How Can I Support Someone With Parkinson’s Towards The End Of Life
In the advanced stages of Parkinsons, your patients care needs may be more complex and require careful planning along with the patient, their family and other health and social care professionals involved.
Palliative care should be holistic, considering the whole person to support the personal, social, psychological and spiritual needs of your patient and their family. It should give your patient some control and choice over areas such as treatment options and where they will be cared for, as well as providing advice and support to all the people involved in their care.
Palliative care in Parkinsons may be supported by a number of professionals, including a Parkinsons nurse specialist, local hospice or specialist palliative care team, physiotherapist, occupational therapist, speech and language therapist or dietitian. Many people with Parkinson’s also find complementary therapies beneficial.
It is important that you find out whether the person has a care plan in place regarding their preferences for how the issues surrounding advanced Parkinsons should be managed. This could include legal documentation such as a Lasting Power of Attorney and an advance care plan. Advance care plans include information on what the persons wishes and preferences are for their care in the future. They may include decisions on any treatments the person does not want to have in the future this is called an Advance Directive, Advance Decision to Refuse Treatment or Living Will.
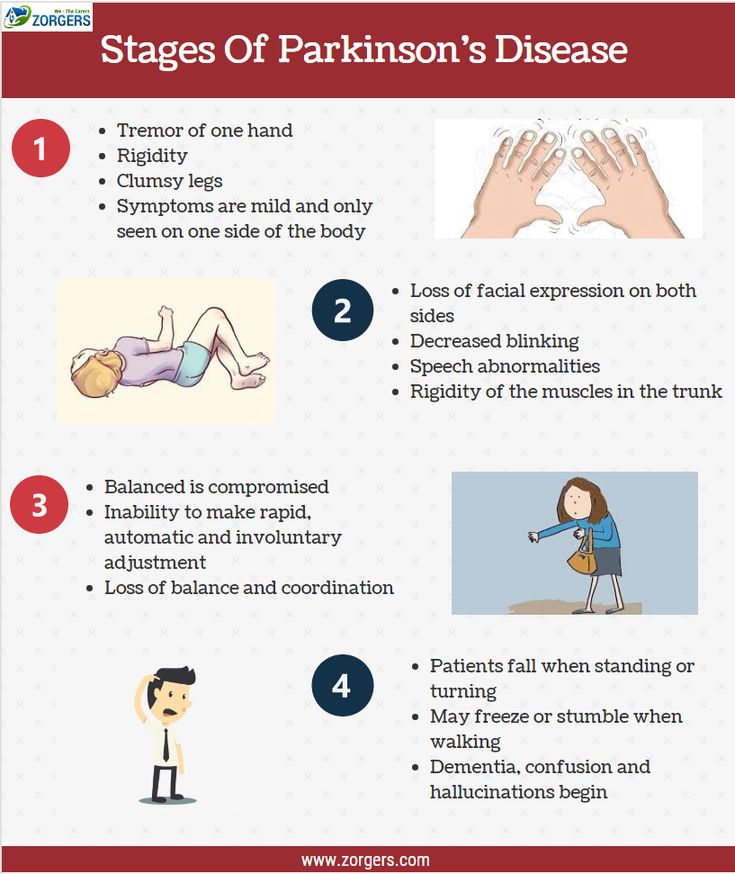
Stage One: Symptoms Affect Only One Side Of Your Body
The initial phase of Parkinsons disease typically presents with mild symptoms. Some patients will not even detect their symptoms in the earliest phases of this stage. Typical motor symptoms experienced in Stage One include tremors and shaking limbs. Family members and friends may begin to notice other symptoms including tremor, poor posture, and mask face or loss of facial expression.
How Care Providers Can Assist With Late Stage Parkinsons Care
With added hands-on care required, its essential for family caregivers to learn how to properly and efficiently provide this support to minimize the possibility of doing harm to either themselves or the loved one being cared for.
If the older adult isnt already receiving physical therapy services, check with the physician for a referral. The physical therapist, while helping optimize the persons ability level, may also advise family caregivers on the ideal approaches for hands-on assistance.
One new symptom that frequently develops in the later stages of Parkinsons is freezing, when the person is suddenly unable to move. Methods to help break a freezing episode include:
- Using a laser pointer and asking the person to step on the light
- Utilizing a rhythmic noise, such as clapping, and encouraging the person to take a step with each clap
- Playing music and prompting the individual to walk to the beat
As always, stay close at hand when the person is mobile to avoid a fall.
Make sure to provide an abundance of extra time for day-to-day activities such as getting dressed and eating, which are likely to take longer now. This is important in protecting the persons self-sufficiency. Even if it requires longer to accomplish a task, it is always better to foster as much self-reliance as you possibly can.
You May Like: How Dopamine Affects Parkinson’s Disease
What Is Parkinsons Disease
Parkinsons disease is a progressive brain disorder that affects mobility and mental ability. If you or a loved one has been diagnosed with Parkinsons, you may be wondering about life expectancy.
According to some research, on average, people with Parkinsons can expect to live almost as long as those who dont have the condition.
When To Seek Hospice Care
When you or your loved one have a life expectancy of six months or less, you become eligible for hospice care a type of comfort care provided at the end of life for someone living with end-stage Parkinsons disease. Hospice provides extra support so your loved one can live as comfortably as possible.
If you have experienced a significant decline in your ability to move, speak, or participate in activities of daily living without caregiver assistance, its time to speak with a hospice professional.
Read more: What is hospice care?
Some of the things that determine whether your loved one with end-stage Parkinsons is eligible for hospice include: difficulty breathing, bed bound, unintelligible speech, inability to eat or drink sufficiently, and/or complications including pneumonia or sepsis.
If you live in South Jersey, our nurse care coordinator can answer your questions and decide if your loved one is ready for hospice care. Call us 24/7 at 229-8183.
Also Check: Is Parkinson’s Disease Terminal
How Will The Person With Advanced Pd Experience Death
The journey for every person with PD will be different. Their symptoms, disease progression, access to medical care, and their concurrent medical issues may vary widely and play a role in their life and their death with PD. As described above, the person with advanced PD typically dies from an event that occurs on top of the increasing levels of frailty and disability that build up over time. That event may be a fall, an infection, a choking event, or another medical issue that leads to a hospitalization and causes a more precipitous decline.
Regardless of the cause, when a neurologist assesses that the possibility of death within a particular time frame is likely, hospice care can be initiated. This is different from palliative care, which is a clinical approach that focuses on improving quality of life for people with complex diseases. Palliative care can begin at any point during the disease progression and work in conjunction with the treatment plan. Hospice care, on the other hand, is provided to improve the quality of life when end of life is near.
In summary, while it is true that PD in and of itself is not fatal in the same way that a rupture of a brain aneurysm or a massive heart attack may be , the disability caused by PD can contribute to death in a variety of ways as outlined above. Educating yourself on the various possibilities and areas of concern may help you better prepare for the future, minimize some risks, and possibly enhance or prolong quality of life.
Starting Palliative Care In Patients With Pd
Patients with PD benefit early from palliative care in view of the impact of the disease impairing autonomy and quality of life. The provision of palliative care in patients with PD focuses on unmet needs and should be aligned with patient priorities. It is recommended that a palliative care approach should be applied from the early phase, throughout the course of the disease, complementing but not replacing other treatments . However, like other patients with chronic neurological condition, the individual needs may vary over time, therefore it is suggested that a model of dynamic involvement of palliative care services should be adopted . The services can be triggered at times of particular symptoms or psychosocial issuessuch as the start of new interventions or at the very end of life.
For patients with complex physical, social, psychological and/or spiritual needs that do not respond to simple or established protocols of palliative care, there should be access to the support from specialist palliative care service .
However, rate of use of hospice in PD patients has been low . Caregivers often considered palliative care services to be synonymous with hospice care, and hence they did not consider this service option . Health care workers also have uncertainty about timing of palliative care, such that it was often not introduced until a crisis point .
Don’t Miss: Parkinson’s Copay Assistance Program
Palliative Care Management Of Non
Patients with PD can develop non-motor manifestations, categorized into autonomic dysfunction, cognitive impairment, neuropsychiatric disorders, and sleep disturbances. At the end-stage of PD, non-motor symptoms become more common and can become the most prominent medical problem, leading to increasing decline in quality of life both for patient as well as increasing caregiver burden . Non-motor symptoms occur in up to 50% of PD patients especially in association with the medication off state and may become worse by anti-PD medications . Almost one third of patients reports their non-motor symptoms to be at least as debilitating as their motor symptoms .
All patients with motor fluctuations face at least one non-motor problem during the off phase . In end-stage of PD, dementia, psychosis, and falls become more complex to manage than the motor complications as a result, managing non-motor aspects is important to increase quality of life and decrease the burden of illness . Chaudhuri and co-workers, using a new 30-item non-motor symptom screening questionnaire , found noticeably high scores among PD patients for impaired taste/smell, impaired swallowing, weight loss, constipation, urinary urgency, forgetfulness, dribbling, sadness, hallucinations, anxiety, sexual dysfunction, falling, reduced concentration, daytime sleepiness, vivid dreams, and sweating .
Surveillance Epidemiology And End Results Program
tracks a persons 5-year relative survival rate based on how far the cancer has spread throughout the body:
- Localized: The cancer has not spread outside the liver.
- Regional: The cancer has spread to nearby structures and lymph nodes.
- Distant: The cancer has spread to distant parts of the body.
A relative survival rate helps give an idea of how long a person with a particular condition will live after receiving a diagnosis compared to people without the condition.
For example, if the 5-year relative survival rate is 70%, it means that a person with the condition is 70% as likely to live for 5 years as someone without the condition.
The 5-year relative survival rate is 12.8% for regional stage liver cancer and 3.1% for distant stage liver cancer.
The following symptoms may indicate end stage liver cancer. Certain symptoms may also indicate that a person is nearing the end of life.
Recommended Reading: Does Parkinson’s Cause Fatigue
Parkinsons Disease: When Is It Time For Hospice
Knowing when its time for hospice care when living with Parkinsons Disease can be difficult as the disease may take many years to progress and each person with the disease may also exhibit a range of different symptoms. However, entering the end-stages of the disease , patients will have symptoms that will indicate that it is time to seek hospice assistance:
How To Manage Symptoms At The End Of Life
At the end of life, good practice is to plan for any potential symptoms that may arise. The most common symptoms anticipated are pain, dyspnoea, nausea and vomiting, agitation, anxiety, delirium and noisy respiratory secretions.18 For patients with PD particular considerations should be given to the more commonly used medicines, specifically anticholinergics and antidopaminergics. These are usually prescribed for treatment of respiratory secretions and nausea and vomiting. Alternatives are available for respiratory secretions, and include glycopyrronium, in preference to hyoscine hydrobromide. Although this is an anticholinergic, only a small proportion crosses the blood brain barrier.
For nausea and vomiting, ondansetron,19 cyclizine, domperidone have all been suggested in PD.20 However, ondansetron has been shown to be inferior to domperidone in the pre-treatment of apomorphine.21 Cyclizine has anticholinergic properties and may exacerbate confusion, especially when comorbid psychosis or cognitive impairment are present. Levomepromazine, although it has antidopaminergic effects, has been shown to be effective for nausea with rotigotine in a case report.22
Agitation, dyspnoea and pain can all be managed with the same anticipatory medications as recommended.20 Specifically relating to PD, several case reports have supported the intraoperative use of midazolam, during sedation, for tremor and dyskinesias,23,24 as well as for agitation at the end of life.20
Read Also: Does Parkinson’s Cause Anger
Palliative Care In Parkinson’s Disease
In the absence of any curative treatment, the principles of palliative care should be applied throughout the course of the disease and not limited to the terminal end-of-life period. This chapter defines palliative care and discusses the palliative phase of Parkinson’s disease, palliative carers, care homes, social costs, withdrawl of drugs, pressure ulsers, end-of-life issues, recommendations and ethical issues.
Treatment To Slow Parkinsons Disease Progression
Researchers continue to study medications and therapies with the hope of slowing progression.
Levodopa is a first-line medication that clinicians prescribe for Parkinsons disease symptoms, but it does not slow disease progression, says the NINDS.
The body uses levodopa to produce dopamine. Doctors often prescribe it alongside carbidopa, a medication that reduces the negative side effects of levodopa.
Deep brain stimulation is a surgical treatment option for people who do not respond well to or are not candidates for medication. This surgery targets the movement symptoms of Parkinsons disease.
The NINDS states that DBS does not stop PD from progressing. However, a 2020 study showed that DBS decreases the risk of disease progression in a trial of people with early-stage Parkinsons disease. Over a 5-year study period, people receiving DBS were less likely to need increasingly higher doses of levodopa to manage symptoms.
Doctors prescribe medications and lifestyle practices to help with other symptoms of Parkinsons disease.
Nancy Hammond, M.D., reviewed the following questions.
Read Also: What Happens If You Stop Taking Parkinson’s Medication
Caring For A Family Member With Late Stage Parkinsons Disease: Part 3 Of 3
The late stage of Parkinsons disease can present new caregiving challenges for family members.
A Parkinsons diagnosis affects family members along with the person who is afflicted. Understanding what to anticipate as the illness progresses is the key to being prepared for the changes to come and to making life the very best it can be each and every day.
Over the last few months, we have shared information about what to anticipate in the early and middle stages of Parkinsons disease. Information has included what family members can do to best help a loved one with Parkinsons and how Abby Senior Care can help. In this closing segment in the series, we provide information about taking care of someone with late stage Parkinsons disease.
When Should I Think About Advanced Stages
You, or the person you care for, may not be experiencing advanced symptoms at the moment.
But you may wish to read about advanced Parkinson’s now, so you can be prepared as things arise, and deal with any difficult decisions that need to be made.
You’ll have the chance to think about what you may like to happen if you become unwell, or if you experience symptoms of dementia.
Discussing your wishes with your family, and writing them down, will help them if they need to make decisions about your care.
You May Like: Does Parkinson’s Run In The Family
Symptom Burden In Advanced Pd
There are established guidelines in management of motor and non-motor symptoms in PD. However, symptom burden in advanced PD is still high, and it has been reported to be of similar degree as in metastatic cancer .
The motor symptoms of PD progress over years and the Hoehn and Yahr scale is a commonly used system for describing this . After the honeymoon period in early years of PD when antiparkinsonian drugs usually provide excellent control over the motor symptoms of bradykinesia and rigidity, majority of patients begin to experience less reliable drug response upon disease progression. Patient would experience complications from the long-term drug treatment, including motor fluctuations and dyskinesia. In advanced PD, prominent motor symptoms, as reported in a cohort of 50 patients with stage 4 or 5 of Hoehn and Yahr, include severe akinesia, postural instability, freezing of gait, dysarthria and dysphagia .
Table 2
From the patients perspective, there is a recent questionnaire survey which included 814 PD patients who felt subjectively severely affected by their illness. The commonest reasons for feeling severely affected were mobility impairment , coordination problems , speech problems , and limited day-to-day activities , e.g., getting dressed and personal hygiene. Significant associations were observed between subjectively felt severe affectedness and Hoehn and Yahr, poorer health, higher nursing care level, and having no children .
Can I Afford Hospice Care
Medicare pays for hospice services under the Medicare Hospice Benefit. Under this benefit all care, medications and medical supplies related to the hospice diagnosis are completely covered. The benefit allows for months of care not just during the last weeks of life.
Medicaid and most private insurances also have a hospice benefit that covers costs. For patients not receiving Medicare, Medicaid or private insurance benefits, Lower Cape Fear LifeCare never refuses care based on someones ability to pay.
Recommended Reading: Is Fish Oil Good For Parkinson Disease
Therapeutic Management Of Late
, December 12, 2011
This review of the Movement Disorder Societys guidelines for therapeutic management of late-stage Parkinsons applies the guidelines to a case scenario. The guidelines first appeared in the European Handbook of Neurological Management. This review cites the Annals of Long-Term Care: Clinical Care and Aging, 2011 19 : 42-46.
Demographic And General Health Measures
Baseline demographic and general health predictors of mortality included age at onset or diagnosis, chronological age, male sex, body mass index and comorbid illness. For every year increase in age at onset, there was an associated increase in a range of HRs from a minimum 1.05 to a maximum 1.11 , with age ranging from 61 to 77 years of age at baseline for those who died. Multiple analyses estimated the impact of 10-year increases in age at onset on mortality, with increased HRs of 1.4 to 2.8 . Advanced chronological age or age at onset was estimated using a variety of methods, but in general found that patients with PDRD faced higher risk of death above 7885 years of age at onset. Male sex was associated with statistically significant increased HRs of 1.36 up to 2.9 compared with females RR increase of mortality of 1.7 and fivefold higher odds of death . In a retrospective repeated measures analysis, Goy et al found rapidly declining BMI was significantly associated with progression to death among patients with PDRD. A decrease in BMI was seen, from mean of 26 at 3036 months to 24.6 at 612 months prior to death. Further, an absolute BMI< 18 was a predictor of mortality.
You May Like: What Are Parkinson’s Off Episodes
