Asceneurons Innovation In Pdd And Dlb
Several symptomatic treatments addressing motoric disturbances in PD are currently available. In contrast, there is a very high unmet medical need for novel symptomatic medications to mitigate the cognitive decline in Parkinsons disease dementia patients, since available options have limited efficacy and considerable side effects. As the disease progresses, balancing the benefits of medications with their side effects becomes challenging for caregivers.
Asceneuron has generated small molecules of novel chemical classes that have the potential to deliver novel, well-tolerated and efficacious drugs to treat learning and memory deficits in dementia. Our positive allosteric modulators of the M1 muscarinic acetylcholine receptor have the potential to bring the first approved treatment for PDD to patients and a new class of molecules for the treatment of dementia in general. M1 PAMs induce a change in the shape of the receptor, enhancing binding to the neurotransmitter acetylcholine. As a result, receptor activity is potentiated so that it can still fulfill its signaling functions, critical for cognition, even in situations where acetylcholine levels are reduced as observed in Parkinsons disease dementia and other dementia in general.
Given the high unmet medical need in PDD, a symptomatic treatment for one of the more debilitating facets of PD would bring significant benefit to PD patients and their caregivers.
Diagnosis Of Parkinsons Disease
A number of disorders can cause symptoms similar to those of Parkinson’s disease. People with Parkinson’s-like symptoms that result from other causes are sometimes said to have parkinsonism. While these disorders initially may be misdiagnosed as Parkinson’s, certain medical tests, as well as response to drug treatment, may help to distinguish them from Parkinson’s. Since many other diseases have similar features but require different treatments, it is important to make an exact diagnosis as soon as possible.
There are currently no blood or laboratory tests to diagnose nongenetic cases of Parkinson’s disease. Diagnosis is based on a person’s medical history and a neurological examination. Improvement after initiating medication is another important hallmark of Parkinson’s disease.
What You Need To Know
- Lewy body dementia is a form of progressive dementia that affects a persons ability to think, reason, and process information.
- Diagnosing Lewy body dementia can be challenging an estimated 1.4 million Americans are living with the disease.
- LBD has three features that distinguish it from other forms of dementia:
- Fluctuating effects on mental functioning, particularly alertness and attention, which may resemble delirium
- Recurrent visual hallucinations
- Parkinson-like movement symptoms, such as rigidity and lack of spontaneous movement.
Lewy bodies are clumps of abnormal protein particles that, for reasons that are not fully understood, accumulate in the brain. These deposits cause a form of dementia called Lewy body dementia, or LBD which is what the late actor and comedian Robin Williams suffered from.
LBD is not the same as Parkinsons, but the two are closely related: LBD causes some or all of the motor symptoms of Parkinsons. More than 1 million people in the U.S. are affected by Lewy body dementia, according to the Lewy Body Dementia Association.
Read Also: Parkinson Disease Autosomal Dominant
Concomitant Dysfunction In Frontal And Arousal Networks Contributes To Generation Of Visual Hallucinations
Overlapping dysfunctions in a number of other cognitive networks are also likely to contribute to the generation of visual hallucinations in PDD. For example, several functional MRI studies comparing patients with Parkinsons disease with hallucinations to those without during performance of visual paradigms have demonstrated not only dysfunction in visual cortical areas in the former, but also simultaneous disruption of activity in frontal areas . The presence of hallucinations in PDD is closely associated with worsening impairments on tests of attentional control , as well as impairments on tests of inhibitory control such as the Stroop Test and Go/No-Go Task , deficits that might in part be attributable to dysfunctions in the fronto-parietal and noradrenergic networks respectively . This therefore suggests that breakdown in these frontal networks may play a contributory role in the generation of visual hallucinations in PDD, perhaps by reducing attentional and inhibitory control of perceptual errors arising from dysfunction in posterior visual cortices, allowing them to enter conscious perception as hallucinations .
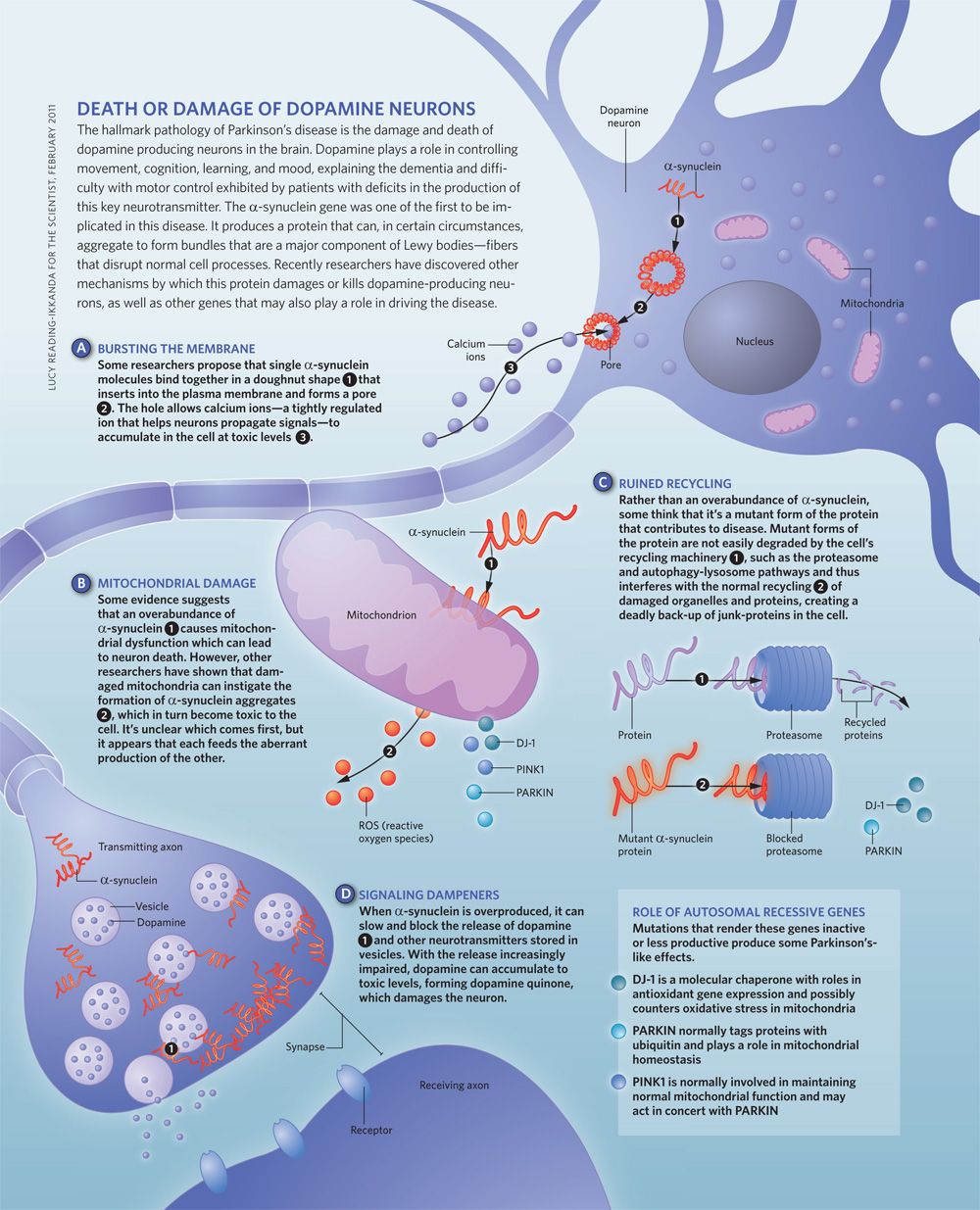
What Causes Parkinson Disease
Parkinson disease arises from decreased dopamine production in the brain. The absence of dopamine makes it hard for the brain to coordinate muscle movements. Low dopamine also contributes to mood and cognitive problems later in the course of the disease. Experts don’t know what triggers the development of Parkinson disease most of the time. Early onset Parkinson disease is often inherited and is the result of certain gene defects.
You May Like: What Color Is The Ribbon For Parkinson’s
Tremors Are Just One Of Many Symptoms That May Indicate Parkinson’s Disease
In addition to tremors, there are several other symptoms to look out for if you suspect PD. According to the Mayo Clinic, many patients experience slowed movement, rigid muscles, impaired balance, poor posture, and a decreased ability to perform unconscious movements, like swinging your arms while you walk. Additionally, PD patients often notice changes to their speech, including speaking more softly, speaking in monotone, developing a slur, or hesitating before speaking. Finally, some people with Parkinson’s find that their handwriting changesâit may become increasingly difficult to write, and your handwriting may become smaller over time.
For more health news sent directly to your inbox, .
What Is Parkinsons Disease Dementia
Parkinsons disease dementia is a brain disorder that occurs in somebut not allpeople living with Parkinsons disease. The brain cell damage caused by the disease can lead to a loss of memory and other cognitive functions such as problem solving and speed of thinking. These changes in thinking and behavior can impact your daily living, independence, and relationships.
In those who do develop Parkinsons disease dementia, there is at least one yearand usually 10 to 15 yearsbetween the Parkinsons diagnosis and the onset of dementia. According to estimates by the Alzheimers Association, 50% or more of people with Parkinsons disease eventually experience dementia, although there are a number of risk factors that impact the likelihood of developing symptoms:
- Parkinsons patients who experience hallucinations, excessive daytime sleepiness, and more severe motor control problems are at higher risk for dementia.
- Dementia is more common in people who are older at onset of Parkinsons.
- Dementia is a bigger risk factor in non-tremor predominant Parkinsons.
- Overwhelming stress, cardiovascular disease, and adverse reactions to the Parkinsons disease drug levodopa can also indicate an increased risk for developing dementia.
- Dementia is relatively rare in people who develop Parkinsons before age 50, no matter how long they have had the disease.
You May Like: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Degeneration In The Mesocortical Dopamine Network Contributes To Executive Dysfunction
However, dopamine-dependent neural circuitry underlying executive deficits in Parkinsons disease may not be limited to the fronto-striatal network alone. The mesocortical dopamine network originates in the midbrain ventral tegmental area and projects diffusely to neocortical areas, particularly prefrontal, insular and cingulate cortices . Release of dopamine from this network modulates prefrontal D2 receptors and thereby facilitates cognitive flexibility, a core feature of executive processing . Insular cortex in particular is considered to mediate such flexibility, acting as a hub to recruit other cognitive circuits such as the fronto-parietal network . In support of this, insular lesions in human patients have been shown to impair performance on tasks requiring cognitive flexibility .
What Are The Symptoms Of Parkinson Disease
Parkinson disease symptoms usually start out mild, and then progressively get much worse. The first signs are often so subtle that many people don’t seek medical attention at first. These are common symptoms of Parkinson disease:
- Tremors that affect the face and jaw, legs, arms, and hands
- Slow, stiff walking
Don’t Miss: Is Sugar Bad For Parkinson’s Disease
Clinical Features And Diagnostic Criteria Of Dlb
Table 1 Clinical overlap and dissimilarities between dementia with Lewy bodies and Parkinson disease with dementia
Supporting clinical features for the diagnosis of probable or possible DLB are repeated falls, syncopes, hyposmia, severe autonomic dysfunction, hypersomnia, hallucinations in non-visual modalities, apathy, depression, and severe sensitivity to antipsychotic agents . However, since these changes also occur in advanced PD, they cannot differentiate DLB from PDD, e.g., the prevalence of neuroleptic sensitivity does not differ significantly between them .
A diagnosis of clinically probable DLB requires two or more core clinical features to be present, with or without indicative biomarkers, or the presence of only one core clinical feature but with one or more indicative biomarkers . Although the diagnostic specificity of these criteria is high , the sensitivity can be low , improving with additional supporting features such as biomarkers . A recent meta-analysis reported a pooled sensitivity, specificity, and accuracy of 60.2% , 93.8% , and 79.7% , respectively, for the diagnostic criteria of DLB . Thus, currently, approximately 20% of DLB diagnoses are incorrect .
Diagnosis: Parkinson’s Dementia Or Dementia With Lewy Bodies
During assessment, a specialist may look at when the dementia symptoms first appeared before reaching a diagnosis of Parkinson’s dementia or dementia with Lewy bodies.
If there have been motor symptoms for at least one year before dementia symptoms occur, specialists will often give a diagnosis of Parkinson’s dementia.
If dementia symptoms occur before or at the same time as motor symptoms, specialists will usually give a diagnosis of dementia with Lewy bodies.
However, it should be noted that in some cases of dementia with Lewy bodies, no motor symptoms develop at all.
Theres no single test – diagnosis is made through several different assessments, usually starting with an appointment with your GP or Parkinson’s nurse.
Some people find it helps to go to the appointment with someone who knows them well, who can give the GP or Parkinson’s nurse information about changes they’ve noticed.
Your GP can discuss your symptoms with you and carry out a physical examination, including blood and urine tests, to rule out other potential causes of the symptoms .
Your GP may also review your medication, in case your symptoms are side effects.
If your GP thinks you have dementia, they can refer you to a specialist, such as a neurologist, psychiatrist or geriatrician.
You might be referred to a memory clinic or memory service. In some areas of the country, you can refer yourself to these services.
But if you feel you need to see the specialist again, you can ask to be referred back.
Also Check: Can Parkinson’s Run In The Family
Treatments For Parkinsons Disease Dementia And Dementia With Lewy Bodies
Treatments for DLB are similar to PDD and are aimed at symptom control. The motor symptoms of slowness, stiffness and walking difficulties can be treated with Levodopa. However, Levodopa can cause or exacerbate hallucinations, making it difficult to use it as a treatment for patients who have or are at risk of having hallucinations. Sometimes, clinicians will need to treat the hallucinations more aggressively in order for a patient to tolerate Levodopa given to help the motor symptoms. On the flipside, anti-psychotic medications to control hallucinations can worsen motor symptoms, so treating all the symptoms of LBD simultaneously can be a tricky balancing act.
What Is The Best Way To Communicate With A Person With Pdd
PD-related mood and motor changes can impact communication cognitive changes and Parkinsons disease dementia can further these difficulties.
- It is not usually helpful to try to reason or argue with someone experiencing a hallucination or delusion. Stay calm and be patient. If the person is frightened by the hallucination or delusion, try to redirect their attention to something else.
- You may find acknowledging what the person is seeing, even if you do not see it, can reduce stress.
- Speak slowly and at eye level. Communicate in simple sentences.
- Ask one question at a time and wait for an answer.
- Limit distractions. Turn off the TV or radio before asking a person with PDD to do something.
- Consider causes behind disruptive behavior: the person may be hungry, thirsty, tired, in pain, frustrated, lonely or bored.
- If the person is stuck on an idea, try agreeing with them, then changing the subject.
- Its OK to use humor to diffuse stressful situations but avoid negative humor or sarcasm these can be misunderstood.
Page reviewed by Dr. Jori Fleisher, MSCE, Assistant Professor, Department of Neurological Sciences at Rush University Medical Center, a Parkinsons Foundation Center of Excellence.
Recommended Reading: Does Parkinson’s Kill You
What Causes Parkinson’s Disease Dementia
Doctors don’t yet know the exact cause of Parkinson’s disease dementia, but they think it has to do with an accumulation of a protein called alpha-synuclein. When it builds up in the brain, it can create clumps called “Lewy bodies” in nerve cells, causing them to die.
The death of those cells usually results in the motor symptoms typically associated with Parkinson’s disease. As Parkinson’s disease progresses, those Lewy bodies may eventually damage the brain and cause problems with memory and thinking.
While many people with Parkinson’s disease experience cognitive changes, not all of them will go on to develop dementia. It’s estimated that between 50% and 80% of individuals with the disease eventually develop Parkinson’s disease dementia, usually in the later stages of the disease.
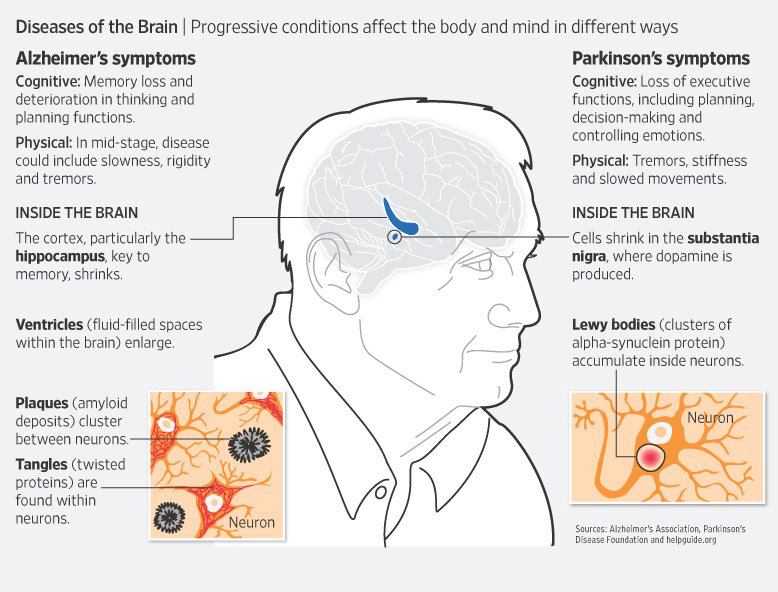
What Are The Symptoms Of These Diseases
The main symptoms of Parkinson’s disease involve motor control, such as tremor , slowness of movement, stiffness of the limbs and trunk as well as postural instability. Many patients develop a decline in thinking and reasoning known as Parkinsons disease dementia if it occurs more than one year after the initial diagnosis of Parkinsons disease. Common symptoms for PDD include decline in memory, concentration and judgment, visual hallucinations, depression, irritability and anxiety.
The central feature of Lewy body dementia is progressive cognitive decline, combined with pronounced fluctuations in alertness and attention, complex visual hallucinations and motor symptoms such as rigidity and the loss of spontaneous movement. It can easily be mistaken for Alzheimers disease or for Parkinsons disease dementia .
You May Like: What Color Represents Parkinson’s Disease
Parkinson’s Disease Dementia Surgery And Gene Therapy
- Great strides have been made in the surgical treatment of Parkinson’s disease. Several different procedures are now available, and they are successful in many patients in relieving movement symptoms. Unfortunately, surgery has no effect on cognitive symptoms. In fact, most people with dementia are not candidates for surgery.
- Gene therapy is in its infancy there are ongoing human and animal trials with various methods to insert genes into neuronal cells to reduce or stop Parkinson’s disease symptoms by causing cells to produce dopamine coded by the newly inserted genes. Early results with the treatment termed ProSavin are encouraging. However, it is not clear if such therapy could prevent or reverse Parkinson’s disease dementia.
Is There A Test To Diagnose Pd Dementia
There is no single test for PDD. The diagnosis is made clinically. If you or someone you spend time with notices cognitive changes, it is important to discuss them with your care team. If you dont have a care team in place, its important to find a specialist or physician familiar with dementia or geriatric medicine. Call the Parkinson’s Foundation Helpline 1-800-4PD-INFO for a referral.
Also Check: Can Essential Tremor Turn Into Parkinson’s
Tip : Make It A Priority To Be Socially Engaged
The more socially active you are, the more you connect face-to-face with others, the stronger your memory and cognition is likely to be. You dont need to be a social butterfly or the life of the party, but you do need to regularly connect with people who care about you.
Connecting with others is the most effective means of relieving stress which left unchecked can exacerbate symptoms of Parkinsons disease. Staying socially engaged also stimulates immune function that may slow the progress of disease. While many of us become more isolated as we get older, its never too late to meet others and develop new friendships.
Tips for meeting new people
- Volunteer
Hotlines and support
In the U.S.: Call the Helpline at 1-800-473-4636 or visit Parkinsons Foundation for resources and support. For Parkinsons Disease Dementia, call the Alzheimers Association helpline at 1-800-272-3900.
UK: Call the helpline at 0808 800 0303 or visit Parkinsons UK to find support
Australia: Call the info line at 1800 644 189 or visit Parkinsons Australia for links to state organizations that provide support and services.
Canada: Call 1 800 565-3000 for information or referrals or visit Parkinson Society of Canada for regional resources and support.
Dysfunction In Cholinergic And Noradrenergic Networks Impairs Bottom
One view of automatic orienting of attention considers it to be mediated by bottom-up or stimulus-driven signals from the NBM in the basal forebrain . This nucleus consists of 90% cholinergic neurons and its widespread projection axons provide the main cholinergic innervation to the entire cortical mantle . Selective activation of the nucleus basalis of Meynert network causes an increase in acetylcholine levels in the cortical target field, which boosts the signal-to-noise ratio for salient stimuli, thereby enhancing the strength of their neural representations . In facilitating this process the NBM effectively amplifies detection of salient stimuli by posterior regions of the fronto-parietal network and ensures their attentional significance . Animal experiments have shown that this NBM-driven cortical signal enhancement is responsible for generating event-related potentials on the EEG . These can be measured on the human EEG as negative deflections occurring 80100 ms after an unpredictable stimulus , and have long been regarded as the electrophysiological correlate of orienting of attention .
You May Like: Stages Of Parkinson Disease Life Expectancy
What Is Needed For A Parkinson’s Disease Dementia Diagnosis
There is no definitive medical test that confirms cognitive decline or dementia in Parkinson’s disease. The most accurate way to measure cognitive decline is through neuropsychological testing.
- The testing involves answering questions and performing tasks that have been carefully designed for this purpose. It is carried out by a specialist in this kind of testing.
- Neuropsychological testing addresses the individual’s appearance, mood, anxiety level, and experience of delusions or hallucinations.
- It assesses cognitive abilities such as memory, attention, orientation to time and place, use of language, and abilities to carry out various tasks and follow instructions.
- Reasoning, abstract thinking, and problem solving are tested.
- Neuropsychological testing gives a more accurate diagnosis of the problems and thus can help in treatment planning.
- The tests are repeated periodically to see how well treatment is working and check for new problems.
Imaging studies: Generally, brain scans such as CT scan and MRI are of little use in diagnosing dementia in people with Parkinson’s disease. Positron emission tomographic scan may help distinguish dementia from depression and similar conditions in Parkinson’s disease.
