Management Of Incontinence In Patients With Parkinsons Disease
It is estimated that two-thirds of all patients with PD have some degree of bladder problems ranging from complete inability to empty the bladder to the more common problem of urinating too often and to the ability to make it to the bathroom in time . Common dysfunctions are bladder overactivity, causing urinary urgency, frequency, and incontinence . Getting up at night to use the bathroom is the most prevalently reported non-motor symptom with PD, reported by more than 60%. Weak voiding is also a common dysfunction. Patients may feel like they must go frequently, but when they go it may take longer than average to void. Constipation is another common issue that may arise and being constipated can affect medication absorption. Some studies suggest that 80% of people who have Parkinsons Disease report constipation.
Patients with Parkinsons Disease may also have difficulty eliminating urine. This can be caused by a sphincter that wants to close when the bladder is ready to empty or by a bladder muscle that is too weak to expel urine. This is a concern because incomplete bladder emptying can cause accumulation of urine and the growth of bacteria. The latter can result in an infection. The symptoms of difficulty eliminating urine include weak urinary stream, dribbling or leaking, and feeling that the bladder has not completely emptied.
Patient should be educated to alert their health care provider is they have any of the following signs:
Parkinsons Disease And Your Bladder
Many diagnosed with Parkinsons disease experience urinary tract issues. A Michigan Medicine urologist discusses treatment options for patients to consider.
Anne Pelletier-Cameron, M.D., often jokes to her patients that shes a female plumber of the lower urinary tract. On a more professional note, however, shes a urologist in the Michigan Medicine Department of Urology.
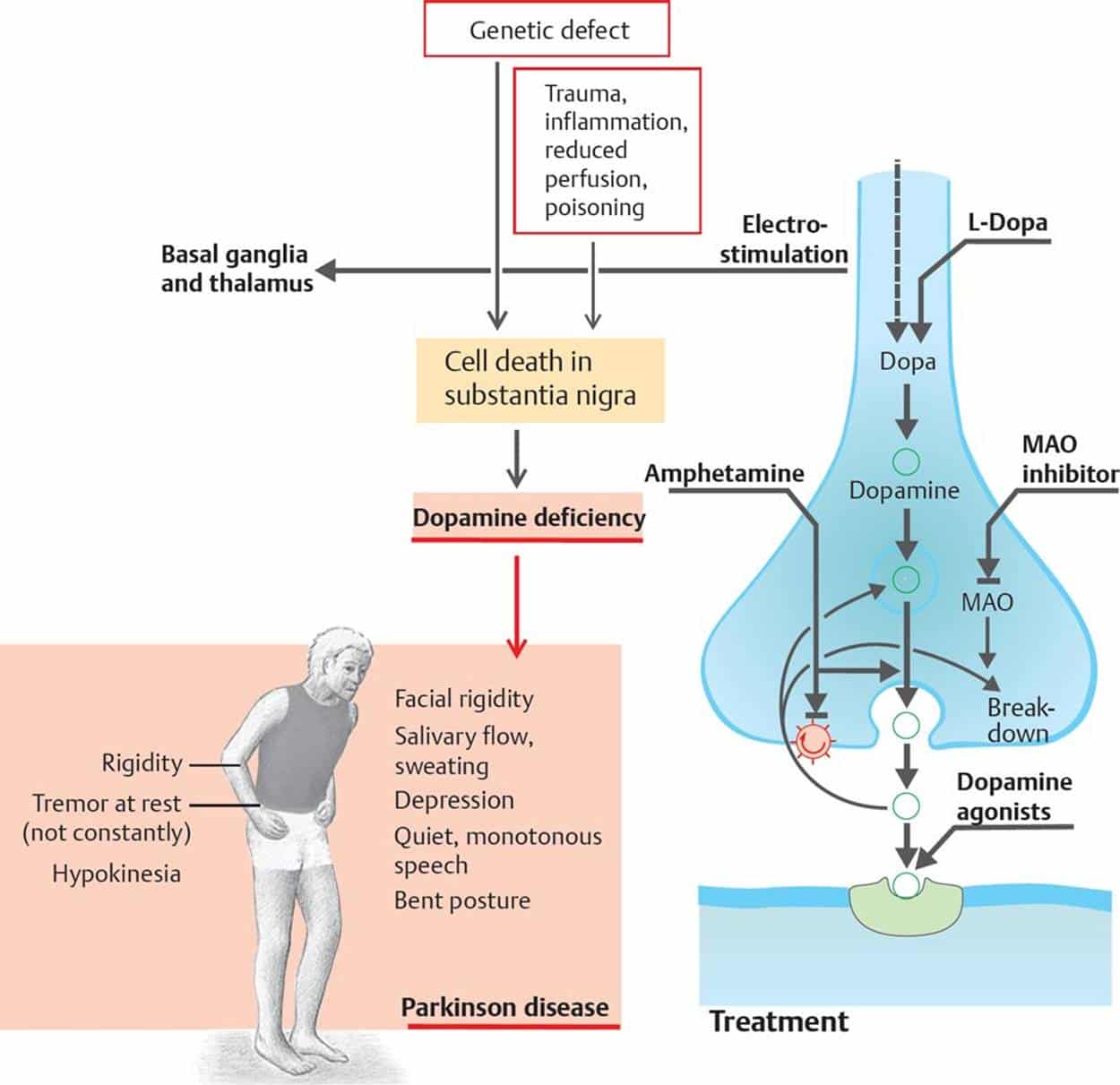
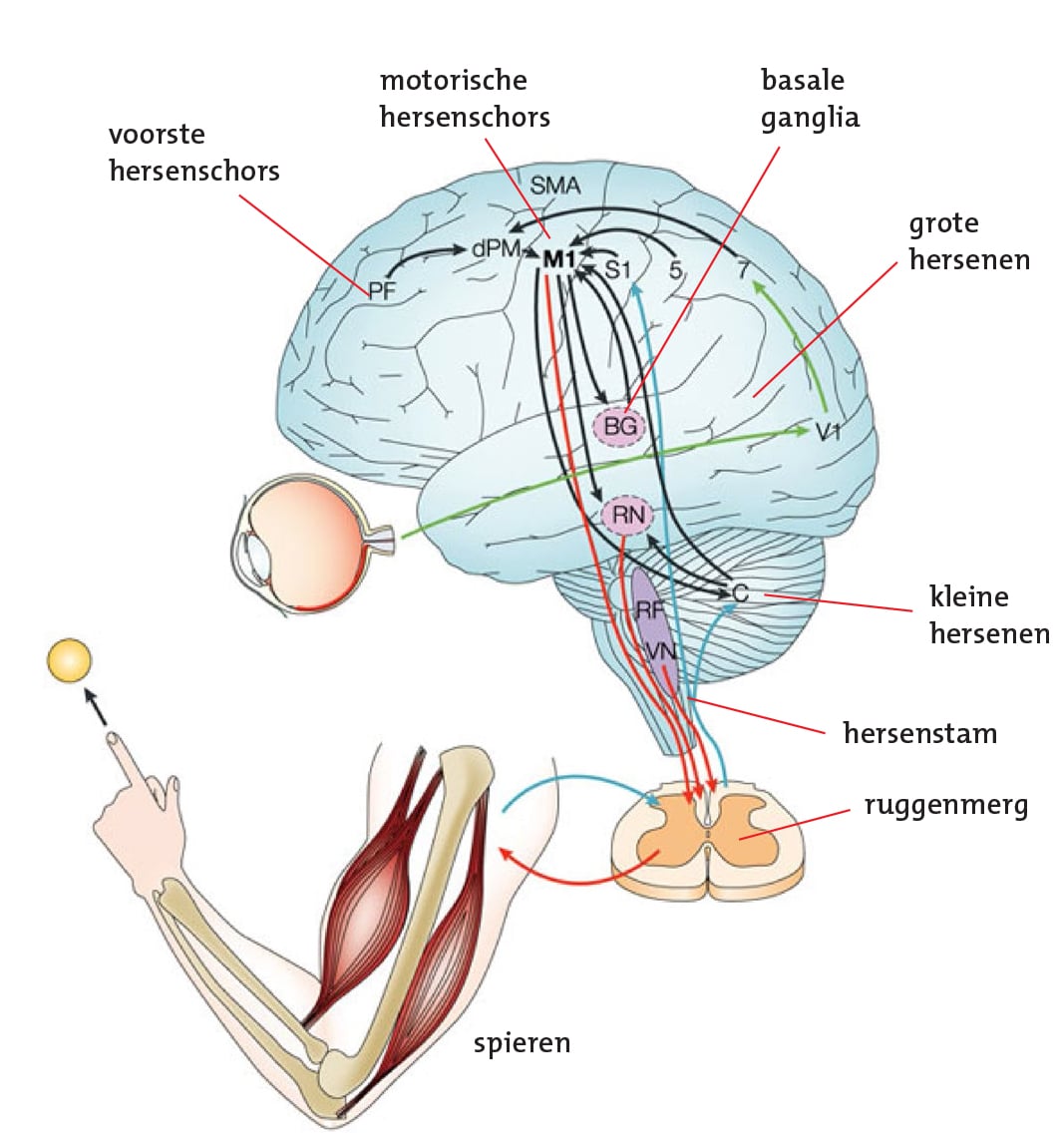
In this role, Pelletier-Cameron treats patients with a variety of lower urinary tract symptoms. Some of her patients have been diagnosed with Parkinsons disease, a progressive nervous system disorder that impacts movement. But the breakdown of nerve cells that characterize Parkinsons disease can also cause non-movement symptoms, including bladder issues.
Half of all women and 17% of men will experience urinary incontinence, or the inability to hold urine, she says, noting that for Parkinsons disease patients, those numbers escalate.
Many of my PD patients end up having other bladder problems, including issues with urgency and frequency, says Pelletier-Cameron. Nocturia, or the need to urinate many times during the night, is also common, along with difficulty in emptying the bladder.
Pelletier-Cameron says the impact of bladder symptoms cant be ignored.
Management Of Urinary Symptoms In Parkinsons Disease
Questionnaires including bother scores identify LUTS in PD with higher specificity than questionnaires without bother scores . When addressing bladder problems in patients with Parkinsonism in daily clinical work, systematic interview is needed. Addressing nocturia, urgency, frequency feeling of incomplete emptying and incontinence often provides the needed information for initiating treatment. It is important to address how these symptoms affect the daily life of the patients, as symptoms of overactive bladder may be particularly unpleasant in a patient with an akinetic rigid syndrome with postural instability.
Also Check: Antibiotic For Bladder Infection In Elderly
Don’t Miss: Parkinson’s Disease Mayo Clinic
A New Toilet Or An Alternative
If you have real difficulties getting to the toilet, it may be possible to get a grant to build a new one, perhaps downstairs. An occupational therapist can advise you on this.
Not all homes are suitable for building new toilets, so a commode might be needed. A commode is a moveable toilet that doesnt use running water. It looks like a chair, with a container underneath that can be removed and cleaned after someone has used it. They can be very discreet.
Difficulty Emptying The Bladder
- Some people with Parkinsons find it difficult to pass urine if the bladder fails to contract when required, or because the sphincter does not let urine out or a combination of the two. This is a result of reduced dopamine levels interfering with the efficiency of the bladder muscles and causing a residual amount of urine to be left in the bladder. This reduces the total amount the bladder can hold and creates a feeling of wanting to empty the bladder very often. Unfortunately, there is an increased risk of urinary infection if the bladder is not emptied completely.
- In some older people, constipation which is often associated with Parkinsons can result in faeces collecting in the rectum. This can result in difficulties in bladder emptying, which may be because of pressure on the urethra, or mediated by the nerves in the region. The bladder is then unable to empty and may continue distending, causing dribbling incontinence.
- Anticholinergic medications can also make emptying problems worse.
Read Also: Can A Person With Parkinson’s Drive
Treatment For Genitourinary Dysfunctions
Unlike the motor symptoms of PD, genitourinary dysfunctions do not respond to levodopa therapy, and other treatments must be used. There are several medications that can help manage urinary difficulties, including Detrol® , Ditropan® , Enablex® , and Vesicare® . These medications work to block or reduce overactivity in the bladder. Treatments for sexual dysfunction include counseling or talk therapy, treating erectile dysfunction with Viagra® or Cialis® , and the use of lubricants in women.1,3-5
Gastrointestinal Issues In Advanced Parkinsons Disease
Problems with motility of the gut can be a major source of difficulty throughout the disease course and can be particularly problematic in advanced PD as well. . Constipation, which can be one of the earliest symptoms of PD is a very common problem throughout the disease course. Two gut issues that tend to be particularly problematic in people with advanced PD are abdominal pain and fecal incontinence.
Recommended Reading: Solutions For Parkinson’s Disease
Treatment For Over Active Bladder In Parkinsons
Overactive bladder affects up to 27% of men and 43% of women of the global population. Now, add a neurological condition and the problem becomes more challenging. First, there is a list of medications which make the problem worse, so should be avoided. Then, a thorough evaluation and physical exam. Treatment depends on the cause, but evaluating all medications and an adjustment of dopamine medication is often necessary. If you are still having problems, five further treatment options are included.
Management Of Reduced Functional Bladder Capacity
Antimuscarinic Agents
Antimuscarinic medications are the first-line treatment for bladder storage symptoms and detrusor overactivity. Oxybutynin, tolterodine, solifenacin, and trospium chloride have beneficial effects on nocturia. If prescribed, a low dose is initially recommended with a progressive increasing dosage. Furthermore, the strict respect of the scheduled taking is important in order to reduce nonurinary anticholinergic effects.
However, their side-effect profile, which corresponds to an increasing anticholinergic burden, limits their use. The risk of urinary retention has not been specifically assessed in PD. Consequently, a repeated PVR measurement is recommended. In addition, constipation was reported not to be increased in parkinsonian patients using antimuscarinics. Of particular concern is the impact on cognitive functions in patients with PD, especially in the elderly. Anticholinergic medications can add to the anticholinergic burden of antiparkinsonian therapy and thus to the cognitive dysfunction . Drugs such as trospium chloride or tolterodine, which do not cross the bloodbrain barrier, have may be preferred. However, evidence supporting these considerations in clinical practice is limited, and caution is advised when using an antimuscarinic agent in PD.
Read Also: What Protein Causes Parkinson’s Disease
Strategies For Managing Nocturia In Pd
Despite the high prevalence of nocturia and impact on QoL, treatment options for managing this problem are currently limited and are often poorly tolerated or ineffective in PD. Guidance on nocturia treatment is limited, and most treatment options are derived from guidance around general management of urinary symptoms in neurological patients., ,
Urinary Complaints And Abdominal Ultrasound
Eighteen patients had a complaint of nocturia, , which was found to be the most common urinary complaint. This was followed by the complaints of urgency with or without urge incontinence, which was noted in 16 patients. Three patients had obstructive urinary complaints in the form of hesitancy and straining to void and retention. Three patients had mixed urinary complaints.
Ultrasound was suggestive of significant PVR in three patients. No patient was reported to be showing back pressure changes in the form of hydroureter or hydronephrosis. Out of 12 males, 1 patient was observed to be having prostate enlargement.
Also Check: Is There A Parkinson’s Gene
Bladder Problems Are A Common Non
When we asked people affected by Parkinsons what their research priorities were for improving everyday life, reducing urinary problems emerged in the top ten.
Bladder problems can have a significant impact on peoples quality of life.
Lets hear Pauls story
I was diagnosed with Parkinsons about two years ago, but I can now look back and see that Ive had symptoms for five years or so, and this includes problems with the waterworks. My problem is not an inability to go, but if I need to go, I need to go now.
It really affects me, my first thought when planning a trip is when am I going to be able to go to the toilet. My life is controlled by where my nearest toilet is. Its a very embarrassing situation to be in. My doctor has given me pills for an overactive bladder, which help a bit. But they dont make the problem go away. Although my other Parkinsons symptoms can be frustrating at times, if I could control my bladder problems it would be life changing for me.
It has taken me some time to accept that my condition is a disability and as such I can access disabled facilities. The Radar Key Scheme allows me to access over 10,000 disabled facilities across the UK and you dont need to have a blue badge to use one. The scheme has given me much more confidence. If like me you are struggling with bladder incontinence then you should consider getting yourself a Radar Key, it can be a lifesaver!
Paul, Patient and Public Involvement Volunteer
Ongoing research
Bowel Incontinence: Another Embarrassing Casualty Of Pd
Fecal Incontinence is where you lose control of your bowels. This blog post explains the primary cause of this in Parkinsons disease. Problems reaching the toilet in time because of mobility, abdominal bloating or cramping compound the problem. Dr. De León has included a check list of things to help minimize occurrences and embarrassment, even to the point of surgery, if necessary.
You May Like: Can You Drink Alcohol With Parkinson’s Disease
What Medications Should Be Avoided In Parkinsons Disease
Maxine Mann | Answered July 20, 2020
These drugs include Prochlorperazine , Promethazine , and Metoclopramide . They should be avoided. Also, drugs that deplete dopamine such as reserpine and tetrabenazine may worsen Parkinsons disease and parkinsonism and should be avoided in most cases.Sep 22, 2011
The Impact Of Nocturia
Most studies have demonstrated that nocturia has a significant negative impact on quality of life., Awakening once at night is considered to be normal by many, and the degree of bother associated with nocturia increases with the frequency of nocturia. A recent population-based study demonstrated that having two voids or more per night was associated with impaired health-related quality of life . A number of community-based studies have demonstrated that a high proportion of patients with nocturia perceive this to be a troublesome complaint. In a large study, urinary incontinence was found to be major predictors of QoL in patients with PD using the 39-item Parkinson’s Disease Questionnaire however, the question regarding nocturia was not specifically evaluated in this study.
Few studies have evaluated the bother associated with nocturia in patients with PD, and nocturia was reported to be bothersome in 50% in one questionnaire-based study. QoL has been shown to be poor in PD patients reporting nocturia. In general, LUT symptoms have an immense impact on QoL measures, early institutionalization, and health-related costs. There exists an association between nocturia and the risk for falls and hip fractures. This becomes particularly relevant to PD where patients are at risk for falls, and a prevalence of 54% in PD patients compared to 18% in age-matched healthy participants was reported in one study.
You May Like: Upper Extremity Exercises For Parkinson Disease
Problems Caused By Limited Mobility
Some people with Parkinsons might soil their underwear. This is because mobility problems can make it difficult to wipe after using the toilet. If this is the case, it might help to use wet wipes, a bidet, or an adapted bottom wiper. An occupational therapist or the Disabled Living Foundation can offer further advice.
Bowel problems are common. But you should tell your GP if there are any changes in your bowel habits, particularly if you see blood in your stool. Some problems are difficult to avoid, but there are things you can do to make them less likely to happen.
Urinary Problems In Parkinsons Disease
This 1-hour webinar is an interview with Dr. Janis Miyasaki, Dr. Jorges Juncos, and retired movement disorder specialist and young onset Parkinsons patient, Dr. Maria De Leon. They discuss the effect of Parkinsons disease on the autonomic nervous system, which regulates many body functions, including bladder control. Urinary problem diagnosis, symptom management and ongoing research on the topic wrap up the hour.
Read Also: Different Types Of Bladder Cancer
Also Check: What Is The Best Diet For Parkinson Disease
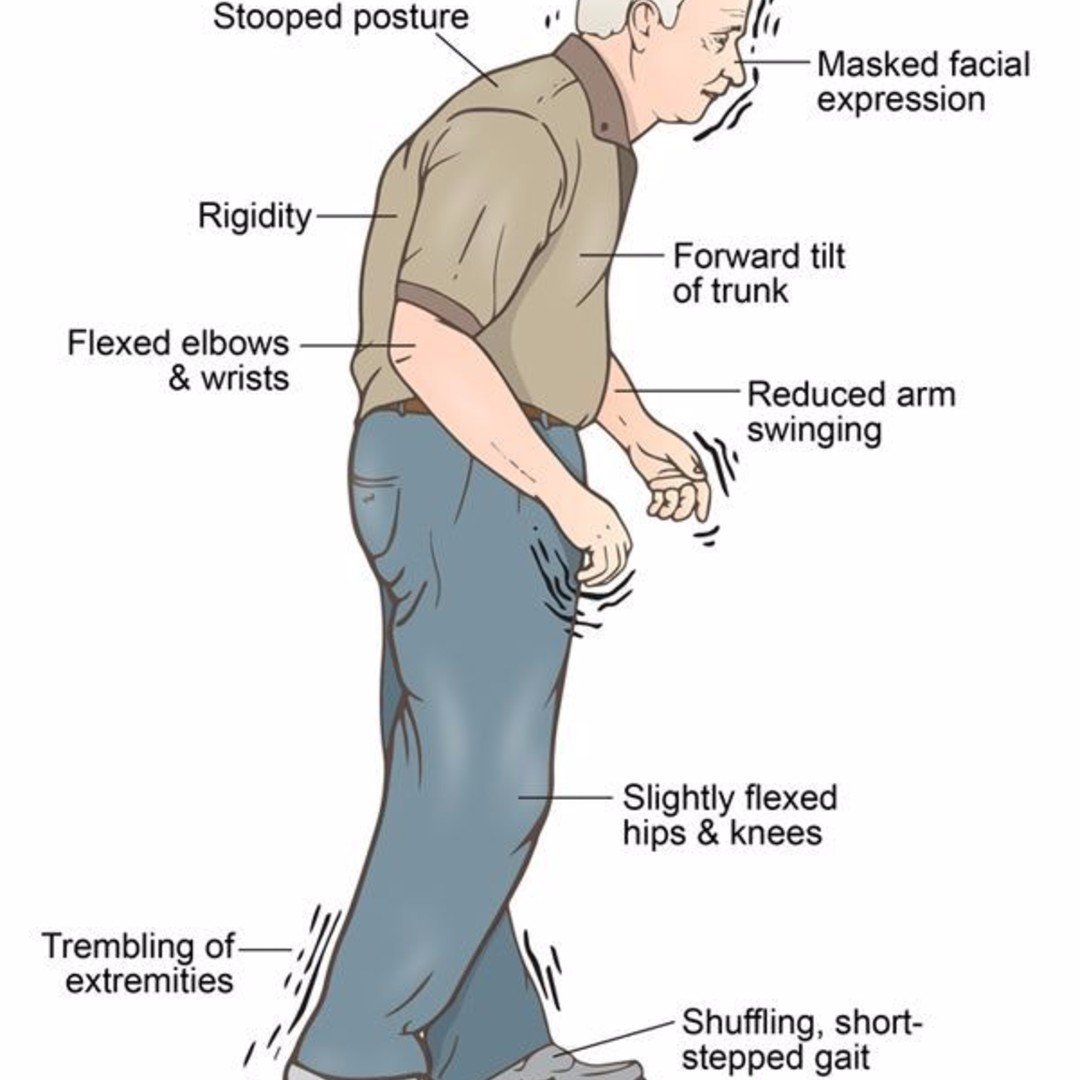
Balance Impairment And Falls In Parkinsons Disease
One of the most challenging symptoms of Parkinsons disease that fundamentally affects quality of life is balance impairment that can lead to falls.
Falls are one of the major causes of emergency room visits and hospitalizations for people with PD, so finding ways to prevent as many falls as possible is a high priority for people with PD. Thankfully there are things you can do to improve your stability and decrease the likelihood of falling, and well share some helpful tips and advice below.
Also Check: Interstitial Cystitis Or Bladder Cancer
How Is Neurogenic Bladder Diagnosed
A doctor will do an exam and may order several tests of the nervous system and the bladder to diagnose neurogenic bladder: These include:
- Urodynamic studies: These bladder function tests measure how much urine the bladder can hold, the pressure within the bladder, how well urine flows, and how well the bladder empties when it is full. Special sensors may be placed on the skin near the urethra or rectum to see if the muscles and nerves in those parts of the body are working properly.
- Cystoscopy: The doctor may perform this procedure to examine the inside of the bladder and urethra with the use of a small telescope .
Dont Miss: What Antibiotic Do You Take For A Bladder Infection
Recommended Reading: Ashwagandha And Parkinson’s Disease
Livdry Incontinence Productsdelivered Discreetly With Free Shipping
As you navigate new and progressing symptoms,it can seem overwhelming. TYE Medical offers an easy way to evaluate, compare,and purchase the incontinence supplies you need.
You can shop our online store to compare products andtake advantage of our Product Finder Tool to help make apersonalized choice. If you have questions, our friendly customer service teamis standing by to help.
You can also take advantage of discreet, free shipping on all orders!
Compliance With Ethical Standards
Amit Batla and Natalie Tayim each declare no potential conflicts of interest.
Mahreen Pakzad has been a speaker for Astellas.
Jalesh N. Panicker has received royalties from Cambridge University Press, has been involved in trials supported by FirstKind Ltd, Allergan and Ipsen and has received speaker honoraria from Wellspect, Astellas and Allergan.
Don’t Miss: Shoes For Parkinson’s Patients Australia
What Happens To Someone Who Has Urinary Incontinence
The pelvic floor consists of a hammock of muscles, ligaments, and connective tissue, which covers the bottom of the pelvic cavity and assists in supporting the abdominal and pelvic organs. The pelvic floor maintains continence of bowel and bladder and plays an important role in sexual function.
The pelvic floor muscle consists of three layers and has fast and slow-twitch fibers to assist with support and sphincter properties. The muscle is the same in women and men and both sexes benefit from maintaining good strength and tone of the pelvic floor muscle.
As we age and with certain diseases such as PD our muscles become weak and the signals do not always tell the muscles to tighten up when they need too. Add a few pounds to the belly region also and you have the perfect storm for Peezing, Peelaughing, as well as a host of other words for embarrassing moments due to urinary incontinence or urgency!
Recommended Reading: Hard To Urinate When Bladder Full
What You Can Do To Help
- Discuss bladder problems with your family doctor or neurologist, who may perform some tests to rule out urinary tract infection or other problems.
- Speak with your family doctor or neurologist about a referral to a urologist . The urologist will be able to look into any bladder symptoms and provide treatment plans.
- Be aware that bladder difficulties can be a sign of wearing off. Wearing off is where some of the symptoms of Parkinsons occur or worsen between doses of medication and are related to the level of medication becoming too low. Taking your medication on time every time helps reduce fluctuations and that will help reduce bladder difficulties.
- Managing constipation and making sure that you have regular bowel movements will also assist in minimising bladder problems.
Read Also: What Is Shuffling Gait Parkinson’s Disease
Management Of Sexual Dysfunction
Management of sexual dysfunction in patients with PD includes both behavioural and pharmacological options depending on the nature of the sexual dysfunction. Behavioural therapy may be used to treat SD, if considered as a learned maladaptive behaviour and may involve the use of psychodynamic psychotherapy and cognitive behavioural therapy . Pharmacological treatment of SD, on the other hand, requires either the reduction or elimination of drugs interfering with the sexual function or the introduction of drugs that improves sexual function . Ultimately, treatment options for SD may require multidisciplinary input from neurologists and psychologists for optimum results . Although phosphodiesterase 5 inhibitors are standard treatment option for erectile dysfunction , intracavernosal alprostadil 1.2510 g injections can be used.
The management of hypersexuality as part of an impulse control disorder includes reduction/stopping of dopamine receptor agonist and practical therapeutic strategies including psychological therapies but not limited to counselling, psychotherapy, sex, couple and behavioural therapies . Hormonal treatment specifically testosterone has been tried in PD .
