Theory Of Pd Progression: Braaks Hypothesis
The current theory is that the earliest signs of Parkinson’s are found in the enteric nervous system, the medulla and the olfactory bulb, which controls sense of smell. Under this theory, Parkinson’s only progresses to the substantia nigra and cortex over time.
This theory is increasingly borne out by evidence that non-motor symptoms, such as a loss of sense of smell , sleep disorders and constipation may precede the motor features of the disease by several years. For this reason, researchers are increasingly focused on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Ryan Barmore, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
*Please note that not all content is available in both languages. If you are interested in receiving Spanish communications, we recommend selecting both” to stay best informed on the Foundation’s work and the latest in PD news.
How Is Parkinsons Disease Dementia Diagnosed
No single test can diagnose Parkinsons disease dementia. Instead, doctors rely on a series or combination of tests and indicators.
Your neurologist will likely diagnose you with Parkinsons and then track your progression. They may monitor you for signs of dementia. As you get older, your risk for Parkinsons dementia increases.
Your doctor is more likely to conduct regular testing to monitor your cognitive functions, memory recall, and mental health.
Parkinsons Disease Symptoms Of Dementia
Up to one-third of people living with Parkinson’s disease experience dementia, according to the Parkinson’s Disease Foundation. Problems with dementia may include trouble with memory, attention span, and what is called executive function the process of making decisions, organizing, managing time, and setting priorities.
RELATED: 12 Famous People With Parkinson’s Disease
Don’t Miss: Is Parkinson’s Disease Fatal
Parkinson’s Progression Palliative And End Of Life Issues
This 38-minute webinar provides an overview of Parkinson’s symptoms, and treatment challenges due to disease progression. 18-minutes in the topic turns to planning a good death, the euphemisms even doctors use to avoid discussing death, the most common cause of death in those with PD, putting your end-of-life preferences in writing. Palliative care can help families face these end-of-life issues.
How To Manage Symptoms At The End Of Life
At the end of life, good practice is to plan for any potential symptoms that may arise. The most common symptoms anticipated are pain, dyspnoea, nausea and vomiting, agitation, anxiety, delirium and noisy respiratory secretions.18 For patients with PD particular considerations should be given to the more commonly used medicines, specifically anticholinergics and antidopaminergics. These are usually prescribed for treatment of respiratory secretions and nausea and vomiting. Alternatives are available for respiratory secretions, and include glycopyrronium, in preference to hyoscine hydrobromide. Although this is an anticholinergic, only a small proportion crosses the blood brain barrier.
For nausea and vomiting, ondansetron,19 cyclizine, domperidone have all been suggested in PD.20 However, ondansetron has been shown to be inferior to domperidone in the pre-treatment of apomorphine.21 Cyclizine has anticholinergic properties and may exacerbate confusion, especially when comorbid psychosis or cognitive impairment are present. Levomepromazine, although it has antidopaminergic effects, has been shown to be effective for nausea with rotigotine in a case report.22
Agitation, dyspnoea and pain can all be managed with the same anticipatory medications as recommended.20 Specifically relating to PD, several case reports have supported the intraoperative use of midazolam, during sedation, for tremor and dyskinesias,23,24 as well as for agitation at the end of life.20
Also Check: What Is The Life Expectancy Of Someone With Parkinson’s Disease
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
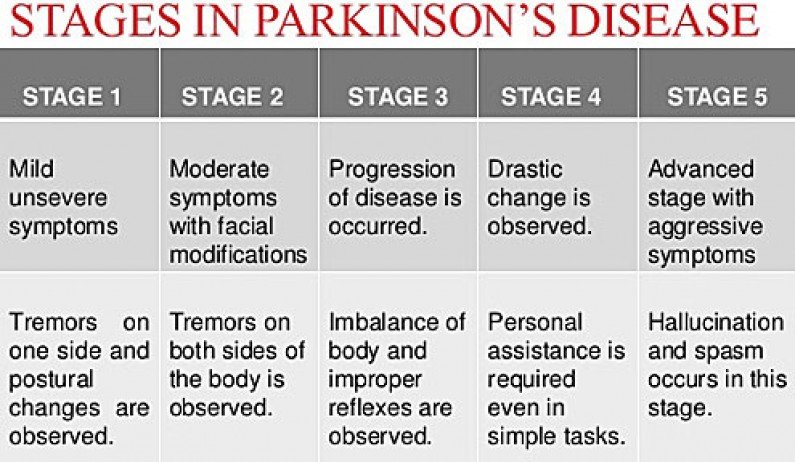
What Are The Stages Of Parkinsons
Doctors sometimes use five stages to describe the progress of Parkinsons disease. Each stage presents changing or new symptoms that a person is likely to encounter.
It is worth noting that not everyone will reach the advanced stages. For some people, the symptoms remain mild, and they can continue to live independently and be mobile.
Dividing the condition into stages helps doctors and caregivers understand and address some of the challenges a person is experiencing as it progresses.
Don’t Miss: Does Alice Waters Have Parkinson’s
What Are The Non
Parkinson’s disease stages are defined by the severity of a patient’s motor symptoms and how much those symptoms impact one’s ability to function every day. But there are non-motor symptoms that are more likely to develop later in the disease, too, and a doctor may take those into consideration when assessing someone with the disorder.
For example, people with late-stage Parkinson’s disease might have difficulty chewing, eating, speaking, or swallowing , which is considered both a motor and non-motor symptom. Dysphagia in particular can lead to serious health problems like malnutrition, dehydration, and aspiration.
In the final stages of Parkinson’s disease, a person might develop cognitive changes, including slowness of memory or thinking, trouble planning and accomplishing tasks, and difficulty concentrating. Or they might notice changes in their bone health or vision.
But there’s no telling for sure if or when these symptoms will occur in any individual because Parkinson’s disease symptoms vary from person to person.
Parkinson’s Disease Symptoms: Life Expectancy
Even though Parkinson’s disease is a serious, progressive condition, it is not considered a fatal illness. People who have Parkinson’s disease usually have the same average life expectancy as people without the disease.
But when the disease is in its advanced stages, Parkinson’s symptoms can lead to life-threatening complications, including:
- Falls that lead to fractured bones
- Pneumonia
- Choking
Thinking about the progression of Parkinson’s disease can be frightening. But proper treatments can help you live a full, productive life for years to come. And researchers hope to one day find ways to halt the progression of Parkinson’s and restore lost functioning.
Recommended Reading: Is Parkinson’s Deadly
Palliative Care In Parkinson’s Disease
In the absence of any curative treatment, the principles of palliative care should be applied throughout the course of the disease and not limited to the terminal end-of-life period. This chapter defines palliative care and discusses the palliative phase of Parkinson’s disease, palliative carers, care homes, social costs, withdrawl of drugs, pressure ulsers, end-of-life issues, recommendations and ethical issues.
Who Is Eligible For Hospice For Parkinsons Disease
An individual suffering from Parkinsons, whatever stage they may be, can avail of hospice services. Without assistance, it will be hard for both the individual and their family to help control and treat this disease.
For hospice eligibility, the individual must exhibit the following end-stage Parkinsons symptoms:
- Difficulty in breathing or dyspnea
- A constant need for a wheelchair or they are already bed-ridden
- Has pneumonia
- Inability to do daily activities without help
- Has speech deficiency
- Has eating problems
Also Check: Parkinsons And Leg Pain
What Are The Considerations For Pain Management In The Last Days Of Life In Pd
It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25 The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
How Is Parkinson’s Managed
There is currently no cure for Parkinsons but there are medications and therapies that can help to manage Parkinsons symptoms.
Medicines that increase the level of dopamine in the brain are the main treatment used to manage the symptoms of Parkinson’s. Medicines are tailored to each individuals needs.
Symptoms will get worse when someones Parkinsons medicines are wearing off and improve again after Parkinsons medicines are taken. If people with Parkinsons dont get their medication at the right time, it leads to their motor symptoms becoming uncontrolled. It can take some time to get their symptoms under control again. If you work in a hospital or care home, it is important to be aware that medicine timings will vary from person to person and may be different to ward medicine rounds.
As well as medicines, surgical options are available for some people with Parkinson’s, depending on their symptoms.
Treatments can help to manage the symptoms, but may become less effective in the later stages of the condition.
Parkinsons UK has more information on how Parkinsons affects people and how it can be managed.
Don’t Miss: Is Sugar Bad For Parkinson’s Disease
Is Parkinsons Disease Fatal
Parkinsons disease itself doesnt cause death. However, symptoms related to Parkinsons can be fatal. For example, injuries that occur because of a fall or problems associated with dementia can be fatal.
Some people with Parkinsons experience difficulty swallowing. This can lead to aspiration pneumonia. This condition is caused when foods, or other foreign objects, are inhaled into the lungs.
What Are The Important Points Regarding Duodopa At The End Of Life
Duodopa is a continuous infusion of dopaminergic medication administered as a gel into the gut, pumped via a percutaneously inserted gastrostomy tube . There is a requirement for care of the stoma and PEG tube together with functioning of the pump by the patient or carer.41 It reduces the time in motor off periods in advanced PD and quality of life.42 There is evidence of effective treatment up until death from within a case series.43
Recommended Reading: Are Weighted Blankets Good For Parkinson’s Patients
Caregiving In The Late Stages Of Parkinsons Disease
In late-stage PD, patients have significant mobility challenges. Caregivers likely need to provide more hands-on assistance to help them get around the house. Its important that caregivers learn safe and effective methods to provide help without injuring themselves. Physical therapists can be a great resource to assess an individual situation and teach effective ways of giving assistance.3
Freezing, a sudden but temporary inability to move, can become more common in late-stage PD. Freezing often happens when initiating movement or navigating around obstacles, and freezing episodes contribute to falls. Caregivers can help their loved one overcome freezing by providing a visual cue to step over, like a laser pointer, or using music or rhythm for the person with PD to walk to.3
Late stage PD can make daily activities, such as getting dressed, much more challenging. Caregivers can make getting dressed easier by ensuring adequate time to account for slow movement, choosing a time when medications are “on” and working well, and assembling all necessary items close to the person. Allowing the person with PD to do as much as they can gives them a sense of participation in the process.3
Lewy Body Dementia Vs Parkinsons Disease Dementia
Diagnoses of Lewy body dementia include dementia with Lewy bodies and Parkinsons disease dementia. Symptoms in both of these diagnoses can be similar.
Lewy body dementia is a progressive dementia caused by abnormal deposits of a protein called alpha-synuclein in the brain. Lewy bodies are also seen in Parkinsons disease.
The overlap in symptoms between Lewy body dementia and Parkinsons disease dementia include movement symptoms, rigid muscles, and problems with thinking and reasoning.
This seems to indicate that they could be linked to the same abnormalities, though more research is needed to confirm that.
The later stages of Parkinsons disease have more severe symptoms that may require help moving around, around-the-clock care, or a wheelchair. Quality of life can decline rapidly.
Risks of infection, incontinence, pneumonia, falls, insomnia, and choking increase.
Hospice care, memory care, home health aides, social workers, and support counselors can be a help in later stages.
Parkinsons disease itself isnt fatal, but complications can be.
Research has shown a median survival rate of about
Also Check: What Are Early Warning Signs Of Parkinson’s Disease
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
My Parkinson’s Story: Advanced Parkinsons
This 10-minute video alternates between an interview with a man and his wife and his palliative care team, including a doctor, nurse, clerg and social worker. The man and his wife shares his experience with late stage Parkinson’s. The palliative care team explains that their job is to support the best physical, emotional and spiritual wellbeing of the immediate family as well as help the family make end of life decisions.
Also Check: Can Parkinson’s Run In The Family
Stage Two: Symptoms Begin Affecting Movement On Both Sides Of Your Body
Once the motor symptoms of Parkinsons disease are affecting both sides of the body, you have progressed to Stage Two. You may begin having trouble walking and maintaining your balance while standing. You may also begin noticing increasing difficulty with performing once-easy physical tasks, such as cleaning, dressing, or bathing. Still, most patients in this stage lead normal lives with little interference from the disease.
During this stage of the disease, you may begin taking medication. The most common first treatment for Parkinsons disease is dopamine agonists. This medication activates dopamine receptors, which make the neurotransmitters move more easily.
What Are The Symptoms Of Parkinson’s

The main motor symptoms of Parkinsons are:
- tremor
- slowness of movement
- problems with balance.
However, the condition doesnt only affect movement. People living with the condition can experience a range of non-motor symptoms that can often have a greater impact on their lives than movement difficulties.
Non-motor symptoms include:
- urinary urgency, frequency
- pain.
These non-motor symptoms are present at all stages of the condition but they can become more severe in the later stages of Parkinsons and have a major impact on quality of life.
Parkinsons gets worse over time and it can be difficult to predict how quickly the condition will progress. For most people, it can take years for the condition to progress to a point where it can cause major problems. For others, Parkinsons may progress more quickly.
Read Also: How To Take Mannitol For Parkinson’s
Is Parkinsons Disease Inherited
Scientists have discovered gene mutations that are associated with Parkinsons disease.
There is some belief that some cases of early-onset Parkinsons disease disease starting before age 50 may be inherited. Scientists identified a gene mutation in people with Parkinsons disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinsons disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinsons disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinsons disease.
Scientists think that about 10% to 15% of persons with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
