How Long Can A Person Live With Stage 5 Parkinson
. People also ask, what is end stage Parkinsons?
When patients reach stage five the final stage of Parkinsons disease they will have severe posture issues in their back, neck, and hips. In endstage of Parkinsons disease, patients will also often experience non-motor symptoms. These can include incontinence, insomnia, and dementia.
Additionally, what do Parkinsons patients usually die from? But the most common cause of death in those with Parkinsons is pneumonia, because the disease impairs patients ability to swallow, putting them at risk for inhaling or aspirating food or liquids into their lungs, leading to aspiration pneumonia.
Likewise, what happens in stage 5 Parkinsons?
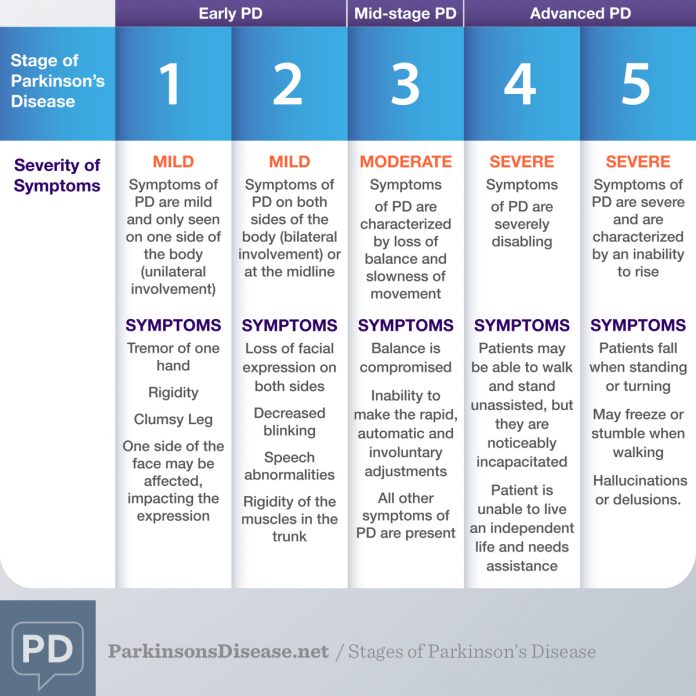
Stage Five of Parkinsons Disease Stage five is the most advanced and is characterized by an inability to arise from a chair or get out of bed without help. They may have a tendency to fall when standing or turning, and they may freeze or stumble when walking.
How quickly can Parkinsons progress?
While symptoms and disease progression are unique to each person, knowing the typical stages of Parkinsons can help you cope with changes as they occur. Some people experience the changes over 20 years or more. Others find the disease progresses more quickly.
You May Like: Power For Parkinsons Exercise Videos
Learn About The Brain
The Brain-Gut Connection is an exploding area of research for Parkinsons for a variety of reasons. As it turns out, your brain and your gut are intricately connected. As youre venturing into this new diagnosis of Parkinsons, shifting to eating in a way thats healthy for your gut is crucial as it impacts your brain health tremendously. I get dozens of questions each day on nutrition for Parkinsons, which is why I created a free four-part video series all about how to maximize your gut health. You can check it out here:
Parkinsons Medications And Sweating
In some cases, excessive sweatingor insufficient sweatingis part of the disease process due to autonomic nervous system involvement. In Parkinsons disease, excessive sweating affects the face, head, and trunk, while the palms may sweat less than usual.
Additionally, too much sweating or too little sweating can be side effects of some Parkinsons medications, although sweating too little is less common.
You May Like: Adaptive Silverware For Parkinsons
Don’t Miss: How Do Neurologists Diagnose Parkinson’s Disease
What Makes Pd Hard To Predict
Parkinsonâs comes with two main buckets of possible symptoms. One affects your ability to move and leads to motor issues like tremors and rigid muscles. The other bucket has non-motor symptoms, like pain, loss of smell, and dementia.
You may not get all the symptoms. And you canât predict how bad theyâll be, or how fast theyâll get worse. One person may have slight tremors but severe dementia. Another might have major tremors but no issues with thinking or memory. And someone else may have severe symptoms all around.
On top of that, the drugs that treat Parkinsonâs work better for some people than others. All that adds up to a disease thatâs very hard to predict.
Palliative Care Management Of Non
Patients with PD can develop non-motor manifestations, categorized into autonomic dysfunction, cognitive impairment, neuropsychiatric disorders, and sleep disturbances. At the end-stage of PD, non-motor symptoms become more common and can become the most prominent medical problem, leading to increasing decline in quality of life both for patient as well as increasing caregiver burden . Non-motor symptoms occur in up to 50% of PD patients especially in association with the medication off state and may become worse by anti-PD medications . Almost one third of patients reports their non-motor symptoms to be at least as debilitating as their motor symptoms .
All patients with motor fluctuations face at least one non-motor problem during the off phase . In end-stage of PD, dementia, psychosis, and falls become more complex to manage than the motor complications as a result, managing non-motor aspects is important to increase quality of life and decrease the burden of illness . Chaudhuri and co-workers, using a new 30-item non-motor symptom screening questionnaire , found noticeably high scores among PD patients for impaired taste/smell, impaired swallowing, weight loss, constipation, urinary urgency, forgetfulness, dribbling, sadness, hallucinations, anxiety, sexual dysfunction, falling, reduced concentration, daytime sleepiness, vivid dreams, and sweating .
Recommended Reading: How Does Parkinson’s Start
How To Manage Symptoms At The End Of Life
At the end of life, good practice is to plan for any potential symptoms that may arise. The most common symptoms anticipated are pain, dyspnoea, nausea and vomiting, agitation, anxiety, delirium and noisy respiratory secretions.18 For patients with PD particular considerations should be given to the more commonly used medicines, specifically anticholinergics and antidopaminergics. These are usually prescribed for treatment of respiratory secretions and nausea and vomiting. Alternatives are available for respiratory secretions, and include glycopyrronium, in preference to hyoscine hydrobromide. Although this is an anticholinergic, only a small proportion crosses the blood brain barrier.
For nausea and vomiting, ondansetron,19 cyclizine, domperidone have all been suggested in PD.20 However, ondansetron has been shown to be inferior to domperidone in the pre-treatment of apomorphine.21 Cyclizine has anticholinergic properties and may exacerbate confusion, especially when comorbid psychosis or cognitive impairment are present. Levomepromazine, although it has antidopaminergic effects, has been shown to be effective for nausea with rotigotine in a case report.22
Agitation, dyspnoea and pain can all be managed with the same anticipatory medications as recommended.20 Specifically relating to PD, several case reports have supported the intraoperative use of midazolam, during sedation, for tremor and dyskinesias,23,24 as well as for agitation at the end of life.20
What Are The Symptoms
The best-known symptoms of Parkinson’s disease involve loss of muscle control. However, experts now know that muscle control-related issues aren’t the only possible symptoms of Parkinson’s disease.
Motor-related symptoms
Motor symptoms which means movement-related symptoms of Parkinsons disease include the following:
Additional motor symptoms can include:
- Blinking less often than usual. This is also a symptom of reduced control of facial muscles.
- Cramped or small handwriting. Known as micrographia, this happens because of muscle control problems.
- Drooling. Another symptom that happens because of loss of facial muscle control.
- Mask-like facial expression. Known as hypomimia, this means facial expressions change very little or not at all.
- Trouble swallowing . This happens with reduced throat muscle control. It increases the risk of problems like pneumonia or choking.
- Unusually soft speaking voice . This happens because of reduced muscle control in the throat and chest.
Non-motor symptoms
Several symptoms are possible that aren’t connected to movement and muscle control. In years past, experts believed non-motor symptoms were risk factors for this disease when seen before motor symptoms. However, theres a growing amount of evidence that these symptoms can appear in the earliest stages of the disease. That means these symptoms might be warning signs that start years or even decades before motor symptoms.
Non-motor symptoms include:
Stages of Parkinsons disease
Recommended Reading: What Does Early Parkinson’s Feel Like
When Is It Time For Hospice Care
Even though the course of Parkinsons is predictable, the end stage of Parkinsons is not. Despite its severity, people dont pass on from Parkinsons rather, the disease leaves patients vulnerable to injury or infection which, in their weakened conditions, often proves to be fatal.
Consequently, knowing when to call hospice is not a simple matter of tracking symptoms. Physicians should always be consulted if patients are experiencing:
- Persistent pain
- Systolic blood pressure below 90
- Frequent falls or poor balance
- Recurrent infections
- Constant nausea
Once a doctor has given the patient a six-month prognosis, a hospice team can be called in. Patients can receive hospice wherever they call homeresidential care facilities, retirement communities or wherever theyve been residing.
Hospice serves both patients and families alike. It also gives patients a chance to spend their final weeks or months free from pain, while lifting a huge burden from families.
Hospice teams provide comfort care to patients. Comfort care provides relief from pain, nausea, and shortness of breath. Working closely with the patients doctor, the hospice team creates a personal care plan to manage symptoms. Nurses check in regularly to adjust pain medication. Home Health aides tend to the patients hygiene. Case managers secure high-grade equipment, such as hospital beds or oxygen machines.
Hospice Care For Late Stage Parkinsons
There are a number of reasons why choosing to have home health care services for Parkinson patients is one of the best options. Hospice care for late stage Parkinsons is extremely important.
- End of Life 40% of those who were in a long term care facility died alone without a family member being with them. Every person in the study listed who had in home health care and hospice had at least 1 significant family member or loved one with them at the time of their passing.
- Satisfaction 83% of those who utilized hospice were satisfied to highly satisfied with their experience. They cited their satisfaction with the ability to handle the extreme grief and handling of the symptoms of the disease as two of the main reasons for being appreciative with the care received.
- Focus Hospice care for late stage Parkinsons focuses on comfort care, symptom care, grief counseling and acceptance. Maintaining a level of understanding and comfort for both the patient and their loved ones is a primary goal.
We can see the importance of a loved one remaining at home as they battle PD, especially as they move towards the final stages of the disease. Above & Beyond Home Health Care can be there for you with professional hospice care for late stage Parkinsons so you know that your loved one is provided for with the best care possible.
Cited Works:
End of Life Care for a Person with Parkinson Disease Dept. of Education
Don’t Miss: How Do You Find Out If You Have Parkinson Disease
Signs Of Parkinsons Disease
In 1817, Dr. James Parkinson published An Essay on the Shaking Palsy describing non-motor, as well as, motor symptoms of the illness that bears his name. Parkinsons is not just a movement disorder, explained Dr. Shprecher. Constipation, impaired sense of smell, and dream enactment can occur years before motor symptoms of Parkinsons. The latter, caused by a condition called REM sleep behavior disorder, is a very strong risk factor for both Parkinsons and dementia . This has prompted us to join a consortium of centers studying REM sleep behavior disorder.
How Is Parkinson’s Managed
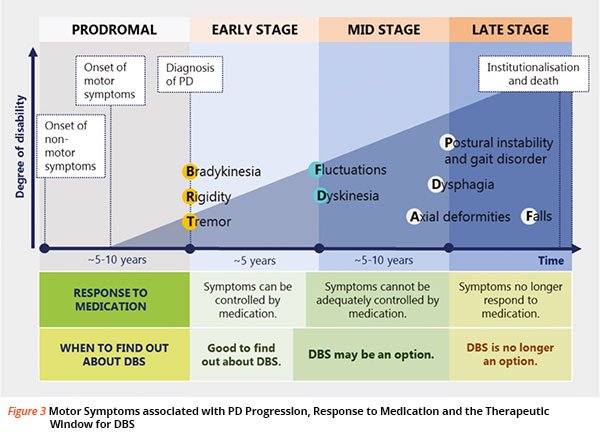
There is currently no cure for Parkinsons but there are medications and therapies that can help to manage Parkinsons symptoms.
Medicines that increase the level of dopamine in the brain are the main treatment used to manage the symptoms of Parkinson’s. Medicines are tailored to each individuals needs.
Symptoms will get worse when someones Parkinsons medicines are wearing off and improve again after Parkinsons medicines are taken. If people with Parkinsons do not get their medication at the right time, it leads to their motor symptoms becoming uncontrolled. It can take some time to get their symptoms under control again. If you work in a hospital or care home, it is important to be aware that medicine timings will vary from person to person and may be different to ward medicine rounds.
As well as medicines, surgical options are available for some people with Parkinson’s, depending on their symptoms.
Treatments can help to manage the symptoms, but may become less effective in the later stages of the condition.
Parkinsons UK has more information on how Parkinsons affects people and how it can be managed.
Also Check: Does Massage Help Parkinson’s Disease
How Soon After Treatment Will I Feel Better And How Long Will It Take To Recover
The time it takes to recover and see the effects of Parkinson’s disease treatments depends strongly on the type of treatments, the severity of the condition and other factors. Your healthcare provider is the best person to offer more information about what you can expect from treatment. The information they give you can consider any unique factors that might affect what you experience.
The 5 Stages Of Parkinsons Disease
Getting older is underrated by most. Its a joyful experience to sit back, relax and watch the people in your life grow up, have kids of their own and flourish. Age can be a beautiful thing, even as our bodies begin to slow down. We spoke with David Shprecher, DO, movement disorders director at Banner Sun Health Research Institute about a well-known illness which afflicts as many as 2% of people older than 65, Parkinsons Disease.
Recommended Reading: What Are The Environmental Causes Of Parkinson Disease
You May Like: Does Eddie Marsan Have Parkinson’s In Real Life
What Are The Risks Of Not Receiving Any Dopaminergic Medication
There is the possibility of neuroleptic malignant-like syndrome , a life-threatening and distressing condition resulting in rigidity and fever, from withdrawal of therapy.31 This can also occur with sudden cessation of Deep Brain Stimulation .32,33,34 To reduce the risk of this, dopaminergic therapy at the end of life should be continued.27 It should also be noted that in a patient dying of another condition, whose PD is still responsive to dopaminergic medication, the cessation of this also risks aspiration pneumonia.35 Transdermal rotigotine can be used in patients in whom a NG tube may cause excessive distress or is not possible. The dose should be calculated with an accepted converter.36
Data Abstraction And Risk Assessment
Any two of three investigators independently screened titles, abstracts and retrieved full papers with eligibility criteria. Differences were resolved by review of the third investigator.
We assessed risk of bias by reviewing study design characteristics, including appropriate temporal relationships between exposures and outcomes, matching populations through individual variables or propensity scores and other adjustment methods. However, given we did not develop a meta-analysis from the findings, we did not exclude reporting any studies that met our inclusion criteria.
Recommended Reading: What Is The Best Mucuna Pruriens For Parkinson’s
Parkinsons Disease Late Stage Complications
During the most advanced stage of Parkinsons typically between stages four and five a persons symptoms and medication regime become more complex.
Supporting care becomes especially important in advanced Parkinsons, with an estimated 50 to 80% of people eventually experiencing dementia and an increased number of falls.
Recommended Reading: Recipes For Parkinsons Patients
Causes Of Parkinsons Disease
The exact cause of Parkinsons is unknown. It may have both genetic and environmental components. Some scientists think that viruses can trigger Parkinsons as well.
Low levels of dopamine and norepinephrine, a substance that regulates dopamine, have been linked with Parkinsons. Abnormal proteins called Lewy bodies have also been found in the brains of people with Parkinsons. Scientists dont know what role, if any, Lewy bodies play in the development of Parkinsons.
While theres no known cause, research has identified groups of people who are more likely to develop the condition. These include:
- Sex: Men are one and a half times more likely to get Parkinsons than women.
- Race: Whites are more likely to get Parkinsons than African Americans or Asians.
- Age: Parkinsons usually appears between the ages of 50 and 60. It only occurs before the age of 40 in 5-10 percent of cases.
- Family history: People who have close family members with Parkinsons disease are more likely to develop Parkinsons disease, too.
- Toxins: Exposure to certain toxins may increase the risk of Parkinsons disease.
- Head injury: People who experience head injuries may be more likely to develop Parkinsons disease.
Also Check: Wolf Parkinsons White Disease Treatment
Read Also: What Brain Structure Is Affected By Parkinson’s
How Is Parkinson Disease Treated
Parkinson disease can’t be cured. But there are different therapies that can help control symptoms. Many of the medicines used to treat Parkinson disease help to offset the loss of the chemical dopamine in the brain. Most of these medicines help manage symptoms quite successfully.
A procedure called deep brain stimulation may also be used to treat Parkinson disease. It sends electrical impulses into the brain to help control tremors and twitching movements. Some people may need surgery to manage Parkinson disease symptoms. Surgery may involve destroying small areas of brain tissue responsible for the symptoms. However, these surgeries are rarely done since deep brain stimulation is now available.
Can A Patients Ability To Make Decisions In The Last Days Of Life Be Impaired And How Is This Managed
In a North American study of 47 carers of idiopathic PD patients in the last months of life most described the goal of care as comfort, and almost half of the patients were described as unable to make any decisions in the last month of life. 10
When presenting, the patient may already be unable to communicate their symptoms and care preferences due to cognitive impairment and confusion. Also, there might be a physical difficulty in communication from severe rigidity. Care should be taken in considering the presence and consequent treatment of an intercurrent illness, and whether dopaminergic medication is exacerbating confusion due to hallucinations and/or psychosis.27
Continued attempts at verbal and non-verbal communication should be made throughout given the often fluctuating symptoms associated with PD and possible improvement in the intercurrent illness. In the absence of a next of kin or other person who is able to inform the clinical team, decisions should be made on a best interest basis as recommended in end of life care guidance.30
You May Like: How Long Does A Person Live With Parkinsons Disease
Recommended Reading: How To Improve Walking With Parkinson’s
End Stage Of Dementia
The end stage of dementia is the most difficult stage for those suffering from the disease, and also for family members, caregivers, and healthcare professionals. Victims lose what is left of their intellectual and physical capabilities and become completely dependent on others. The model is still shifting in considering end stage dementia an end of life condition experts are pushing this model in order to advocate for better pain and distress management for those suffering at their end.
Also Check: Parkinsons Fight Club The Villages Fl
