Search Strategy And Literature Sources
We reviewed both pharmacological and non-pharmacological treatments for pain in patients with PD. We searched for studies cataloged in PubMed and the Cochrane library, to October 31, 2019. An initial search was conducted between February and June 2018. An updated search was performed in November 2019 to look for new publications. The keywords Parkinson, pain, and treatment OR management were combined with and to search within the title and abstract fields for each database. We also included relevant keyword derivatives, such as Parkinsons Disease, Parkinsons, and PD. In addition to the title and abstract fields, we searched reference sections for all included articles.
Assembling Your Care Team
Assembling a team that will provide you with physical and emotional support and adapt to your needs over time is one of the best ways to remain healthy. Parkinsons disease is complex and requires an interdisciplinary approach to care. The care team may include, but is not limited to:
- Movement disorder specialist
- Rehabilitation specialists including physical, occupational, and speech therapists
What Can We Do
It would seem to me that there are a number of very vicious circles and negative feedback loops between neck stiffness/rigidity/pain and neck immobilization and posture in PD, which not only impact on each other, but also have neurological and physiological implications much more broadly, including on nervous system, blood pressure and breathing. The principal strategy for progressive symptom reduction would therefore be to increase and maintain mobilization of the neck and to improve posture as much as possible, through daily exercises and therapies, and to address any old injuries elsewhere on the body which may be impacting on posture and hence neck strain.
Dr Farias provides a suite of daily exercises which help to reduce these type of neck problems over time, especially designed for, and tailored to the different types of, cervical dystonia. Many people around the world report that doing his exercise classes daily reduces the symptoms and pain of their neck dystonia, and can eventually even lead to a full recovery. This works through a process of neuroplasticity, which re-wires the connections between the muscles and the brain through movement therapy.
Dont Miss: Parkinsons Disease And Lupus
You May Like: How Does Parkinson’s Affect You
Parkinson’s Disease And Movement Disorders Center
Our center provides compassionate and timely treatment to patients with movement disorders, such as dystonia, ataxia, essential tremor and similar conditions. But our mission goes beyond patient care excellence. By offering educational events and support groups, we empower patients and caregivers to become better partners in their health.
Looking Out For Side Effects If Youre A Carer
If youre a carer of someone with Parkinsons, medication side effects can be difficult and tiring to cope with.
It may be that the person having side effects such as hallucinations and delusions or impulsive and compulsive behaviour does not realise they are experiencing them.
Its important to seek help from your specialist as soon as you can.
Read Also: Does Sam Waterston Have Parkinsons
Don’t Miss: When Does Parkinson Disease Start
What Are The Different Types Of Pain Experienced By People With Parkinsons
Five main types of pain are common for people with Parkinsons. Multiple types may be present simultaneously or occur at different points throughout a persons path with Parkinsons. Recognizing which kind of pain is present can help you optimize treatment, as can paying attention to what activities or times of day make your pain better or worse.
Musculoskeletal pain
Musculoskeletal pain that affects muscles, bones, tendons, ligaments, and/or nerves. The pain can be localized or generalized and can fade or intensify at different times. Existing musculoskeletal pain can be exacerbated by Parkinsons.
Neuropathic pain
Rather than being caused by a physical injury, this type of pain is caused by damage to the somatosensory nervous system or a disease affecting the somatosensory nervous system, which responds to external stimuli like touch, temperature, and vibration. It tends to be fairly consistent throughout the day and is present no matter what activity youre doing. Unlike the aching you may feel when youre doing a strenuous physical activity, neuropathic pain feels more like a tingly, crawly, uncomfortable sensation.
Dystonic pain
Dystonia, the movement disorder in which involuntary muscle contractions cause repetitive or twisting motions, is often very painful. Many people with Parkinsons experience dystonia as a motor symptom, whether its localized , in multiple nearby body parts , or all over .
Akathisia
Central pain
Contraindicated Drugs For Parkinsons Patients
More than two dozen drugs should not be taken by Parkinsons patients because they alter the brains dopamine system. Always let your neurologist know before you have surgery, so he or she can work with your medical team to keep your Parkinsons in control. View a list of drugs that Parkinsons patients should not take.
You May Like: Parkinson Disease Medications To Avoid
You May Like: Parkinson’s Disease Speech Therapy
Fluctuations Of Pain Experiences In Pd
Patterns of NMS fluctuations are heterogeneous and complex. Psychic NMS seem to fluctuate more frequently and severely than nonpsychic symptoms. A recent study of ten frequent NMS in advanced PD using VAS rating scales in motor-defined on- and off-states, as well as self-ratings at home, confirmed previous suspicions that increased pain in off-states and pain fluctuations correlate with a low health-related quality of life.40 Pain as NMS was more frequent in the off-state more precisely, it was three to four times more common during the off-state than during the on-state.
Side Effects With Levodopa
To avoid use in individuals with known allergy or hypersensitivity to Mucuna pruriens or components.
There have been some side effects of mucuna. In a study of patients with Parkinsons disease, a derivative of Mucuna pruriens caused minor adverse effects, which were mainly gastrointestinal in nature.
Isolated cases of acute toxic psychosis have been reported1, probably due to levodopa content. Therefore, as with Sinemet and Madopar, its use should be avoided in patients with psychosis or schizophrenia
Also Check: Rare Form Of Parkinsons
You May Like: What Is The Difference Between Parkinson’s And Als
How Is Pain Treated In Patients With Parkinson Disease
Pain serves as 1 of the most frequent nonmotor complaints in patients with Parkinson disease , affecting 68% to 95% of patients across all clinical stages. Published in the Journal of Parkinson Disease, researchers highlight that similar to PD, pain is complex and even has different classifications of subtypes within the disease.
While prominent, real-life pain data in PD remains scarce. Researchers sought to provide an overview on pain in PD, including classification, assessment, presentation, and the existing therapy landscape.
As researchers highlighted, todays classifications of pain in PD include musculoskeletal, radicular/neuropathic, dystonia-related, akathic discomfort/pain, and central pain. Notably, the difference in pain directly related to PD and central pain, which is attributed to objective painprocessing and pain-perception disturbance within ascending and descending pathways, was referenced. Most frequently, pain presents as musculoskeletal/nociceptive pain in PD patients, but in nearly half of the PD population, comorbid conditions, such as spine and joint arthrosis, serve as contributors.
When it comes to treating pain in PD, interventions remain a major unmet need as only approximately 50% of those with the disease receive at least some type of pain therapy. In managing pain, researchers recommend that therapy should be optimized to address dopaminergic issues, which has been shown to be effective in 30% of patients with PD.
Reference
Antipsychotic Drugs Called Neuroleptics
Drug-induced parkinsonism is due primarily to drugs that block dopamine receptors, particularly the D2 receptors . These drugs are most often the antipsychotic drugs, called neuroleptics, such as haloperidol, chlorpromazine, and trifluoperazine, but include metoclopramide, a gastrointestinal motility enhancer, and the antiemetics prochlorperazine and droperidol. In addition, medications that block synthesis of dopamine, such as alpha-methyl para-tyrosine and alpha-methyl dopa or deplete dopamine also induce parkinsonism. In these cases the pathophysiology is presumably due to diminished dopamine receptor stimulation, resulting in a pharmacologic state closely resembling Parkinson disease.
However, the atypical antipsychotics also block D2 receptors. Yet there is no apparent correlation between the degree of this blockade and the risk for inducing parkinsonism. The explanation for this is uncertain. One current hypothesis is the fast off theory, postulating that the duration of the D2 blockade, rather than the percentage of receptors blocked, determines the likelihood of parkinsonism . A competing theory is that the ratio of 5 HT-2a receptor blockade versus the dopamine D2 receptor blockade is critical because of the interplay between the serotonin and dopamine systems in the brain. An older theory relating extrapyramidal side effects to anticholinergic activity is considered untenable because the concomitant use of anticholinergics does not eliminate the problem.
Don’t Miss: How To Fix Parkinson’s Disease
Management Of Pain In Parkinsons Disease
Issue title: Special Issue: Clinical management of Parkinsons disease: Essentials and new developments
Guest editors: Bastiaan R. Bloem and Patrik Brundin
Article type: Review Article
Authors: Buhmann, Carstena * | Kassubek, Janb | Jost, Wolfgang H.c
Affiliations: Department of Neurology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany | Department of Neurology, University of Ulm, Ulm, Germany | Parkinson-Klinik Ortenau, Wolfach, Germany
Correspondence: Correspondence to: Prof. Dr. Carsten Buhmann, Department of Neurology, University Medical Center Hamburg-Eppendorf, Martinistrasse 52, 20246 Hamburg, Germany. Tel.: +49 40 7410 52771 Fax: +49 40 7410 45780 E-mail: .
Keywords: Parkinsons disease, pain, therapy, analgetics, pathophysiology, non-motor symptoms
DOI: 10.3233/JPD-202069
Journal: Journal of Parkinson’s Disease, vol. 10, no. s1, pp. S37-S48, 2020
Abstract
Opening The Medicine Box In The Mind: The Psychology Of Pain
In this 50-minute lecture, Beth Darnall, PhD explains how our experience of pain goes beyond the physical sensation of pain. It has emotional and psychological components that affect our ability to treat pain. She cites research to demonstrate that and shares 13 specific tips to reduce the experience of pain and increase treatment effectiveness. Audience questions follow the lecture.
Don’t Miss: When Was Muhammad Ali Diagnosed With Parkinson’s Disease
Acpa And Stanford Resource Guide To Chronic Pain Management
This 213-page downloadable PDF is a comprehensive, integrated guide to medical, interventional, psychological/behavioral, pharmacologic, rehabilitative, complementary and integrative, and self-help strategies in the treatment of chronic pain. It covers general information compiled from multiple sources, is updated yearly and includes imbedded web links for certain medications and treatments and relevant internet sites of interest.
This questionnaire can help identify type of pain and determine whether someone should see a pain specialist.
My Parkinson’s Story: Pain
This 10-minute video alternates between an interview with a man and and doctors. The man shares his experience with pain as a symptom of Parkinson’s disease. The doctors explain that pain is common in Parkinson’s disease, often due to rigidity or dystonia, which can be exacerbated by “off” periods. Pain caused by Parkinson’s symptoms can be relieved by Parkinson’s medications, exercise, DBS and botox injections. Pain is an invisible symptom that should be mentioned to your neurologist.
You May Like: What Specialist Treats Parkinson’s Disease
Who Should I See To Discuss My Parkinsons Pain
Your first point of contact should be your primary doctor. Whether that means your family doctor, neurologist, or Movement Disorder Specialist , start by asking them how to manage your pain. They may prescribe you one of the medications listed above, offer suggestions about altering your lifestyle, or refer you to a pain specialist.
Pain management specialists are physicians with specialized training in the field of evaluating, diagnosing, and treating pain so, speaking to one of these specialists might be helpful for you. Be sure to get a referral from your primary care doctor, though, to ensure you are visiting a physician who understands the complexity of treating Parkinsons-specific pain.
Health and wellness providers like physical therapists, acupuncturists, and massage therapists can also be valuable members of your care team. Be willing to try new things and approach alternative therapies with an open mind, as no ones path with Parkinsons pain is the same. What works for someone else may not work for you and vice versa. Consider visiting different specialists to find a treatment plan that works best for you.
Other Symptoms: Aging Or Pd
Because the biggest risk factor for developing PD is age , skeletal problems associated with aging are often experienced by people with PD. While it is not clear that PD increases the risk or even the severity of these other skeletal conditions, the problems of PD can make the symptoms of these conditions more prominent.
- Osteoarthritis, the joint damage associated with general wear and tear on the joints, is nearly universal in aging. Osteoarthritis tends to affect larger joints such as the hip and knee.
- Arthritis of the spine is also very common. This may contribute to the development of spinal stenosis, narrowing of the canal in the spine that houses the spinal cord. In severe cases, spinal stenosis causes damage to the nerves as they exit the spine or even to the spinal cord itself.
- Disorders of the fibrous discs between the bones of the spine can also cause pain, or limb numbness or weakness.
Don’t Miss: How To Help Someone With Parkinson’s Dementia
Dopaminergic Pathways For Pain Relief
Glutamate is the main excitatory neurotransmitter in the brain . Glutamatergic conduction is closely related to the sensitivity of the central nervous system, which can produce hypersensitive responses to harmful or non-harmful information. Exercise improves dopamine transmission and affects glutamate transmission and availability, thereby improving basal ganglia function .
Types Of Pain In Parkinsons
One review classified the types of PD pain as follows:
- musculoskeletal, in which the pain results from problems with the muscles , bones or joints
- dystonic, which is due to abnormal muscle contractions caused by PD or the medications used to treat it
- radicular pain or nerve pain
- central pain, which is poorly understood and thought to be due to abnormalities in the brain itself
You May Like: What Is The Best Parkinson’s Charity
Mental Status And Social Networks
As previously mentioned, depression and pain are significant clinical problems that are comorbid with PD. Marital status, as well as other social networks, interferes with these conditions.41 The patientspouse relationship, which indicates physical and emotional support, may have a mitigating effect on patient outcomes of depression prevalence and pain interference. Single PD patients seem to have greater pain interference scores than cohabiting PD patients.42
When To Start Treatment
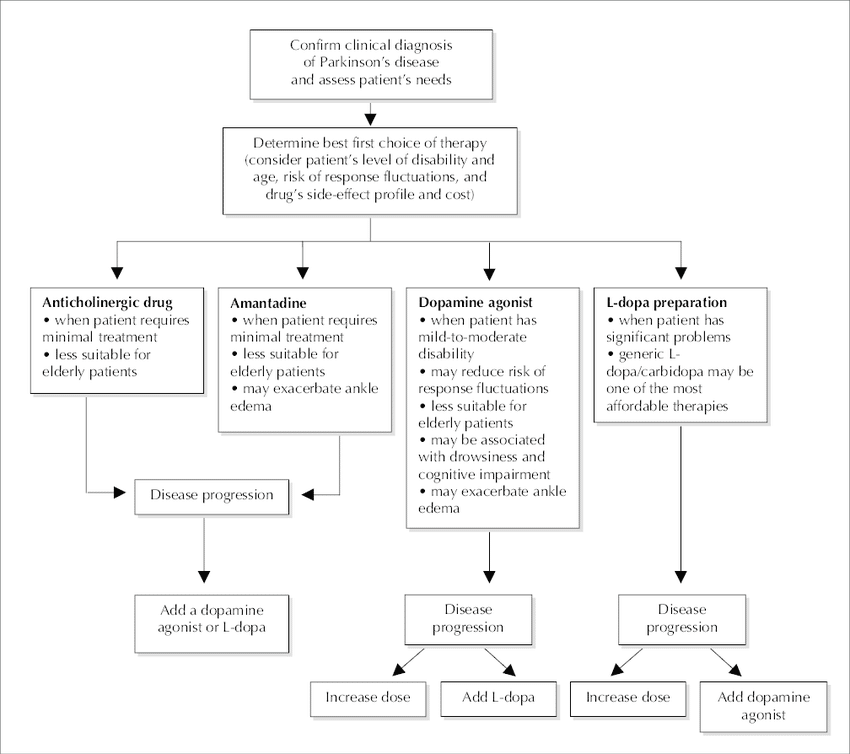
Deciding when to start drug therapy for Parkinsons disease should be individually tailored to a patients symptoms, circumstances and comorbidities. Treatment is indicated when symptoms impact on quality of life. When treatment is needed there is no evidence to support undue delay because of concerns about levodopa toxicity or the development of treatment resistance.3 The aim is to control symptoms and maintain an on state.
Some drugs with good symptomatic benefit are speculated to have a role in neuroprotection and some specialists advocate their use from the time of diagnosis.4 Delayed start trials have been used to try and differentiate symptomatic from disease-modifying effects. A recent delayed start study of rasagiline, a monoamine oxidase B inhibitor, in treatment-naïve patients with mild Parkinsons disease showed a small benefit in the low-dose treatment group. This was not seen with the 2 mg dose and a clear explanation for this has not been established.5 Further studies are needed before such treatments are considered truly disease modifying. Until a drug is unequivocally proven to slow disease progression, the time to commence treatment will remain contentious.
Dont Miss: How Much Does It Cost To Treat Parkinson Disease
Also Check: Parkinson’s Disease And Boxing Therapy
Parkinsons Patients With Severe Pain Benefit From Oxycodone
In a recent paper published in The Lancet Neurology, researchers evaluated the analgesic effect of prolonged-release oxycodone-naloxone in patients with Parkinsons disease suffering from severe and chronic pain in a pioneer Phase II clinical trial. Pain is a very common, non-motory symptom in PD patients and is one of the symptoms associated with a depressed mood and reduced quality of life. Pain in PD patients has commonly only been treated by increasing the doses of dopaminergic therapy, and so far there is no full understanding on the different types of pain these patients suffer from either a medical or patient perspective.
The multi-center, double-blind randomized placebo controlled trial, funded by Mundipharma and named PANDA, included 202 patients, 93 assigned to OXN PR and 109 to placebo. The primary endpoint was set to average 24-hour pain scores at 16 weeks in the full analysis population. Although this endpoint was not significant, results were encouraging given the statistically significant differences at week 4 , week 8 and week 12 . Also, secondary endpoints revealed OXN PR treated patients used less rescue medications and had clinically relevant improvements, relative to placebo. Moreover, researchers observed an improvement in severe musculoskeletal and severe nocturnal pain compared to placebo. However, secondary adverse effects like nausea and constipation were more frequent in patients taking OXN PR than those administered with placebo.
General Aspects Of Pain Treatment In Pd
Despite the high prevalence of pain in PD, literature data suggest that only up to a maximum of 50% of PD patients receive at least some type of pain therapy .
Still, the fundament of pain therapy should be an optimized dopaminergic treatment which can improve pain related to insufficient dopaminergic supply such as akinesia and/or rigidity , pain due to dopaminergic over-supply such as dyskinesia and/or dystonia , or central pain that is dopamine-sensitive . This concept was reported to be effective in about 30% of PD patients . A standardized levodopa test can be helpful to decide whether the pain is dopaminergic responsive or not, but any result of this short-term effect must always be interpreted with caution so that the long-term assessment of pain under dopaminergic therapy over several weeks remains essential .
A systematic review and meta-analysis including databases from January 2014 until February 2018 investigated the efficacy of a variety of novel, complimentary, and conventional treatments for pain in PD and found the greatest reduction in pain for safinamide, followed by cannabinoids and opioids, multidisciplinary team care, COMT-inhibitors, and electrical and Chinese therapies, while the weakest effects were obtained for dopaminergic agonists and miscellaneous therapies . Table 1 gives an overview of larger randomized controlled trials of antiparkinsonian drugs and opioids assessing the effect on pain in PD patients.
Table 1
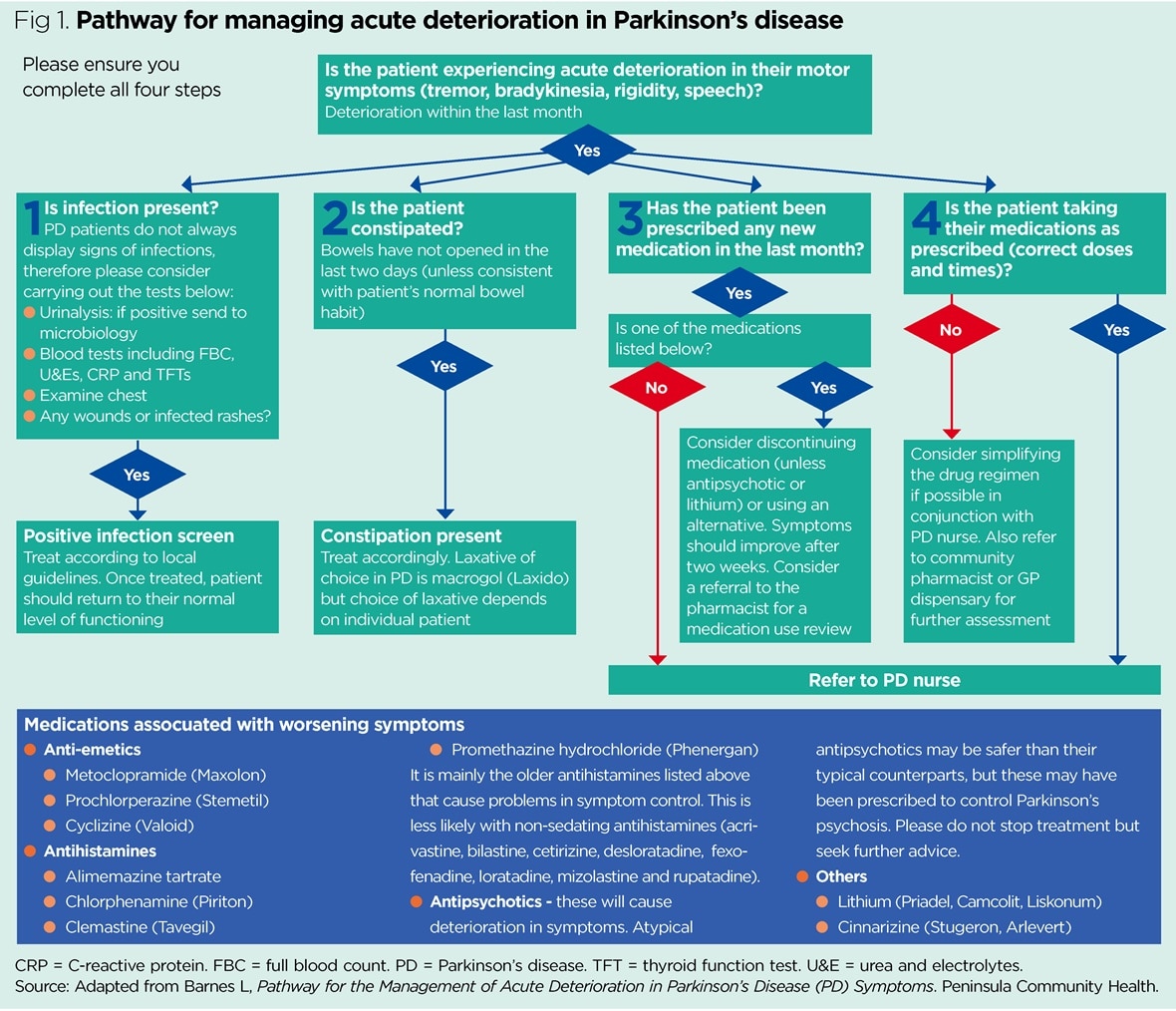
Fig.1
Don’t Miss: How Young Can Parkinson’s Start
