Exclusion Of Atypical Parkinsonism
The umbrella term atypical parkinsonism covers neurodegenerative disorders that feature rapidly progressive parkinsonism together with additional, often debilitating symptoms that are uncharacteristic for idiopathic PD. MSA, PSP and CBD fall under this category. Neuropathologically, PD and MSA share prominent alpha-synuclein inclusion pathology. Intriguingly, inclusion bodies in MSA patients are predominantly seen in oligodendrocytes, whereas Lewy bodies are mostly seen in the cytoplasm of neurons. In contrast to these disorders, PSP and CBD are considered to be tauopathies with 4-repeat tau protein accumulation. For adequate patient counselling, it is important to recognize these atypical disorders since the natural course of these disorders and treatment options are different from PD. In addition, to reduce between-subject heterogeneity in interventional trials, early and accurate diagnosis is at utmost importance. However, on clinical grounds, degenerative parkinsonian disorders can be indistinguishable from one another in early disease stages and, therefore, additional investigations such as MRI may become necessary to correctly diagnose patients with atypical parkinsonism .
Structural MRI with conventional MRI sequences
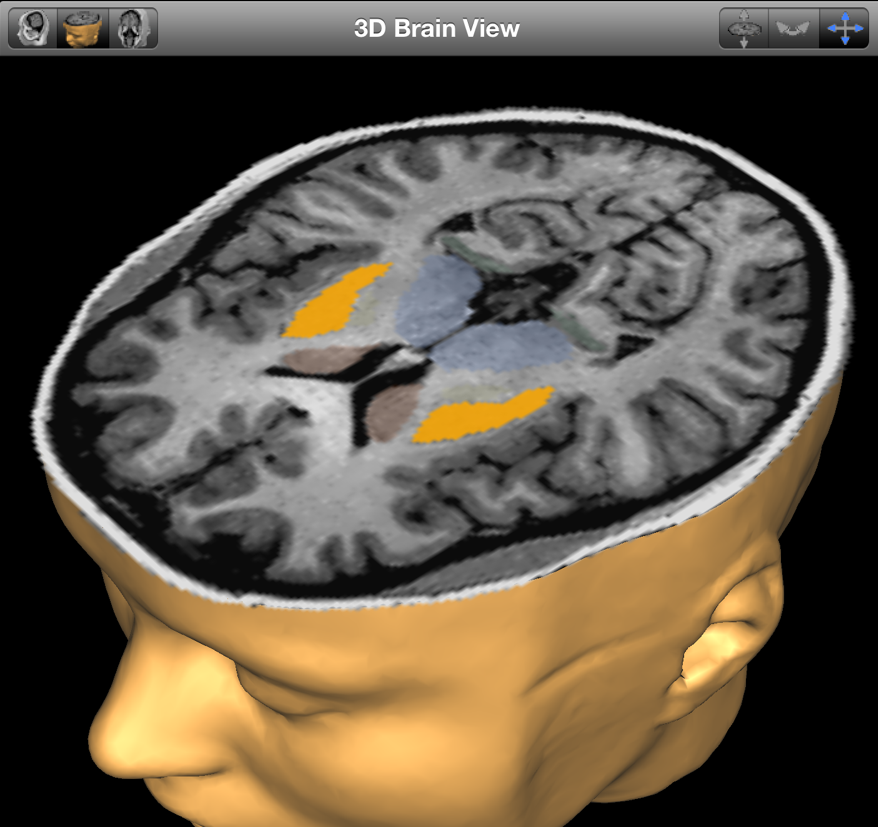
Modified from Neuroimaging of Movement Disorders,Structural MRI in Idiopathic Parkinson Disease and Parkinsonism, Volume 44 of the series Current Clinical Neurology, 2013, pp 105-128, Mueller C et al., with permission of Springer
Quantitative MRI
Tractography And Anatomical Connectivity
Tractography is a technique based on the anisotropy of water diffusion that allows reconstructing fibre tracts in the brain. Tracks are reconstructed by assuming that the main direction of diffusion in a voxel indicates the local orientation of white matter fibres . Using tractography, diffusion measures and connectivity measures can be calculated within the specific fibre tracks. Tractography has also been successfully used to parcel out the SN and the basal ganglia into specific territories .
In PD, reduced connectivity was observed between the SN and ipsilateral putamen and thalamus as well as in the sensorimotor circuit of the basal ganglia . Automated diffusion-based parcellation of SN subregions showed that the SNr and SNc in PD patients showed a general atrophy . Tractography is therefore used to investigate changes in anatomical connectivity in PD patients .
Why Is A Pet Scan Used In Parkinson’s Disease
For patients with Parkinson’s disease , a PET scan is used to assess activity and function of brain regions involved in movement. However, doctors may request a PET scan for many different reasons. Aside from potential problems in the brain and spinal cord, the test can also be used to diagnose heart problems as well as certain kinds of cancer, including breast, brain, lung, colon, and prostate cancers and lymphoma.
Recommended Reading: How Does Parkinson’s Begin
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinsons disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinsons disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinsons disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinsons disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinsons disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
What Is Parkinsons Disease
Parkinsons disease is a chronic neurological condition. It is progressive and symptoms worsen over time. It is named after Dr James Parkinson who first described the condition in 1817.
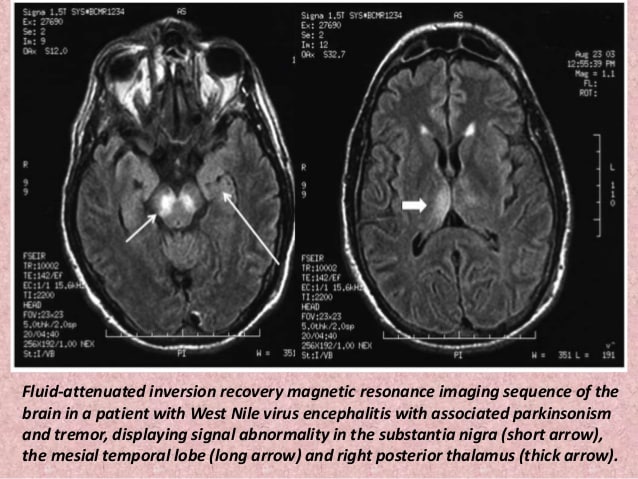
People with Parkinsons disease experience a loss of nerve cells in the part of their brains responsible for controlling voluntary movements. This part of the brain is called the substantia nigra . The nerve cells in the substantia nigra usually produce a chemical called dopamine which helps transmit messages from the brain to the rest of the body via the central nervous system . As these cells are lost, people with Parkinsons disease experience a loss of dopamine and the messages controlling movement stop being transmitted efficiently.
Parkinsons disease is more common as people get older but it can affect younger adults. Men tend to be affected in slightly higher numbers than women.
Read Also: What Is Good For Parkinson’s Disease
Does Parkinsons Affect Voice
The voice is affected too, because the voice box is ultimately controlled by the basal ganglia as well. Thus the voice becomes soft, slurred and hushed. Others may comment that the patient is mumbling. The mumbling goes away temporarily once the patient becomes aware of it but soon returns to the soft, slurred state.
This temporary improvement when attention is paid is true of many of the motor symptoms of PD because the condition primarily affects subconscious movements, and does not directly affect nerve or muscle control at the most basic level. Thus, conscious awareness can override the slowness to a certain extent. This fact is one reason why physical therapy and physical activity are so useful and necessary in treating PD.
- Slowness of walking and other movements
- Trouble with dexterity
Imbalance, loss of balance reflexes
- May fall backwards
Datscan: A Test To Help In The Diagnosis Of Parkinsons
In 2011, the Food and Drug Administration approved an imaging test to help diagnose PD. In this test, a radioactive tracer, Ioflupane 123I, also known as DaTscan, is injected into the blood, where it circulates around the body and makes its way into the brain. It attaches itself to the dopamine transporter, a molecule found on dopamine neurons. Several hours after the tracer has been injected, special imaging equipment scans the head to detect the presence of DaTscan.
People with PD will typically have a smaller signal in a part of the brain called the striatum, where the ends of the dopamine neurons are meant to be. Here is a normal scan on the left, which would indicate a healthy dopamine system, next to an abnormal scan on the right, which would indicate an unhealthy dopamine system.
It is important to note that conventional MRI imaging will appear normal in PD and is therefore not helpful in confirming the diagnosis. Other atypical parkinsonian conditions, such as vascular parkinsonism however, can have abnormalities on MRI, so the test may be done to rule out other diagnoses.
Also Check: Are Weighted Blankets Good For Parkinson’s
What Should I Expect During The Mri
As the MRI scan begins, you will hear the equipment making a variety of banging, clanging and muffled thumping sound that will last for several minutes. None of them are anything other than annoying. Other than the sound, you should experience no unusual sensations during the scanning.
Certain MRI exams require an injection of a contrast material. This helps identify certain anatomic structures on the scan images.
Please feel free to ask questions. Tell the technologist or the doctor if you have any concerns.
Looking For Signs Of Parkinsons
Your specialist will examine you to look for common signs of Parkinsons. You may be asked to:
- write or draw to see if your writing is small or gradually fades
- walk to see whether theres a reduction in the natural swing of your arm or in your stride length and speed
- speak to see if your voice is soft or lacks volume
The specialist will also look at and ask you about your:
- face to see if there is a masked look or if you have difficulty with facial expressions
- limbs to see if you have a tremor, any stiffness or slowness of movement
As well as examining you for any of the typical signs of Parkinsons, the specialist will also look for signs that may suggest a different diagnosis.
It may be helpful to take someone with you for support when seeing a specialist. Taking a list of questions you want to ask can also be useful so you dont forget to mention something you want to know about. If a healthcare professional says something you dont understand, dont be afraid to ask them to explain what they mean.
Read Also: Can Parkinson’s Cause Weakness In The Legs
Differences Between Parkinsons Disease And Atypical Parkinsonism
The symptoms of Parkinsons disease and atypical parkinsonism overlap, and in a clinical setting, it can be hard to tell if a patient has one or the other. Atypical parkinsonism is diseases that present some of the signs and symptoms of Parkinsons Disease but do not respond well to drug treatment. With an MRI, your doctor can help to make the diagnosis more accurate, which is essential for quality treatment. Additionally, an MRI can also help your medical team to determine if you have a certain type of atypical parkinsonism. This can help to create a prognosis and guide your treatment options.
Mri And Pet Reveal Parkinsons Is Two Diseases
Advanced imaging shows Parkinsons can begin as brain-first or body-first.
Its been a long-standing question in neuroscience: is Parkinsons more than one disease? Now, thanks to MRI and PET scans, clinicians have an answer yes. And, having this knowledge could pave the way for personalized medicine for these patients.
Based on the analysis of advanced imaging scans, researchers have determined that Parkinsons in, in fact, two distinct conditions one that begins in the intestines and moves to the brain, and one that starts in the brain and migrates to the intestines and other organs.
Until now, many people have viewed the disease as relatively homogeneous and defined it based on the classical movement disorders. But, at the same time, weve been puzzled about why there was such a big difference between patient symptoms, said Per Borghammer, Ph.D., professor of nuclear medicine and neuroscience at Aarhus University in Denmark. With this new knowledge, the different symptoms make more sense, and this is also the perspective in which future research should be viewed.
In addition to the showing the differences between the brain-first and body-first types of Parkinsons, the team also hypothesized that isolated REM sleep behavior disorder a known risk factor for developing Parkinsons could be specifically associated with body-first disease.
The team of Aarhus University researchers published their findings recently in the journal Brain.
Also Check: Can Celiac Disease Cause Parkinson’s Disease
An Overview Of The Current Clinical Evidence For Morphological Changes In The Brain Associated With Symptoms And Potential Associated Neural Mechanisms
Parkinsons disease is characteristically shown to have motor symptoms including resting tremor, rigidity, and bradykinesia but cognitive and behavioral problems in PD are more common and they have a direct effect on the quality of life.
The estimated prevalence of dementia in patients with PD ranges between 24 and 31% has conservatively been estimated to range between 24 and 31%. Cognitive function in PD patients with dementia is significantly different than that of the cortical dementia of Alzheimers disease . Patients with PDD often exhibit difficulties with executive functions, the retrieval aspects of memory, and visuospatial skills .
Patients with PDD often show a typical pattern of cognitive decline which shows characteristically a subcortical dementia that can be differentiated from AD in which cortical areas are affected early in the disease process and often include clear aphasia, apraxia, or agnosia. Dementia in PD is gradual in onset, and it is typically exhibited years after the onset of motor symptoms.
Evidence has shown widespread cortical cholinergic dysfunction to be factor of cognitive decline in PD. Adrenergic and serotonergic deficits have also been described in PD but they have been associated with behavioral rather than cognitive function. Regional cortical Lewy body formation, have also been implicated in cognitive decline in PD.
What Are The Pitfalls Of Datscan
DaTscan will appear abnormal in any disease in which there is a loss of dopamine nerve endings in the striatum. Therefore, Parkinson-plus syndromes, discussed in a prior blog, such as Progressive supranuclear palsy , Corticobasal ganglionic degeneration and Multiple system atrophy all typically demonstrate abnormal DaTscans. DaTscan therefore cannot be used to distinguish between these syndromes.
Every medical test has a false positive and a false negative rate. This means, that it is inevitable that in a certain percentage of people who have PD, the DaTscan will be read as normal and in a certain percentage of people without PD, the DaTscan will be read as abnormal. Results of any medical test that is performed, must therefore be considered within the entire clinical context.
Recommended Reading: What Does Parkinson’s Medication Do
The Role Of Magnetic Resonance Imaging For The Diagnosis Of Atypical Parkinsonism
- 1Institut du Cerveau et de la Moelle épinièreICM, INSERM U 1127, CNRS UMR 7225, Sorbonne Université, UPMC Univ Paris 06, UMRS 1127, CNRS UMR 7225, Paris, France
- 2ICM, Movement Investigations and Therapeutics Team , Paris, France
- 3ICM, Centre de NeuroImagerie de RechercheCENIR, Paris, France
- 4Service de Neuroradiologie, Hôpital Pitié-Salpêtrière, APHP, Paris, France
- 5Dynamics and Pathophysiology of Neuronal Networks Team, Center for Interdisciplinary Research in Biology, Collège de France, CNRS UMR7241/INSERM U1050, MemoLife Labex, Paris, France
- 6Department of Neurology, Avicenne University Hospital, Sorbonne Paris Nord University, Bobigny, France
- 7Département des Maladies du Système Nerveux, Hôpital Pitié-Salpêtrière, APHP, Paris, France
Sedation And Regional Anesthesia For Deep Brain Stimulation In Parkinsons Disease
Dilek Yazicioglu
1Ankara Diskapi Yildirim Beyazit Teaching and Research Hospital, Irfan Bastug Caddesi, Dskap, 06330 Ankara, Turkey
Academic Editor:
Abstract
Objective. To present the conscious sedation and the regional anesthesia technique, consisting of scalp block and superficial cervical plexus block, used in our institution for patients undergoing deep brain stimulation for the treatment of Parkinsons disease . Methods. The study included 26 consecutive patients. A standardized anesthesia protocol was used and clinical data were collected prospectively. Results. Conscious sedation and regional anesthesia were used in all cases. The dexmedetomidine loading dose was 1gkg1 and mean infusion rate was 0.26gkg1h1 . Propofol was used to facilitate regional anesthesia. Mean propofol dose was 1.68mgkg . Scalp block and superficial cervical plexus block were used for regional anesthesia. Anesthesia related complications were minor. Postoperative pain was evaluated mean visual analog scale pain scores were 0 at the postoperative 1st and 6th hours and 4 at the 12th and 24th hours. Values are mean . . Dexmedetomidine sedation along with scalp block and SCPB provides good surgical conditions and pain relief and does not interfere with neurophysiologic testing during DBS for PD. During DBS the SCPB may be beneficial for patients with osteoarthritic cervical pain. This trial is registered with Clinical Trials Identifier .
1. Introduction
Read Also: How Do You Test For Parkinson’s
Where To Get A Parkinsons Mri
Your two main choices if youre thinking about a Parkinsons MRI are a hospital and a free-standing imaging center. An imaging center offers you a comfortable environment with the highest quality equipment and technicians who are extremely experienced and focus exclusively on imaging. Imaging centers are also more affordable than hospitals.
Do you need a Parkinsons MRI? Are you a doctor who wants to schedule a Parkinsons MRI for a patient? Then, contact us today. At American Health Imaging, we focus on imaging, and we would love to help you.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinsons. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Recommended Reading: Can Parkinsons Be Passed Down
Brain Mri Tracks Parkinsons Progression
All Science News articles summarize a research study and are not an official opinion, endorsement or position of the Parkinsons Foundations.
Researchers at a Parkinsons Foundation Center of Excellence have found that a brain MRI that uses a special protocol can track changes that occur as Parkinsons disease progresses. This biomarker could be used in clinical trials, as an objective way to monitor whether the therapies being tested are effective. The study appears in the August 2017 issue of Brain.
Doctors currently diagnose PD based on a persons symptoms slowness, stiffness, tremor and balance difficulties. But these symptoms, and the rate at which they progress, differ from person to person. And there is no blood test, or biomarker, to definitively diagnose PD or objectively monitor underlying biological changes as PD progresses. Currently, a brain MRI may be ordered to rule out other conditions, but cannot diagnose PD or monitor its progression.
In earlier research, scientists led by David Vaillancourt, Ph.D., at the University of Florida in Gainesville a Parkinsons Foundation Center of Excellence, used a brain scanning technique called diffusion MRI to detect changes that happen only in the brains of people with PD. The scans showed an increase in free water water outside of brain cells in a part of the brain called the substantia nigra.
Results
What Does It Mean?
