Dementia With Lewy Bodies
- Dementia with Lewy bodies is a progressive, neurodegenerative disorder in which abnormal deposits of a protein called alpha-synuclein build up in multiple areas of the brain.
- DLB first causes progressive problems with memory and fluctuations in thinking, as well as hallucinations. These symptoms are joined later in the course of the disease by parkinsonism with slowness, stiffness and other symptoms similar to PD.
- While the same abnormal protein is found in the brains of those with PD, when individuals with PD develop memory and thinking problems it tends to occur later in the course of their disease.
- There are no specific treatments for DLB. Treatment focuses on symptoms.
Als As A Disease Of Rna Quality Control
Although ALS research was dominated for many years by the apparent connection between SOD1 misfolding and FALS, the recent discovery of two additional genes, mutations which appear to be associated with both familial disease and increased risk for sporadic ALS, has caused a rethinking of the molecular etiology of most forms of the disorder. In contrast to the antioxidant enzymatic activity of SOD1 and its tendency to form pathological aggregates, these two new genes, TDP-43 and FUS/TLS, encode primarily nuclear proteins that function in RNA biology. As we shall see, they not only raise the possibility that ALS is an RNA-based disease, they also suggest that a broader view of the concept of proteostasis may be valuable for developing new approaches to its treatment.
Unprecedented Method Predicts Als Parkinson’s Disease
- Date:
- Mayo Clinic
- Summary:
- A new Mayo Clinic study details an unprecedented method to predict brain aging disorders such as amyotrophic lateral sclerosis and Parkinson’s disease. Investigators studied common variations within axon guidance pathway genes and identified several gene variations that collectively predicted people who are at a high risk for ALS .
A new Mayo Clinic study details an unprecedented method to predict brain aging disorders such as amyotrophic lateral sclerosis and Parkinson’s disease. Investigators studied common variations within axon guidance pathway genes and identified several gene variations that collectively predicted people who are at a high risk for ALS . They also identified several gene variations that collectively predicted people at a high risk for Parkinson’s disease .
The probability that the findings were by chance was extremely small . The axon guidance pathway consists of a complex array of chemical signals that wires the brain during fetal development and maintains and repairs brain wiring throughout life.
About the Study
The investigators obtained these results by analyzing publicly available datasets of whole-genome variations in people with ALS, Parkinson’s disease and those who did not have neurological disorders. The datasets were released recently by the Coriell Institute and the National Institutes of Health. The investigators developed and applied to the data a genomic pathways approach.
About ALS
About Parkinson’s disease
Also Check: Can Parkinson’s Change Your Personality
Alterations In Other Monoamine Neurotransmitter Systems
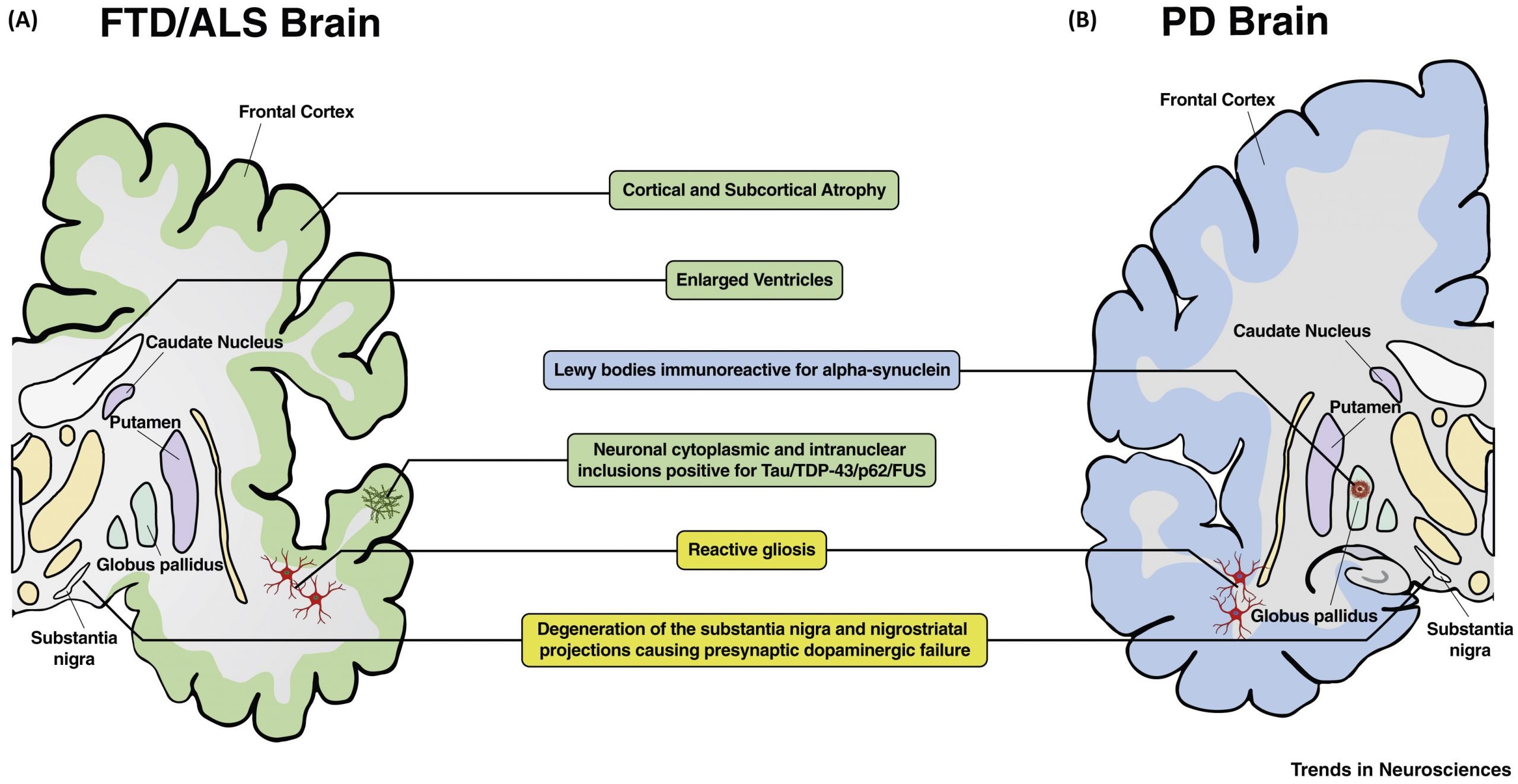
NA levels have been previously reported to be significantly increased in the cervical, thoracic and lumbar spinal cord of ALS patients compared to controls , with highest concentrations measured in ventral and intermediate gray matter. In CSF, a similar increase has been noted . Independently of 5-HT, NA increases the excitability of motor neurons to glutamate . Bertel et al. further discussed that in all probability, it is unlikely that the noradrenergic changes were due to the effect of tissue shrinkagesince concentrations were expressed in ng/g wet weighed tissuebut rather a consequence of denser noradrenergic innervation, such as from sprouting of noradrenergic fibers into affected areas. In PD, the noradrenergic dysfunction has been investigated in more detail. In summary, -synuclein depositions in the locus coeruleus , the brain’s main source of NA, have been evidenced to precede that of the SN . Consequently, neuronal loss in this noradrenergic nucleus and the accompanying noradrenergic deficiency both on the central and peripheral level have been related to various motor and non-motor symptoms, including the progression to dementia .
Introduction: Neurologic Disorders Of Movement
More than two million Americans are believed to suffer from some form of neurodegenerative movement disorder, the total cost of which is estimated to exceed $10 billion annually. Because no society on earth is spared the effects of these crippling diseases, the figures for other countries are similar, adjusted for population differences. The neurodegenerative diseases Parkinsons disease and amyotrophic lateral sclerosis are the most important of the movement disorders from a proteostasis perspective. ALS is often classified separately, as a motor neuron disease, but there are a number of reasons for considering them together, of which perhaps the most important is that the two sometimes present together, as in the Parkinsonism-dementia complex of Guam . This movement disorder occurs among the Chamorro populations of Guam and the Mariana Islands and is frequently accompanied by a motor neuron disease resembling ALS. The course of the disease is rapid, with death typically occurring within 5 years .
In the following sections, we will review the evidence that links dysfunction in the proteostasis of certain proteins to the pathology of ALS and PD. Recent data support the notion that at least most forms of Parkinsons disease may be amenable to therapeutic strategies aimed at proteostasis of -synuclein or proteins called parkin or LRRK2, while the situation with ALS is still far from clear.
Also Check: Parkinson’s And Dementia Life Expectancy
Movement Disorders Similar To Parkinsons
Conditions causing excess movement or decreased movement that are sometimes associated with Parkinson’s disease-like symptoms include:
What Movement Disorder Could I Have?
When making a Parkinson’s diagnosis, your doctor will review your medical history and symptoms, perform a careful neurological exam, and, if necessary, carry out further tests to rule out other movement disorders.
Your symptoms may be caused by a movement disorder other than Parkinson’s disease if:
- You display Parkinson’s disease symptoms and features that are characteristic of an additional movement disorder.
- The results of a brain imaging study or laboratory test, such as a blood test, confirm the presence of another movement disorder.
- Your symptoms do not respond to Parkinson’s disease medication.
Because movement disorders are not all treated the same way, it is important to get a proper diagnosis as early as possible so you can formulate the right treatment plan with your doctor.
Parkinsons Disease Vs Als Differences In Symptoms Causes And Treatment
Written byDevon AndrePublished onJuly 25, 2016
Parkinsons disease and ALS can cause difficulties in movement and are both known to be progressive neurological diseases.
ALS is part of a cluster of disorders known as motor neuron diseases that involve gradual degeneration and death of motor neurons. In a healthy individual, messages from motor neurons in the brain are transmitted to the motor neurons in the spinal cord and sent to the particular muscles. In ALS, this communication degenerates and cells begin to die. As a result, the message that is transmitted is incomplete. Unable to function, the muscles begin to weaken and waste away over time. Eventually, communication from the brain to muscles is lost completely.
In its early stage, ALS also known as Lou Gehrigs disease may appear as Parkinsons disease, which is also a neurological disease similar to ALS. Here we will outline the causes, symptoms, and treatment options for both ALS and Parkinsons disease to help you understand the differences between the two.
Read Also: What Happens If You Stop Taking Parkinson’s Medication
Treatment Management And What To Expect
There is no cure for ALS or FTD. Riluzole, the first drug approved for use in the treatment of ALS, has been shown to slow the progression of ALS for some patients and increase survival. Rasagiline developed for Parkinsons disease, is a monoamine oxidase inhibitor but demonstrates neuroprotective action. It has been used to treat ALS and, in a recent randomized controlled study, appears to increase survival. Other medications may help relieve the symptoms of muscle cramping and spasticity. At present, there are no approved medicines for FTD. Symptomatic treatment has been attempted with medications developed for other disorders, but have had limited success in frontotemporal degeneration disorders.
Patients with this diagnosis usually experience a rapid decline in both physical and cognitive abilities. The course of ALS with frontotemporal degeneration may run as quickly as 2 to 3 years, as opposed to the 5-to-10-year course more commonly seen for other forms of FTD.
Physical therapy, including stretching exercises and low-impact exercise can help relieve muscle symptoms. Devices such as ramps, braces, walkers, and wheelchairs can help patients conserve energy and remain mobile. Speech therapy can help a patient develop strategies to speak more clearly. Over time, alternate means of communication, such as speech synthesizers, may be of use.
The Impact Of Disease
The clinical mutations in Parkin associated with disease span from genomic deletions to premature truncations and subtle missense mutations in the coding sequence. For this reason, it has been widely accepted that the pathogenicity of these PARK2 mutations derives from a critical loss-of-function. Despite the predicted loss of E3 ligase activity of these parkin mutants, biochemical evidence of parkin E3 ligase activity and the impact of parkin deficiency has been notoriously difficult to establish. Although numerous putative substrates have been reported, many have failed to withstand independent confirmation. The lack of well-founded substrates has also made it difficult to examine the degree to which each mutation alters activity, precluding an analysis of the correlation between the biochemical impact of a given parkin mutation and the severity of the resultant disease in patients. Nonetheless, there have been many valuable observations made regarding the novel PD-associated parkin variants.
Don’t Miss: Parkinson Disease Dementia Mortality
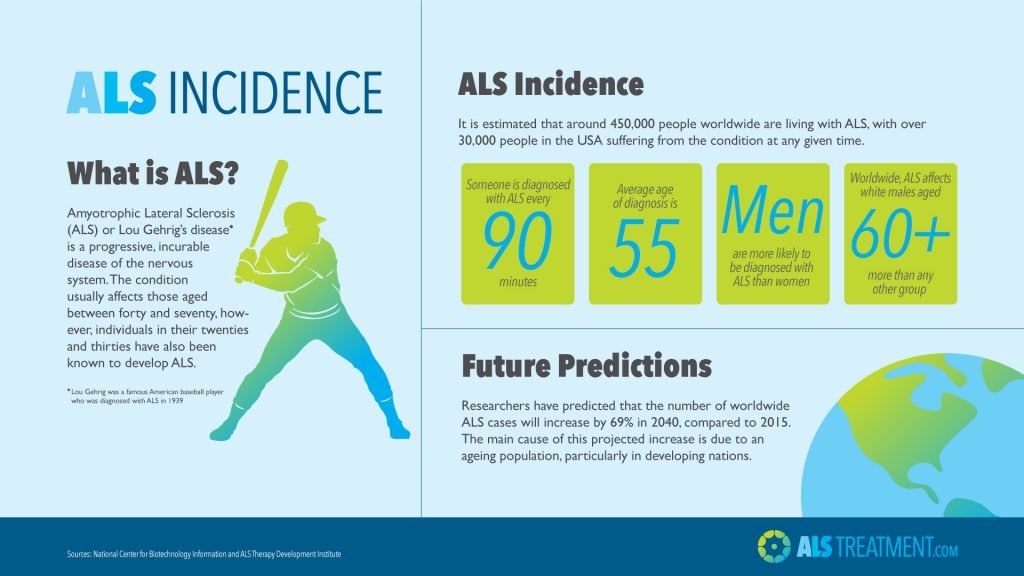
Onset Of Als And Parkinsons
There are several different variants of ALS but it generally affects people between the age of 40 and 70. Juvenile onset ALS, however, can start in childhood or typically before the age of 25, although this form of ALS is particularly rare. The onset of ALS is estimated to be 20% more common in men compared with women and in 10% of cases there is likely to be a genetic component.
Parkinsons disease is usually diagnosed in people over the age of 60, though a small percentage exhibit the symptoms before the age of 50.
Once again, men are more likely to develop Parkinsons than women.
Iqoro Acts On The Entire Swallowing Process
Research shows that IQoro acts on, and regenerates, the entire swallowing process. It stimulates the sensory nerves in the mouth, and by doing this, reaches the brains control system for the swallowing process, which is closely linked to the control systems for other bodily functions, including breathing, the ability to form sounds , facial expression, postural control , stomach and intestine functions, and more. This explains why exercising with IQoro can have a positive effect on so many different bodily functions.
It is not scientifically proven that IQoro has an effect on MS, Parkinsons or ALS sufferers. However, it is highly credible that IQoro can work as a complement, because the majority of research supporting use of the device has been carried out on stroke patients who are also, of course, suffering from a neurological disease.
As well as this, there is clinical experience of treatment of people with the above conditions and over 20 years of research.
Read Also: Can Parkinson’s Run In The Family
What Is The Life Expectancy For Ms Vs Als
In general, the prognosis for MS is much better than for ALS. People with MS may have a lifespan that is relatively normal, but is about six or seven years shorter than in those without the disease. Depending upon the response to treatment and the presence of complications, the prognosis for MS patients may range from good to poor. In contrast, the life expectancy of a person with ALS is only about 2 to 5 years after the time of diagnosis, although about 20% may live somewhat longer than five years. ALS progresses more rapidly than MS, and because nerve cells are the targets that become damaged, the prognosis is at best, fair to poor.
How Are Als And Ms Diagnosed
To make a diagnosis, your doctor will ask for detailed information about your symptoms and your health history. There are also tests they can perform to help make a diagnosis.
If ALS is suspected, your doctor may order electrodiagnostic tests, such as an electromyography or a nerve conduction study.
These tests provide information on the transmission of nerve signals to your muscles and can show certain patterns that are consistent with a diagnosis of ALS.
A muscle or nerve biopsy may also be recommended for evaluation of ALS.
Your doctor may also order blood and urine samples, or perform a lumbar puncture to examine your spinal fluid.
MRI scans or X-rays may be ordered as well. If you have an MRI scan, you may have special images ordered to increase visualization of demyelinating areas in the brain and spine.
Doctors can use MRI results to distinguish between MS and ALS. MS targets and attacks myelin in a process called demyelination.
Demyelination prevents the nerves from performing as well as they once did, and it can be detected by an MRI scan.
On the other hand, ALS attacks the motor neurons, which doesnt appear on brain or spine MRIs.
Theres no cure for either condition, but treatments are available.
Read Also: Parkinson’s Prognosis Life Expectancy
Parkinson And Its Hallmark Symptoms
Parkinsons is a neurodegenerative disease that leads to shaking, stiffness, and difficulty with walking, and causes a person to lose control over some body functions.
Syndrome progresses gradually and differs from individual to individual. Parkinsons patients also experience mood swings accompanied by depression and anxiety.2
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Recommended Reading: What Causes Parkinson’s Patients To Die
What Is The Difference Between Progressive Supranuclear Palsy & Parkinsons Disease
Both PSP and Parkinsons disease show similar symptoms such as stiffness, movement difficulties, and clumsiness, but the severity of the condition is often based on the symptoms.1
Progressive supranuclear palsy is more progressive when compared to Parkinsons disease.2
PSP is a rare brain disorder that causes serious and progressive problems whereas Parkinsons disease is a nervous system disorder that affects movements.3,4
Many studies were conducted based on the facts of the two diseases that presented very similar symptoms, but they are quite different from each other when analyzed in detail.
PSP and Parkinsons have overlapping symptoms, but diagnosis often becomes complicated. However, experts suggest that PSP is more severe with cognitive impairment when compared to Parkinsons disease. Concentration and memory are most severely affected in patients with progressive supranuclear palsy.
Parkinsons Disease Vs Als: Risk Factors And Complications
Risk factors for Parkinsons disease include being over the age of 50, being male, having a family history of Parkinsons disease, carrying gene variations, experiencing a head injury, being exposed to environmental toxins, and taking certain medications such as anti-anxiety medications or sleeping pills.
Complications associated with Parkinsons disease include difficulty thinking, depression, emotional changes, swallowing problems, sleep problems and disorders, bladder issues, constipation, changes in blood pressure, smell dysfunction, fatigue, pain, and sexual dysfunction.
Studies into ALS have revealed some interesting insight. For example, it may just be that some people with this disease are triggered by certain environmental factors. The environmental triggers under investigation include smoking, lead exposure, and military service. Recent research has indicated that people who have served in the military are at a higher risk of getting ALS.
Studies are also looking at the entire human genome, since research has uncovered a number of genetic variations that people with familial ALS and some with non-inherited ALS have in common. These variations might make people more prone to ALS.
Also Check: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Training With Iqoro A Complement To Rehabilitation
IQoro is a new and unique neuromuscular treatment method that requires just 30 seconds exercise, three times per day. Exercising with IQoro can contribute to retaining and maintaining as much as possible of the normal functions for an extended period.
This is possible because IQoro activates the internal involuntary muscles in the same way that traditional physiotherapy strengthens arms and legs. Training with IQoro therefore it makes a positive difference in the ability to continue to eat via the mouth, chew, use facial expressions and to form sounds for an extended time.
IQoro is unique in being able to effectively activate the involuntary musculature from the face, oral cavity, pharynx, and the esophagus, down to the diaphragm.
The treatment is a good complement to physiotherapy as only a short exercise period is required one and a half minutes per day, and that the training has no negative side effects except for possible exercise stiffness in the early days. IQoro cannot, of course, treat the underlying disease.
Excessive Daytime Sleepiness In Pd
Excessive daytime sleepiness involves symptoms of frequent napping, feeling abnormally sleepy and sleep attacks. It is seen in 3376% of patients with PD and is likely a result of damaged to the orexin-producing neurons from the posterior lateral hypothalamus involved in the wakefulness . Other brainstem stimulating monoaminergic neurons are also implicated in promoting wakefulness in damaged in PD . EDS is common in advanced PD and is a marker of dopamine loss . Table 6 display the condition more commonly associated with EDS in PD.
| Severe PD |
Don’t Miss: Can Parkinson’s Run In The Family
How Are They Alike
MS and Parkinsonâs both affect your central nervous system, which includes your brain and spinal cord. Thatâs why they both can affect how you move, sleep, feel, and talk.
These diseases both affect your nerves. MS can break down the coating, called myelin, that surrounds and protects your nerves. In Parkinsonâs, nerve cells in a part of your brain slowly die off.
Both can start out with mild symptoms, but they get worse over time.
Common symptoms of both diseases include:
- Shaky fingers, hands, lips, or limbs
- Slurred speech thatâs hard for others to understand
- Numb or weak limbs that make your walk unsteady
- Loss of muscle control that often affects one side of your body at first, then later both
- Spastic limb movements that are hard to control
- Loss of bladder or bowel control
- Poor balance
Depression is another symptom common to both conditions.
