkinsons.
The death of the brain cells that produce dopamine, the chemical messenger that signals other cells involved in motor control, triggers the symptoms of Parkinsons disease. But researchers still dont know exactly what causes those dopamine-producing cells to die.
Trudeau, a neuroscientist, investigates the possibility that an autoimmune attack on those dopamine cells is the culprit.
Trudeau and his immunologist colleague, Michel Desjardins, are studying the role of the portion of cells called axon terminals. These terminalsthe root-like extremities of cellsrelease the chemical messengers that send communication signals. Trudeau believes the death of these terminals, before the death of the dopamine cells themselves, is where the trouble starts.
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Immune Cells And Autoimmunity In Pd
To date, numerous immune cells have been shown to be responsible for driving PD progression. DCs and microglia are two types of mammalian immune cells that act as the first and main forms of active immune defense in the CNS . They act first as APCs and then activate T cells to initiate the immune system to identify and attack extrinsic antigens. In essence, these immune cells lie at the intersection of the immune response and the neurodegenerative processtwo primary aspects of CNS autoimmune disorders. DCs, the famous APCs , serve as messengers between the innate and adaptive immune systems and can induce and even maintain self-tolerance . It is the differentiation/maturation rather than the haematopoietic origin or subset classification of DCs that determines their tolerogenic or immunogenic functions. Immature DCs can inhibit alloantigen-specific T cell responses to reverse autoimmune diseases in murine models but simultaneously induce antigen-specific T cell tolerance . The maturation of DCs into professional APCs via the upregulation of MHC expression enables DCs to capture antigens successfully . Based on these phenomena, Platt et al. proposed a theory called regulatory mechanisms by DCs for immune responses against self-antigens. They concluded that the failure of DCs to control T cells via Treg differentiation and effector T cell clonal deletion leads to a direct attack on self-antigen-harboring target cells .
In Vitro Studies Of Ipsc
A recent in vitro study using induced-pluripotent stem cells -derived midbrain neurons and T cells from PD patients was the first to show that PD patient-derived T cells can kill dopamine neurons directly. Sommer et al. determined that PD patients contain significantly higher Th17 cells than healthy controls . The PD patient-derived Th17 cells exerted cytotoxic effects on neurons by releasing IL-17A, a cytokine detected by IL-17R expressed on neurons . The iPSC in vitro cultures lacked glia, which express MHC-II and can potentially interact with Th17 cells. In addition, T cells were activated non-specifically, and so the antigen specificity of Th17 cells remains unclear . While the study indicates that PD-derived T cells can directly kill dopaminergic neurons, the omission of professional antigen presenting cells, antigenicity, and neuronal specificity in the cultures in this initial study overlooks the role of multiple relevant in vivo factors important for disease progression. Moreover, the mode of action that garners specific vulnerability of dopaminergic neurons and avoids unaffected neurons was not resolved in this study. Nevertheless, the study indicates Th17 cells may participate in PD-related neuronal death.
Recommended Reading: Can You Die From Parkinson’s Disease
Potential New Treatment Strategies For Parkinson’s
This new finding provides additional knowledge and understanding of the disease processes that are present in PD and opens the door for using immunotherapies, drugs that suppress the abnormal immune response seen in autoimmune disorders. Additional research is needed to understand the molecular steps that occur in PD and the immune response, but researchers are hopeful that an immunotherapy strategy could help to prevent or lessen worsening symptoms in people with PD.1,2
The Role Of Mhc Proteins In Pd Pathogenesis
T cells recognize a complex formed between MHC molecules and a peptide epitope. The epitope is presented to T cells as a result of a complex series of events termed antigen processing and presentation that involve the intracellular degradation of self and foreign proteins into peptides that are then loaded onto the antigen-binding groove of MHC molecules. In general, T cells recognize peptides derived from foreign molecules, but in disease some T cells also evade self-tolerance and can recognize self-peptides. MHC class I in general presents peptides derived from the same cell , while MHC class II typically present peptides derived from extracellular proteins .
Mature neurons are generally thought to lack MHC expression and so to not present antigens. However, SN and LC neurons recently have been shown to express MHC-I and co-localize with CD8+ T cells in response to stimuli such as IFN . Catecholamine neurons are particularly sensitive to inflammation in comparison to other neuron types. A lower amount of IFN is required by dopaminergic neurons to express MHC-I in comparison to other neuronal subtypes. The MHC-I presented by dopaminergic neurons is functional and can result in cytotoxicity in the presence of matching antigen and CD8+ T cells . Dopaminergic neuron sensitivity to inflammation and corresponding MHC-I upregulation could render them susceptible to infiltrating T cells versus neighboring, more resistant GABAergic neurons.
Don’t Miss: Can You Die From Parkinson Disease
What Are Autoimmune Diseases
Autoimmune diseases are inflammatory conditions in which the immune system targets the healthy tissues of the host by mistake .
Currently, the reasons for such dysregulated immune reactions are unknown . When the autoimmune attack is mounted against the brain, it leads to the development of neurological disorders such as Multiple Sclerosis .
In the case of MS, immune T-cells attack the myelin sheath of the neurons in the brain, which damages their ability to transmit signals and function properly .
Treatment options are extremely limited and include medications that suppress the immune system or simply subdue the symptoms. Unfortunately, most of these medications have common side effects.
Parkinsons Disease Linked With Autoimmunity
Parkinsons disease is a degenerative disorder that mainly affects the motor system. Symptoms include shaking, slow movement, and difficulty walking. Diagnosis usually occurs in people over 60 but early onset PD can occur in patients with a shortened life expectancy. In advanced stages, depression and dementia are also associated with the disease. The cause of Parkinsons is believed to be both genetic and environmental and there is no known cure. PD involves the death of vital neurons in the brain. Some of these neurons produce dopamine which is essential for movement and coordination. As PD progresses, the amount of dopamine decreases. Initial treatment is typically with L-DOPA, to increase dopamine levels, and diet and exercise may also improve symptoms. We previously reported on the modulation of NAD+ levels leading to neuroprotective effects in a model of Parkinsons disease.
Also Check: What Are The Four Cardinal Signs Of Parkinson’s Disease
The Connection Between The Immune System & Parkinson’s
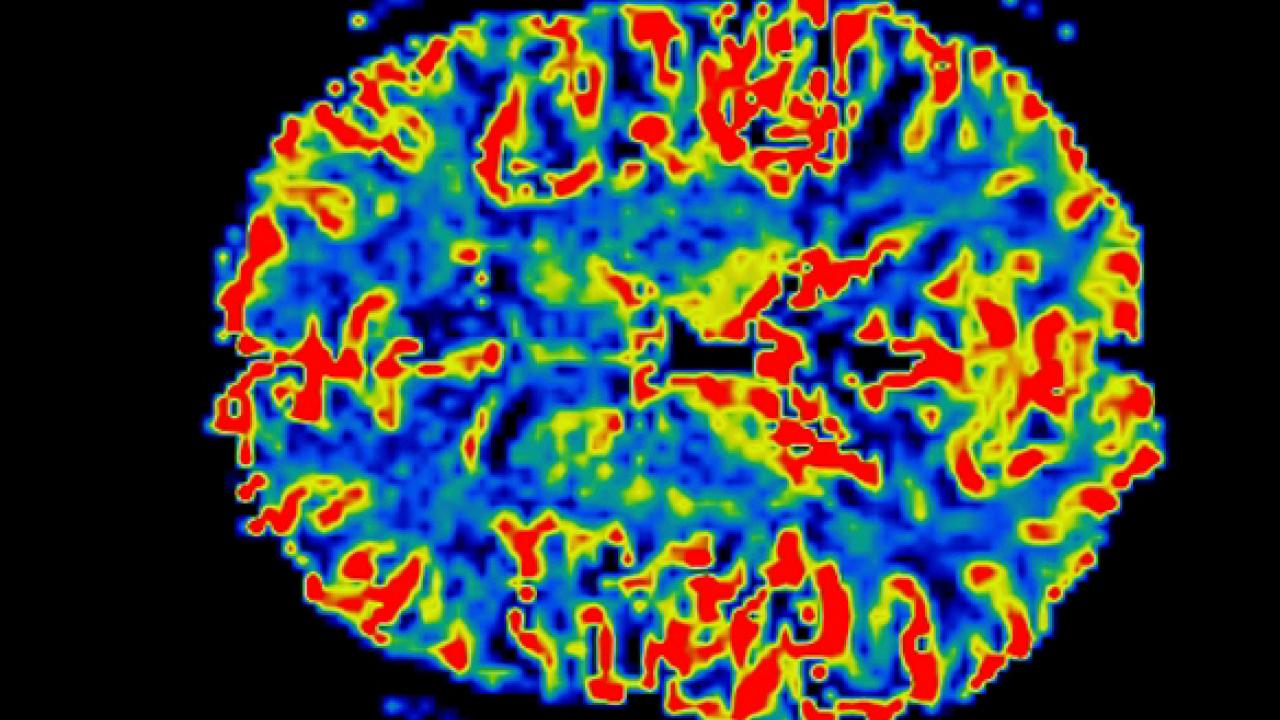
In the recent study, researchers from Columbia University Medical Center and the La Jolla Institute for Allergy and Immunology collected blood samples from 67 people with PD and 36 age-matched healthy control subjects. The blood was then exposed to fragments of alpha-synuclein and other proteins that are found in neurons.
In the healthy controls, there was little immune activity detected, but in the blood samples from people with PD, there was a significant response. Researchers believe that the T-cells in people with PD have been primed to recognize alpha-synuclein from past exposure the exposure being the presence of Lewy bodies in the brain. The immune response seen in the study subjects with PD was associated with a common gene variant that is known to affect the immune system, a gene variant that is common in people with PD.
Researchers hypothesize that autoimmunity in people with PD may develop when the neurons are no longer able to rid themselves of the abnormal accumulations of alpha-synuclein. In normal, healthy cells, old or damaged proteins are broken down and eliminated, but this process is not functioning properly in PD. When alpha-synuclein begins to form clumps, the immune system may mistakenly see it as a pathogen that needs to be attacked.1,2
Is There A Cure For Parkinsons

Theres currently no cure for Parkinsons, a disease that is chronic and worsens over time. More than 50,000 new cases are reported in the United States each year. But there may be even more, since Parkinsons is often misdiagnosed.
Its reported that Parkinsons complications was the
Complications from Parkinsons can greatly reduce quality of life and prognosis. For example, individuals with Parkinsons can experience dangerous falls, as well as blood clots in the lungs and legs. These complications can be fatal.
Proper treatment improves your prognosis, and it increases life expectancy.
It may not be possible to slow the progression of Parkinsons, but you can work to overcome the obstacles and complications to have a better quality of life for as long as possible.
Parkinsons disease is not fatal. However, Parkinsons-related complications can shorten the lifespan of people diagnosed with the disease.
Having Parkinsons increases a persons risk for potentially life threatening complications, like experiencing:
- falls
Parkinsons often causes problems with daily activities. But very simple exercises and stretches may help you move around and walk more safely.
Recommended Reading: Does Restore Gold Work For Parkinson’s
Potential For Ibogaine In The Treatment Of Parkinsons And Autoimmune Diseases
Ibogaine is an alkaloid derived from the African shrub Tabernanthe iboga. Aside from its psychoactive and anti-addiction properties, it has beneficial effects on certain neurotrophic factors and receptors in the brain. Targeting them has shown great potential for the future therapy of neurodegenerative and neuroinflammatory conditions such as Parkinsons.
Parkinsons disease is a crippling neurological disorder that affects more than 1 million people in the US. The number of people with the condition is expected to increase by more than 60% in the next 20 years . Currently, its cause is unknown but new evidence suggests that its main pathogenetic mechanism might be related to an autoimmune reaction that is present even before the onset of the first symptoms.
Autoimmune diseases are debilitating conditions that affect about 5% of the population. Currently, there is no cure for Parkinsons or other autoimmune disorders. The treatment options aim at reducing symptoms, preventing complications, and prolonging life.
The Future Of Parkinsons Treatment
While this research doesnt prove anything definitive, its definitely promising. These studies on autoimmunity could open new avenues on how PD can be treated, especially at the early stages, and even diagnose it before the motor symptoms appear, Paredes says. In the future, doctors may be able to intervene with early therapies when they start noticing early symptoms of Parkinsons, such as changes in the gut microbiome or T cells attacking the brain. Paredes explains that these treatments could involve immunomodulatory drugs, antibiotics or antivirals, or probiotics.
Still, there is much for researchers still to learn. The immune system is very complex, and our understanding is imperfect at best, Beck notes. He calls to mind autoimmune diseases like rheumatoid arthritis and juvenile diabetes, which are still at varying stages of treatment development and prevention research. I am hopeful that progress will be made, Beck asserts. However, like a financial portfolio, a diversity of research investments will be the key to understanding and stopping PD. This research represents another critical step forward in combatting Parkinsons disease, so that hopefully younger generations will be able to halt the disorder before it progresses.
You May Like: What Effect Does R Dopa Have On Parkinson’s Disease
Scientists Link Immune Cells To Parkinson’s Disease Onset
- Date:
- La Jolla Institute for Immunology
- Summary:
- A new study adds increasing evidence that Parkinson’s disease is partly an autoimmune disease. In fact, the researchers report that signs of autoimmunity can appear in Parkinson’s disease patients years before their official diagnosis.
A new study co-led by scientists at the La Jolla Institute for Immunology adds increasing evidence that Parkinson’s disease is partly an autoimmune disease. In fact, the researchers report that signs of autoimmunity can appear in Parkinson’s disease patients years before their official diagnosis.
The research could make it possible to someday detect Parkinson’s disease before the onset of debilitating motor symptoms — and potentially intervene with therapies to slow the disease progression.
The study, published in the April 20, 2020, issue of Nature Communications, was co-led by LJI professor Alessandro Sette, Dr. Biol. Sci, and Professor David Sulzer, Ph.D., of the Columbia University Medical Center.
Scientists have long known that clumps of a damaged protein called alpha-synuclein build up in the dopamine-producing brain cells of patients with Parkinson’s disease. These clumps eventually lead to cell death, causing motor symptoms and cognitive decline.
The researchers hope to study more Parkinson’s patients and follow them over longer time periods to better understand how T cell reactivity changes as the disease progresses.
Story Source:
