What Are The Causes
The cause of Parkinson’s is largely unknown. Scientists are currently investigating the role that genetics, environmental factors, and the natural process of aging have on cell death and PD.
There are also secondary forms of PD that are caused by medications such as haloperidol , reserpine , and metoclopramide .
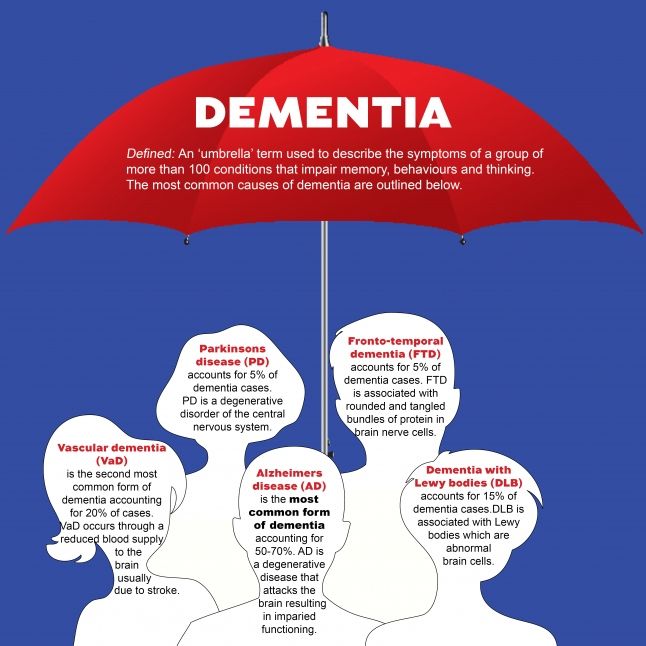
What Is Parkinson’s Disease Dementia
Parkinson’s disease is an age-related degenerative disorder of certain brain cells. It mainly affects movements of the body, but other problems, including dementia, may occur. It is not considered a hereditary disease, although a genetic link has been identified in a small number of families.
- The most common symptoms of Parkinson’s disease are tremor of the hands, arms, jaw, and face rigidity of the trunk and limbs slowness of movement and loss of balance and coordination.
- Other symptoms include shuffling, speaking difficulties, , facial masking , swallowing problems, and stooped posture.
- The symptoms worsen gradually over years.
Depression, anxiety, personality and behavior changes, sleep disturbances, and sexual problems are commonly associated with Parkinson’s disease. In many cases, Parkinson’s disease does not affect a person’s ability to think, reason, learn, or remember .
About 500,000 people in the United States have Parkinson’s disease, and about 50,000 new cases are diagnosed each year. The number of those who have some cognitive symptoms is difficult to pinpoint because accurate data are lacking for the following reasons:
Most people have the first symptoms of Parkinson’s disease after the age of 60 years, but Parkinson’s disease also affects younger people. Early-onset Parkinson’s disease strikes people around the age of 40 years, or even earlier.
What Is The Mediterranean Diet
The Mediterranean diet emphasizes the consumption of olive oil, fish, whole grains, vegetables, fruits, and legumes .
Caffeine intake and regular physical activity also have a protective role in developing Parkinson’s disease, perhaps by reducing inflammation or oxidative stress within the brain.
Interestingly, the link between caffeine intake and ALS risk remains controversial. Some studies suggest a protective role, whereas others have found no effect. The role of exercise in preventing ALS also remains unknown.
Read Also: Is Protein Bad For Parkinson’s Disease
What Are The Symptoms Of Parkinson’s Disease Dementia
Cognitive impairment in Parkinson’s disease may range from a single isolated symptom to severe dementia.
- The appearance of a single cognitive symptom does not mean that dementia will develop.
- Cognitive symptoms in Parkinson’s disease usually appear years after physical symptoms are noted.
- Cognitive symptoms early in the disease suggest dementia with Parkinsonian features, a somewhat different condition.
Cognitive symptoms in Parkinson’s disease include the following:
- Loss of decision-making ability
- Loss of short- and long-term memory
- Difficulty putting a sequence of events in the correct order
- Problems using complex language and comprehending others’ complex language
Persons with Parkinson’s disease, with or without dementia, may often respond slowly to questions and requests. They may become dependent, fearful, indecisive, and passive. As the disease progresses, many people with Parkinson’s disease may become increasingly dependent on spouses or caregivers.
Major mental disorders are common in Parkinson’s disease. Two or more of these may appear together in the same person.
The combination of depression, dementia, and Parkinson’s disease usually means a faster cognitive decline and a more severe disability. Hallucinations, delusions, agitation, and manic states can occur as adverse effects of drug treatment of Parkinson’s disease, this might complicate the diagnosis of Parkinson’s dementia.
Behaviors Seen In Parkinsons Disease Dementia
As dementia progresses, managing disorientation, confusion, agitation, and impulsivity can be a key component of care.
Some patients experience hallucinations or delusions as a complication of Parkinsons disease. These may be frightening and debilitating. Approximately 50 percent of those with the disease may experience them.
The best thing to do when giving care to someone experiencing hallucinations or delusions from Parkinsons disease dementia is to keep them calm and reduce their stress.
Take note of their symptoms and what they were doing before they exhibited signs of hallucinating and then let their doctor know.
This element of the disease can be particularly challenging for caregivers. Patients may become unable to care for themselves or be left alone.
Some ways to make caregiving easier include:
- sticking to a normal routine whenever possible
- being extra comforting after any medical procedures
- limiting distractions
- using curtains, nightlights, and clocks to help stick to a regular sleep schedule
- remembering that the behaviors are a factor of the disease and not the person
Recommended Reading: Why Do Parkinson’s Patients Keep Their Eyes Closed
Reasoning And Executive Functioning
- Mood fluctuations, including agitation and crying
- Negative reaction to questioning
- Loss of initiative and motivation
Behavioral and psychosocial symptoms are common in dementia . Responsive behaviorsa subset of these symptomsare thought to be expressions of unmet needs , responses to the environment , expressions of psychosocial needs , and responses to caregivers and other individuals.
Behavioral and psychosocial changes can lead to frustration and misunderstanding between the individual with dementia and his or her caregiver. Since these reactions are often forms of communication, it is important for caregivers to consider why the behavior is occurring and to explore ways to facilitate better communication .
See Behaviors: How To Respond When Dementia Causes Unpredictable Behaviors from the Alzheimer’s Association for more information.
Concomitant Dysfunction In Frontal And Arousal Networks Contributes To Generation Of Visual Hallucinations
Overlapping dysfunctions in a number of other cognitive networks are also likely to contribute to the generation of visual hallucinations in PDD. For example, several functional MRI studies comparing patients with Parkinsons disease with hallucinations to those without during performance of visual paradigms have demonstrated not only dysfunction in visual cortical areas in the former, but also simultaneous disruption of activity in frontal areas . The presence of hallucinations in PDD is closely associated with worsening impairments on tests of attentional control , as well as impairments on tests of inhibitory control such as the Stroop Test and Go/No-Go Task , deficits that might in part be attributable to dysfunctions in the fronto-parietal and noradrenergic networks respectively . This therefore suggests that breakdown in these frontal networks may play a contributory role in the generation of visual hallucinations in PDD, perhaps by reducing attentional and inhibitory control of perceptual errors arising from dysfunction in posterior visual cortices, allowing them to enter conscious perception as hallucinations .
You May Like: Does Parkinson Cause Eye Problems
Tissue Changes Reflecting Poorer Cognition
We showed that cognition assessed with the MoCA correlated with magnetic susceptibility in hippocampus and thalami, as well as ventromedial prefrontal cortices, basal forebrain and rostral caudate nucleus. Previous studies using conventional structural measures report varying patterns of grey matter atrophy in patients with early cognitive change in PD with several showing no atrophy changes. Hippocampal atrophy is reported in cross-sectional studies in PD, and is the most consistently abnormal region in longitudinal structural MRI. Thalamic changes are also linked with cognition in PD. However, a significant relationship between MoCA and grey matter volume has not been shown in PD.
We also found QSM increases with lower MoCA scores in the caudate nucleus. This is consistent with findings in other modalities functional MRI caudate activation is reduced during memory tasks in PD-MCI and cognitive decline in PD is linked to lower caudate uptake in dopamine transporter single-photon emission computed tomography and positron emission tomography imaging. We found QSM increases in basal forebrain with lower MoCA scores, although not in the substantia innominata . The substantia innominata is the major source of cholinergic innervation to the cerebral cortex and shows post-mortem cell depletion and Lewy-related pathology in Parkinsons dementia. The lack of covariance here could suggest this is a later event in Parkinsons dementia.
Parkinsons And Lewy Body Disease
Lewy body disease occurs when there is an abnormal build-up of a protein called alphasynuclein in the brain. Depending on where the proteins accumulate, Lewy body disease can lead to impairments in movement, thinking and behaviour.
Lewy body disease includes three overlapping disorders:
- Dementia with Lewy bodies
- Parkinsons disease dementia
This overlap results in the disease being called a spectrum disease.
In people with Parkinsons a large number of Lewy bodies appear in an area of the brain known as the substantia nigra. This area of the brain is responsible for movement, so the Lewy bodies are likely to cause impairments in movement.
Some people may go on to develop dementia with Lewy bodies. In this form of the disease, the clumps of protein occur in the cortex . This part of the brain is responsible for many cognitive processes, so the Lewy bodies are likely to result in cognitive impairments like those described under the heading above. It can result in symptoms similar to those seen in Alzheimers.
Recommended Reading: What Causes Shaking In Parkinsons Disease
Recommended Reading: Parkinson’s Breakthrough August 2021
Complementary And Alternative Therapies
DO NOT try to treat Parkinson disease with alternative therapies alone. Used with conventional medications, complementary and alternative therapies may help provide some relief of symptoms and slow progression of the disease. Some CAM therapies may interfere with certain medications, so work with your physician to find the safest, most effective CAM therapies for you.
Roles And Responsibilities Of Speech
Speech-language pathologists play a central role in the screening, assessment, diagnosis, and treatment of persons with dementia. The professional roles and activities in speech-language pathology include clinical/educational services prevention and advocacy and education, administration, and research. See ASHA’s Scope of Practice in Speech-Language Pathology .
Appropriate roles for SLPs include the following:
As indicated in the Code of Ethics , SLPs who serve this population should be specifically educated and appropriately trained to do so. Given the relationship between cognition and communication, practitioners who serve individuals with dementia require knowledge and skills in both areas, including specific knowledge of cognitive-communication disorders associated with dementia, to fulfill the aforementioned roles.
Most of the common dementia-associated diseases are progressive in nature, and SLPs have an ethical responsibility to provide appropriate services that will benefit the individual and maximize cognitive-communication functioning at all stages of the disease process.
Interprofessional Collaboration
Also Check: Is Walking Good For Parkinson’s Disease
Preventing And Delaying Cognitive Change
To overcome the cognitive changes linked to Parkinsons, it is recommended that you keep as active and stimulated as possible physically, mentally and socially. It is important to stimulate all the different parts of the brain. Some useful tips include:
- Undertake regular exercise
You May Like: Parkinsons And Swollen Feet And Ankles
How Is Parkinsons Disease Treated
There is no cure for Parkinsons disease. However, medications and other treatments can help relieve some of your symptoms. Exercise can help your Parkinsons symptoms significantly. In addition, physical therapy, occupational therapy and speech-language therapy can help with walking and balance problems, eating and swallowing challenges and speech problems. Surgery is an option for some patients.
Also Check: Adaptive Clothing For Parkinson’s Patients
Experiment C: Effect Of An Acute Dopaminomimetic Challenge
When comparing the ON state with the OFF state in levodopa-treated patients, we found only a slight modulatory effect of levodopa administration on spectral power. Changes were limited to decreases of relative power in right frontal theta , left occipital beta and left temporal gamma , and an increase in right parietal gamma power after intake of dopaminomimetics.
Diagnosis: Parkinsons Dementia Or Dementia With Lewy Bodies
During assessment, a specialist may look at when the dementia symptoms first appeared before reaching a diagnosis of Parkinsons dementia or dementia with Lewy bodies.
If there have been motor symptoms for at least one year before dementia symptoms occur, specialists will often give a diagnosis of Parkinsons dementia.
If dementia symptoms occur before or at the same time as motor symptoms, specialists will usually give a diagnosis of dementia with Lewy bodies.
However, it should be noted that in some cases of dementia with Lewy bodies, no motor symptoms develop at all.
Theres no single test diagnosis is made through several different assessments, usually starting with an appointment with your GP or Parkinsons nurse.
Some people find it helps to go to the appointment with someone who knows them well, who can give the GP or Parkinsons nurse information about changes theyve noticed.
Your GP can discuss your symptoms with you and carry out a physical examination, including blood and urine tests, to rule out other potential causes of the symptoms .
Your GP may also review your medication, in case your symptoms are side effects.
If your GP thinks you have dementia, they can refer you to a specialist, such as a neurologist, psychiatrist or geriatrician.
You might be referred to a memory clinic or memory service. In some areas of the country, you can refer yourself to these services.
But if you feel you need to see the specialist again, you can ask to be referred back.
Read Also: What Is The Difference Between Parkinson’s And Ms
Living With Parkinson Disease
These measures can help you live well with Parkinson disease:
- An exercise routine can help keep muscles flexible and mobile. Exercise also releases natural brain chemicals that can improve emotional well-being.
- High protein meals can benefit your brain chemistry
- Physical, occupational, and speech therapy can help your ability to care for yourself and communicate with others
- If you or your family has questions about Parkinson disease, want information about treatment, or need to find support, you can contact the American Parkinson Disease Association.
What Are The Symptoms Of Parkinson Disease
Parkinson disease symptoms usually start out mild, and then progressively get much worse. The first signs are often so subtle that many people don’t seek medical attention at first. These are common symptoms of Parkinson disease:
- Tremors that affect the face and jaw, legs, arms, and hands
- Slow, stiff walking
Recommended Reading: Can Dogs Have Parkinson’s Disease
Frontotemporal Dementia With Parkinsonism
One form of familial FTD, also known as frontotemporal dementia with Parkinsonism-17 , is caused by genetic changes in the gene for tau protein, located on chromosome 17. No other risk factors for this condition are known.
FTDP-17 is rare and accounts for only three per cent of all cases of dementia. Symptoms progressively get worse over time and usually appear between the ages of 40 and 60. The condition affects both thinking and behavioural skills and movements such as rigidity, lack of facial expression and problems with balance .
It can be distressing to be told that you have a genetic disorder or are at risk of having one. Genetic counselling provides the person and their family with information about a genetic disorder and its likely impact on their lives. This can assist a person with FTDP-17 to make informed medical and personal decisions about how to manage their condition and the challenges it presents to their health and wellbeing. Prenatal genetic counselling is also available for parents to help them decide about a pregnancy that may be at risk of FTDP-17.
How Can We Manage Hallucinations
It may not be necessary to treat all hallucinations of a person with PDD. Hallucinations are often harmless, and it is okay to allow them to happen, as long as they are not disruptive or upsetting to the person or surroundings. Sometimes, recognizing the hallucination and then switching the topic might be an efficient way of handling frustrations that occur because of a hallucination. If hallucinations need medical treatment, your provider may be able to discuss and suggest some options. However, many of the medications used to treat hallucinations may make movement symptoms worse.
You May Like: What Does Parkinson Do To Your Brain
Hereditary Forms Of Parkinsons Disease And Their Clinical Features
A small but significant number of PD patients have a family history compatible with Mendelian autosomal inheritance , either dominant or recessive. Many of these are classified as young-onset or juvenile-onset PD . A number of levodopa-responsive parkinsonian syndromes have been described and linked to a specific locus or gene in the last few years, and some of them have been classified as PARK syndromes . Some of these denote true PD, whereas others represent more complex phenotypes and dissimilar diseases. Only the former group will be briefly approached here, as the clinical phenotype may be a useful pointer for the diagnosis in daily practice, guiding subsequent molecular testing. For more details on the genetics of PD please refer to .
Autosomal-dominant PD:
PARK1/PARK4 : Mean age at onset of symptoms is in the 30s or 40s . Progression appears to be faster than in sporadic PD and dementia is a frequent finding at times the clinical picture resembles DLB, but mean age at onset is much lower than in sporadic cases . PARK1 and PARK4 are attributable to SNCA mutations and duplications/triplications, respectively.
PARK3 : Researchers described a group of families with parkinsonism closely resembling that of sporadic PD, including age of onset the locus has been mapped to 2p13. Penetrance was estimated to be below 40% . It has not been clearly defined whether this represents a disease susceptibility locus or a true Mendelian form of PD.
Autosomal recessive PD:
Traditional Chinese Medicine And Acupuncture
Traditional Chinese Medicine views disease as caused by internal imbalances. It has historically been used to treat Parkinson disease with acupuncture and individually prepared herbal remedies. One study showed that acupuncture improved symptoms in a small group of people with Parkinson disease. People with Parkinson disease may also find that acupuncture helps them sleep better. If you consult a TCM practitioner, make sure your doctor is aware of any suggested treatment.
Recommended Reading: Does Emmylou Harris Have Parkinson’s
What Are The Symptoms Of End
Stage four for Parkinsons disease is often called advanced Parkinsons disease because people in this stage experience severe and incapacitating symptoms. This is when medication doesnt help as much and serious disabilities set in.
Theres an increased severity in:
- How you speak a softer voice that trails off.
- Falling and trouble with balance and coordination.
- Freezing a sudden, but temporary inability to move, when you start to walk or change direction.
- Moving without assistance or a wheelchair.
- Other symptoms such as constipation, depression, loss of smell, low blood pressure when going to stand up, pain, and sleep issues.
Many times someone with advanced PD cant live on their own and needs help with daily tasks.
Stage five is the final stage of Parkinsons, and assistance will be needed in all areas of daily life as motor skills are seriously impaired. You may:
- Experience stiffness in your legs. It may make it impossible to walk or stand without help.
- Need a wheelchair at all times or are bedridden.
- Need round-the-clock nursing care for all activities.
- Experience hallucinations and delusions.
As Parkinsons disease progresses into these advanced stages, its symptoms can often become increasingly difficult to manage. Whether you or your loved one with end-stage Parkinsons lives at home, in an assisted living facility or a nursing home, hospice services can optimize your quality of life and that of your family members as well.
