Imaging Studies Can Differentiate Parkinsons From Other Causes Of Parkinsonism
Catherine L. Gallagher, MD
Although Parkinsons disease remains a clinical diagnosis, imaging studies are an important ancillary test for differential diagnosis of movement disorders. Imaging studies may be used to rule out structural and other causes of parkinsonian symptoms. Single-photon emission computed tomography scans using labeled tracers for dopamine transporters can also be used to confirm parkinsonism or differentiate PD from secondary causes of parkinsonian motor symptoms. Finally, imaging studies are being used in research to better understand the pathophysiology of PD and elucidate causative mechanisms that could be therapeutic targets in the future.
What Should I Expect During The Mri
As the MRI scan begins, you will hear the equipment making a variety of banging, clanging and muffled thumping sound that will last for several minutes. None of them are anything other than annoying. Other than the sound, you should experience no unusual sensations during the scanning.
Certain MRI exams require an injection of a contrast material. This helps identify certain anatomic structures on the scan images.
Please feel free to ask questions. Tell the technologist or the doctor if you have any concerns.
Amyloid Scan To Detect Alzheimers Plaques
The Amyloid scan uses the tracer Amyvid to detect the brains level of amyloid plaque, an indicator of Alzheimers disease. A negative scan indicates that the symptoms of cognitive decline are caused by something other than Alzheimers, and is useful at ruling out the disease. A positive scan does not necessarily confirm an Alzheimers diagnosis, but it can be quite revealing and helpful in managing treatment.
Also Check: Can Parkinson’s Change Your Personality
Exclusion Of Symptomatic Parkinsonism
Structural brain imaging using cMRI with visual assessment of T2- and T1-weighted sequences including contrast-enhanced T1 imaging is usually normal in patients with early PD thus, its traditional role is the detection/exclusion of other underlying basal ganglia or brainstem pathologies . These include vascular, space-occupying or demyelinating lesions within the basal ganglia or brainstem, drug- or toxic-induced parkinsonism, e.g. due to manganism, or neurodegeneration with brain iron accumulation , normal pressure hydrocephalus, or infectious causes . Typical MR findings in patients with symptomatic parkinsonism are summarized in Table .
Diagnosing And Treating Parkinsons Disease

The diagnosis of Parkinsons disease is largely based upon the type of symptoms that the patient experiences. When someone has symptoms such as tremors or shaking of arms or legs while at rest, muscle stiffness or slow movements, Parkinsons disease must be a consideration, particularly if the individual is at a typical age for the onset of the disorder. Not all patients have every symptom, and often the symptoms start on one side of the body and then progress over time to include the other side. A good response to a trial of Parkinsons disease medication also helps to add confidence to the diagnosis.
The symptoms of Parkinsons disease can be similar to the symptoms of other conditions, and it is frequently misdiagnosed. Skilled doctors who specialize in the treatment of Parkinsons disease are the best practitioners to see for an accurate diagnosis.
The diagnostic process begins with a full medical history and neurological exam, testing movement, strength, coordination, balance, and reflexes. A doctor will often order additional tests to make sure that there are no other conditions present that could explain the patients symptoms. These tests may include an MRI of the brain and/or spine, or diagnostic tests of the electrical responses of muscles and nerves. In Parkinsons disease, these are usually normal and are performed to make sure that there are not problems other than Parkinsons disease that could explain symptoms.
Treatment Options
You May Like: Early Onset Parkinson\’s Prognosis
Mri Brain Scans Detect People With Early Parkinson’s
Oxford University researchers have developed a simple and quick MRI technique that offers promise for early diagnosis of Parkinson’s disease.
The new MRI approach can detect people who have early-stage Parkinson’s disease with 85% accuracy, according to research published in Neurology, the medical journal of the American Academy of Neurology.
‘At the moment we have no way to predict who is at risk of Parkinson’s disease in the vast majority of cases,’ says Dr Clare Mackay of the Department of Psychiatry at Oxford University, one of the joint lead researchers. ‘We are excited that this MRI technique might prove to be a good marker for the earliest signs of Parkinson’s. The results are very promising.’
Claire Bale, research communications manager at Parkinson’s UK, which funded the work, explains: ‘This new research takes us one step closer to diagnosing Parkinson’s at a much earlier stage one of the biggest challenges facing research into the condition. By using a new, simple scanning technique the team at Oxford University have been able to study levels of activity in the brain which may suggest that Parkinson’s is present. One person every hour is diagnosed with Parkinson’s in the UK, and we hope that the researchers are able to continue to refine their test so that it can one day be part of clinical practice.’
We think that our MRI test will be relevant for diagnosis of Parkinson’s
Dr Michele Hu
Is Early Diagnosis Possible
Experts are becoming more aware of symptoms of Parkinsons that precede physical manifestations. Clues to the disease that sometimes show up before motor symptoms and before a formal diagnosis are called prodromal symptoms. These include the loss of sense of smell, a sleep disturbance called REM behavior disorder, ongoing constipation thats not otherwise explained and mood disorders, such as anxiety and depression.
Research into these and other early symptoms holds promise for even more sensitive testing and diagnosis.
For example, biomarker research is trying to answer the question of who gets Parkinsons disease. Researchers hope that once doctors can predict that a person with very early symptoms will eventually get Parkinsons disease, those patients can be appropriately treated. At the very least, these advances could greatly delay progression.
Parkinson’s Disease and Movement Disorders Center
Our center provides compassionate and timely treatment to patients with movement disorders, such as dystonia, ataxia, essential tremor and similar conditions. But our mission goes beyond patient care excellence. By offering educational events and support groups, we empower patients and caregivers to become better partners in their health.
Also Check: Essential Oils For Hand Tremors
Exclusion Of Atypical Parkinsonism
The umbrella term atypical parkinsonism covers neurodegenerative disorders that feature rapidly progressive parkinsonism together with additional, often debilitating symptoms that are uncharacteristic for idiopathic PD. MSA, PSP and CBD fall under this category. Neuropathologically, PD and MSA share prominent alpha-synuclein inclusion pathology. Intriguingly, inclusion bodies in MSA patients are predominantly seen in oligodendrocytes, whereas Lewy bodies are mostly seen in the cytoplasm of neurons. In contrast to these disorders, PSP and CBD are considered to be tauopathies with 4-repeat tau protein accumulation. For adequate patient counselling, it is important to recognize these atypical disorders since the natural course of these disorders and treatment options are different from PD. In addition, to reduce between-subject heterogeneity in interventional trials, early and accurate diagnosis is at utmost importance. However, on clinical grounds, degenerative parkinsonian disorders can be indistinguishable from one another in early disease stages and, therefore, additional investigations such as MRI may become necessary to correctly diagnose patients with atypical parkinsonism .
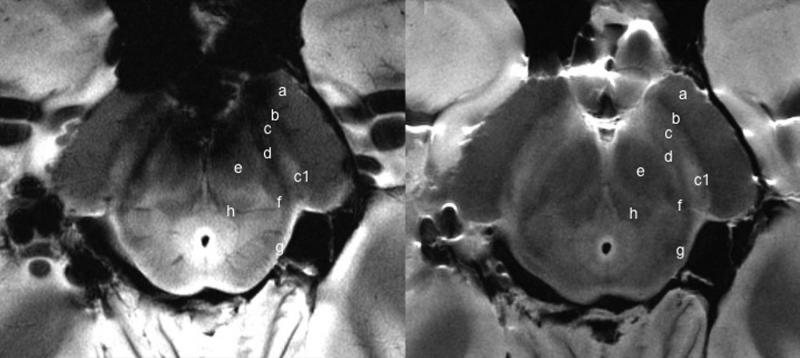
Structural MRI with conventional MRI sequences
Modified from Neuroimaging of Movement Disorders,Structural MRI in Idiopathic Parkinson Disease and Parkinsonism, Volume 44 of the series Current Clinical Neurology, 2013, pp 105-128, Mueller C et al., with permission of Springer
Quantitative MRI
Mri In Parkinson’s Testing
One of the more common tests done during a neurologic workup is an MRI scan and one may think that in the investigation of a disease that affects the brain such as Parkinsons, this imaging test would be a necessity. In the context of Parkinsons disease, however, an MRI is not particularly helpful. It looks at the structure of the brain which, for all intents and purposes, appears normal in this disease. An MRI may, however, be indicated when symptoms appear in younger people or if the clinical picture or the progression of symptoms is not typical for Parkinsons. In these situations, MRI can be used to rule out other disorders such as stroke, tumors, hydrocephalus , and Wilsons Disease .
Recommended Reading: Medial Inferior Pontine Syndrome
Tests To Rule Out Other Conditions
Blood tests can help rule out other possible causes of the symptoms, such as abnormal thyroid hormone levels or liver damage.
An MRI or CT scan can check for signs of a stroke or brain tumor, which may cause similar symptoms.
Hydrocephalus due to atrophy can occur with some types of dementia and would be visible with one of these imaging tests. If the person has neurologic symptoms but a normal scan result, Parkinsons disease may be present.
The doctor a lumbar puncture to rule out inflammation or a brain infection.
What Is Parkinson’s Disease
Parkinson’s disease is a disorder that affects the nervous system and movement.2,3 The symptoms typically begin gradually, and it may take a while for patients to notice them. These symptoms may include tremors, slow movement, rigid muscles as well as speech and writing changes. Patients may also experience impaired posture and balance or loss of automatic movements, such as blinking, smiling or swinging their arms.
Parkinson’s has a variety of risk factors that should be considered. In many cases, Parkinson’s usually affects people who are 50 years of age or older.2,3 However, some patients may experience young onset Parkinson’s disease, also called early-onset Parkinson’s disease, which affects roughly 2-10% of the population with Parkinson’s in the United States.3 Men may be more likely to develop Parkinson’s disease than women.2 If a close relative has Parkinson’s disease, a patient may be more likely to develop the disorder. The risk may still be small unless there are a large number of relatives with Parkinson’s disease. Finally, long-term exposure to herbicides and pesticides may slightly increase a patient’s risk.2
Once the disease has begun to progress, there are five stages that patients may experience.
Recommended Reading: Weighted Blanket Parkinson’s
Brain Imaging In Parkinsons Disease
Traditional brain imaging with CT and MRI scans do not show changes in the brain when someone has Parkinsons disease and are generally not helpful in diagnosis. A new kind of brain scan, called a DaT scan, does show changes in persons with Parkinsons disease and may someday become an important tool in diagnosing Parkinsons.
The dopamine transporter, or DaT, scan uses a chemical that labels the dopamine transporter in the area of the brain known as the striatum. Dopamine is a neurochemical that is decreased in persons with Parkinsons disease.
The dopamine transporter, which moves dopamine in and out of cells, is also decreased in the striatum in persons with Parkinsons disease and related disorders. The chemical that labels the transporter is injected into the vein and can be imaged by using something called single photon emission computerized tomography, or SPECT scanning. This technique has been registered in the European Union since 2000 for differentiating a diagnosis of essential tremor and a parkinsonian syndrome. It was approved by the Food and Drug Administration in 2011 for this same indication and recently became available at the OHSU Brain Institute.
Where To Get A Parkinsons Mri
Your two main choices if youre thinking about a Parkinsons MRI are a hospital and a free-standing imaging center. An imaging center offers you a comfortable environment with the highest quality equipment and technicians who are extremely experienced and focus exclusively on imaging. Imaging centers are also more affordable than hospitals.
Do you need a Parkinsons MRI? Are you a doctor who wants to schedule a Parkinsons MRI for a patient? Then, contact us today. At American Health Imaging, we focus on imaging, and we would love to help you.
Also Check: Do You Die From Parkinson’s Disease
What Are The Treatments
Currently there is no cure for Parkinsons disease.
Symptoms can be mild in the early stages of the condition and people might not need immediate treatment. Your doctor and specialist will monitor your situation.
There are several different types of drugs used to treat Parkinsons disease. Drug treatments are tailored to each individuals needs and are likely to involve a combination of different drugs. Your medication should be reviewed regularly. It is likely that, over time, changes will be made to the types of drugs you take and the doses you take each day.
The main types of drug treatment for Parkinsons disease are:
- drugs which replace dopamine
- drugs which mimic the role of dopamine
- drugs which inhibit the activity of acetylcholine
- drugs which prevent the body breaking down dopamine
- other drugs such as anti-sickness medication
Everybody is affected differently by medication. The possible side effects of Parkinsons disease drugs include nausea , vomiting , tiredness and dizziness. Some people might experience confusion, nightmares and hallucinations. For some people, dopamine agonists have been linked to compulsive behaviour such as addictive gambling or hypersexuality .
The effectiveness of the main drug treatment levodopa can wear off over time and its long-term use can cause some people to develop involuntary twisting or writhing movements of the arms, legs or face . To reduce the risk, doctors might delay the use of levodopa for younger people.
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Also Check: What Are Early Warning Signs Of Parkinson’s Disease
Regional Differences In Gmd Slope Directionality
To further test differences in disease progression between early and PD groups, a comparison of the directionality of the early and PD slope parameters for the age and sex adjusted relationships between duration of disease and GMD was performed. For subcortical regions in early PD, one region had a positive slope, compared to 12 regions which had a negative slope. For subcortical regions in advanced PD patients, all 13 regions had a negative slope. For cortical regions in early PD, 13 regions had a positive slope, compared to one region which had a negative slope. For cortical regions in advanced PD patients, all 14 regions had a negative slope. The difference in the distribution of positive and negative slopes for subcortical and cortical regions in early PD is significant . Additionally, the difference in the distribution of positive and negative slopes for cortical regions between early PD and advanced PD is significant .
What Is Parkinson’s And How Can Mri Help
More than ten million people are living with Parkinson’s disease worldwide, with about one million cases expected to be in the United States by 2020.1 This is more than the number of people with multiple sclerosis, muscular dystrophy and Lou Gehrig’s disease combined.1 With the rising prevalence of Parkinson’s disease, its important to understand the signs and symptoms of the disease. Likewise, physicians and radiology departments may need to know what role magnetic resonance imaging may play.
Read Also: What Are Early Warning Signs Of Parkinson’s Disease
How Can Magnetic Resonance Imaging Help
Magnetic resonance imaging is used to monitor a large variety of disorders and diseases throughout the body. the images produced during an MRI scan may show tissue structures and organs in excellent detail. Functional MRI is one technique that can provide information about the body during certain activities. Both conventional and functional MRI may help show the progress of diseases, including Parkinson’s disease, and may show the response to treatments.
Functional MRI may be used to image the brain during movement. Research for Parkinson’s disease has included fMRI to monitor what regions are activated during automatic motion.4 This study of 12 patients with Parkinson’s disease practiced sequences of finger movement until they were able to be done automatically. Then, they underwent fMRI to compare their scans before and after they had learned the sequences. The results showed that the most of the same areas of the brain were active while performing the sequences before or after they became automatic. Subjects without Parkinson’s had significantly reduced activity in the brain after automaticity. This means that patients with Parkinson’s disease had more trouble performing the actions than the people without.
The Importance Of Early Diagnosis
Early detection and diagnosis is important because the treatments for PD are more effective in the early stages of the disease. In addition, physical therapy and exercise, which greatly improve symptoms and delay progression of the disease, are much easier to perform in the early stages.
Current diagnosis is made through the presence of motor symptoms however, researchers have found that by the time motor symptoms occur, over 60% of all dopamine neurons in the basal ganglia of the brain have been damaged. Non-motor symptoms become apparent in people with PD long before motor symptoms, including sleep disturbances and loss of the sense of smell.3
Active areas of research include looking for markers in the blood, urine, or cerebral spinal fluid that reliably detect PD, called biomarkers. In addition, brain imaging tests that have high sensitivity for detecting PD are also being actively researched.4
Don’t Miss: What Is The Life Expectancy For Someone With Parkinson Disease
If Its Not Parkinsons Disease What Could It Be
Here are some possibilities:
Side effects of medication: Certain drugs used for mental illnesses like psychosis or major depression can bring on symptoms like the ones caused by Parkinsonâs disease. Anti-nausea drugs can, too, but they typically happen on both sides of your body at the same time. They usually go away a few weeks after you stop taking the medication.
Essential tremor: This is a common movement disorder that causes shaking, most often in your hands or arms. Itâs more noticeable when youâre using them, like when you eat or write. Tremors caused by Parkinsonâs disease usually happen when youâre not moving.
Progressive supranuclear palsy: People with this rare disease can have problems with balance, which may cause them to fall a lot. They donât tend to have tremors, but they do have blurry vision and issues with eye movement. These symptoms usually get worse faster than with Parkinson’s disease.
Normal pressure hydrocephalus : This happens when a certain kind of fluid builds up in your brain and causes pressure. People with NPH usually have trouble walking, a loss of bladder control, and dementia.
