What Tests Will Be Done To Diagnose This Condition
When healthcare providers suspect Parkinsons disease or need to rule out other conditions, various imaging and diagnostic tests are possible. These include:
New lab tests are possible
Researchers have found possible ways to test for possible indicators or Parkinsons disease. Both of these new tests involve the alpha-synuclein protein but test for it in new, unusual ways. While these tests cant tell you what conditions you have because of misfolded alpha-synuclein proteins, that information can still help your provider make a diagnosis.
The two tests use the following methods.
- Spinal tap. One of these tests looks for misfolded alpha-synuclein proteins in cerebrospinal fluid, which is the fluid that surrounds your brain and spinal cord. This test involves a spinal tap , where a healthcare provider inserts a needle into your spinal canal to collect some cerebrospinal fluid for testing.
- Skin biopsy. Another possible test involves a biopsy of surface nerve tissue. A biopsy includes collecting a small sample of your skin, including the nerves in the skin. The samples come from a spot on your back and two spots on your leg. Analyzing the samples can help determine if your alpha-synuclein has a certain kind of malfunction that could increase the risk of developing Parkinsons disease.
Problems With Balance Or Walking
Bradykinesia can also contribute to increasing instability, walking difficulties and changes in gait. An early symptom of this is a decrease in the natural swing of one or both arms when walking. As things progress, the steps you take may become slower and smaller, and you may start shuffling your feet.
Some people with Parkinsons disease may also experience freezing episodes where it can feel like their feet are stuck in place, which can increase the risk of falling.
Incidence Of Hospitalized Cases Of Parkinsons Disease
The incidence rate of PD was 13.3 per 100,000 person-years in all hospitalized participants , but incidence rate varied by age, sex, and region. The incidence rate increased with age from 1.6 per 100,000 person-years in those aged â¤50 years at baseline, to 48.8 per 100,000 person-years for participants over 70 years of age at baseline. PD incidence rates were higher in men than in women . Similarly, PD incidence rates were slightly higher in urban than in rural regions .
| Variable |
|---|
Sensitivity analyses excluding the first 3 years of follow-up did not alter the observed associations of smoking, obesity, hypertension, and diabetes with PD. However, sensitivity analysis revealed a higher risk of PD for overweight or obese vs. nonoverweight or obese participants . Analyses of overweight or obesity with PD in the subset of never smokers after adjustment for confounders and by exclusion of the first 3 years of follow-up were unaltered. Assuming overweight or obesity status is causal for an increased risk of PD, population attributable fractions based on the fully adjusted HR indicate that overweight or obesity accounted for approximately 7.9% of all hospitalized cases of PD.
You May Like: Can Parkinsons Symptoms Be Something Else
Recommended Reading: How Do You Spell Parkinson’s
How Is It Treated And Is There A Cure
For now, Parkinsons disease is not curable, but there are multiple ways to manage its symptoms. The treatments can also vary from person to person, depending on their specific symptoms and how well certain treatments work. Medications are the primary way to treat this condition.
A secondary treatment option is a surgery to implant a device that will deliver a mild electrical current to part of your brain . There are also some experimental options, such as stem cell-based treatments, but their availability often varies, and many aren’t an option for people with Parkinsons disease.
Medicines For Parkinsons Disease
Medicines can help treat the symptoms of Parkinsons by:
- Increasing the level of dopamine in the brain
- Having an effect on other brain chemicals, such as neurotransmitters, which transfer information between brain cells
- Helping control non-movement symptoms
The main therapy for Parkinsons is levodopa. Nerve cells use levodopa to make dopamine to replenish the brains dwindling supply. Usually, people take levodopa along with another medication called carbidopa. Carbidopa prevents or reduces some of the side effects of levodopa therapy such as nausea, vomiting, low blood pressure, and restlessness and reduces the amount of levodopa needed to improve symptoms.
People living with Parkinsons disease should never stop taking levodopa without telling their doctor. Suddenly stopping the drug may have serious side effects, like being unable to move or having difficulty breathing.
The doctor may prescribe other medicines to treat Parkinsons symptoms, including:
- Dopamine agonists to stimulate the production of dopamine in the brain
- Enzyme inhibitors to increase the amount of dopamine by slowing down the enzymes that break down dopamine in the brain
- Amantadine to help reduce involuntary movements
- Anticholinergic drugs to reduce tremors and muscle rigidity
Don’t Miss: Vitamins And Herbs For Parkinson’s Disease
Standard Treatments Are Being Tweaked
Since the late 1960s, levodopa has been the most effective treatment for addressing motor symptoms of Parkinsons disease. The problem for some patients, however, is levodopa does not provide the constant flow of dopamine necessary for smooth function throughout the day.
Patients symptoms may be well-controlled, and they may function well while the medication is working, but as the medications wear off, the symptoms return, Witek says. It is hard to live a normal life when facing this unpredictability.
New research is focused on developing treatments that will give people a more steady flow of dopamine and decrease fluctuations.
One common side effect of not having steady levels of dopamine is dyskinesia .
Dopamine Dopamine Receptor And Dopamine Transporter Activity
A catecholamine neurotransmitter dopamine is secreted by the SN, hypothalamus and some other regions of the brain. TH synthesizes the dopamine precursor that is converted to dopamine by L-aromatic amino acid decarboxylase . In the brain, dopamine is used as the precursor of noradrenaline and adrenaline . Loss of dopaminergic neurons in the midbrain and SN of PD brains leads to the reduction of dopamine levels . The dopamine transporter controls dopamine levels by facilitating its reuptake back to the cytosol. However, free dopamine is toxic for neurons, since its oxidation creates poisonous reactive quinones. Therefore, the vesicular monoamine transporter 2 stores excess dopamine in vesicles. Thus, any change in dopamine or DAT levels may be an indicator of PD. Moreover, dopamine activates five types of receptors and the severity of PD is related to the decreased expression of the dopamine type 3 receptor , leading to more severe symptoms because of reduced dopamine signals . Therefore, D3R can be also considered as a potential biomarker for PD .
In another recent article a preclinical phase of PD is identified by analysis of dopamine metabolites in CSF. Low CSF concentrations of 3,4-dihydroxyphenylacetic acid and DOPA identify pre-clinical PD in at-risk healthy individuals .
Also Check: Parkinson’s Lewy Body Dementia Life Expectancy
Managing Your Mood Is Crucial
Living with a chronic, progressive disease can take a serious emotional toll on patients and their loved ones. Depression and anxiety are common symptoms of Parkinsons disease, with up to 60% of people who have the disease experiencing mild or moderate depressive symptoms.
Depression can diminish quality of life for people with Parkinsons disease, Witek says. Often providers focus on the most apparent symptoms, such as tremor or walking problems, but if we do not improve their mood, then we will not improve their quality of life.
Some patients benefit from psychological counseling, cognitive-behavioral therapy, and/or taking medications to help improve their mood. Support groups such as the group hosted by Rush Oak Park Hospital the second Saturday of each month can also help people with Parkinsons disease learn how to live changed, yet still full lives.
We work with our patients to find medications and other therapies that will improve their quality of life at every stage of the disease, targeting the symptoms that matter most to them and their families,Witek says.
Dont Miss: Stretching Exercises For Parkinsons Patients
Impact On Families And Carers
Informal carers spendmany hours dailyproviding care for people living with PD.This can be overwhelming. Physical, emotional and financial pressures can cause great stress to families and carers, and support is required from the health, social, financial and legal systems. Useful support resources from other conditions can be drawn upon, such as WHOs iSupport programme for dementia.
Recommended Reading: What Are The Non Motor Symptoms Of Parkinson’s Disease
Genetic And Environmental Interactions
Although several genetic mutations have been identified to be associated with a higher risk of developing Parkinson’s disease most people do not have these genetic variations.
On the other hand, even though pesticides and head traumas are associated with PD, most people do not have any obvious exposure to these environmental factors.
Parkinson’s is caused by a combination of genes, environmental and lifestyle influences. The interaction of all three components determines if someone will develop Parkinson’s. Parkinsons-specific research is critical to better understanding how these components interact to cause PD and how to prevent it.
Page reviewed by Dr. Lauren Fanty, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
How Do I Take Care Of Myself
If you have Parkinsons disease, the best thing you can do is follow the guidance of your healthcare provider on how to take care of yourself.
- Take your medication as prescribed. Taking your medications can make a huge difference in the symptoms of Parkinsons disease. You should take your medications as prescribed and talk to your provider if you notice side effects or start to feel like your medications arent as effective.
- See your provider as recommended. Your healthcare provider will set up a schedule for you to see them. These visits are especially important to help with managing your conditions and finding the right medications and dosages.
- Dont ignore or avoid symptoms. Parkinsons disease can cause a wide range of symptoms, many of which are treatable by treating the condition or the symptoms themselves. Treatment can make a major difference in keeping symptoms from having worse effects.
Read Also: Is Parkinson’s An Autoimmune Disease
Caffeine And Other Methylxanthines
There is controversy in almost any potential risk factor. For instance, despite previous works providing evidence on negative correlation between coffee consumption and PD risk , we have been unable to find similar results in a case-control study. On the one hand, there is a consensus that there are compounds in coffee that can afford protection, such as caffeine and similar methylxanthines, which block adenosine receptors. On the other hand, the consumption of caffeine is not easy to asses due to differences in caffeine content in coffee, to inter-country differences in the style/amount of drinking coffee/tea, and to the fact that caffeinated drinks must be also considered in the risk analysis. Overall, the evidence stands up. In the exhaustive meta-analysis of Noyce et al. , a significant negative association between coffee drinking and PD risk is confirmed. More information on the validity of this negative association can be found in more recent reviews .
Read Also: What Happens To You When You Have Parkinsons Disease
Leading Possible Risk Factors For Parkinsons
Genetic factors
Scientists estimate that less than 10% of cases of Parkinsons disease are primarily due to genetic causes. The most common genetic effect that triggers Parkinsons disease is mutation in a gene called LRRK2. The LRRK2 defect is particularly frequent in families of North African or Jewish descent. Mutations in alpha-synuclein have also been found to trigger Parkinsons, but these are quite rare. In most cases, no primary genetic cause can be found.
Other risk factors
There are other things that put an individual at higher risk for developing Parkinsons. The main risk factor is age, because Parkinsons disease is most commonly found in adults over the age of 50 . Men also have a higher risk of Parkinsons disease than women. The actual links between any of these factors and Parkinsons disease are not completely understood.
Read Also: How To Delay Parkinson’s Disease
Causes Of Parkinsons Disease And Risk Factors
Parkinsons disease is caused by low dopamine activity in certain areas of the brain. Its associated with degeneration of the substantia nigra, a small area of the brain that produces dopamine, a neurotransmitter that mediates motor movements and other body functions.
The underlying cause or trigger for these changes is not known, although some people have a family history of the condition.
Many potential risk factors have been examined as possible triggers, including exposure to chemicals, but no environmental or lifestyle factors have been confirmed as causing Parkinsons disease.
Comparing Risk Factors Of Incident Pd And Ischemic Stroke
The comparisons of risk factors for PD and ischemic stroke are presented in Table and Fig. . Female sex was more protective for PD when compared with ischemic stroke . Smoking was positively associated with risk of ischemic stroke but was inversely associated with risk of PD . Age, diabetes, NLR, and FBG were the shared risk factors in PD and ischemic stroke , whereas HDL was a common protective factor for the two outcomes . In addition, hypertension was positively associated with the risk of ischemic stroke but was not significantly associated with the risk of PD . In contrast, LDL was inversely associated with the risk of PD but was not significantly associated with the risk of ischemic stroke .
In sensitivity analyses, similar results were observed when excluding those who developed both PD and coronary events or ischemic stroke during the follow-up .
You May Like: How To Get Checked For Parkinson’s Disease
Symptoms Of Parkinsons Disease
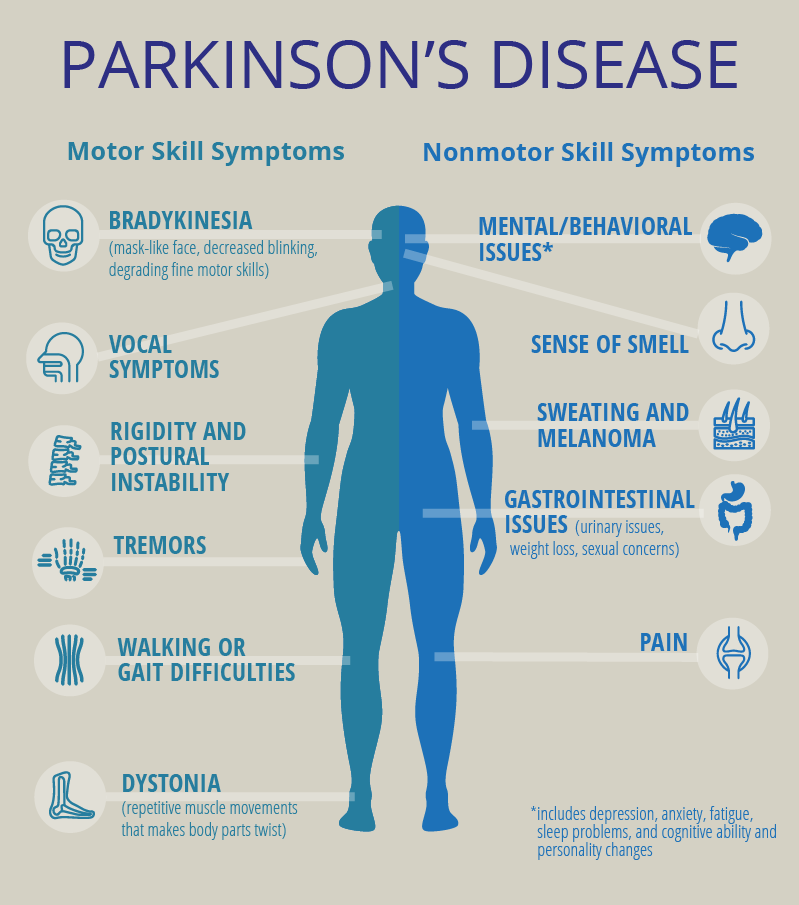
Parkinsons has four main symptoms:
- Tremor in hands, arms, legs, jaw, or head
- Muscle stiffness, where muscle remains contracted for a long time
- Slowness of movement
- Impaired balance and coordination, sometimes leading to falls
Other symptoms may include:
The symptoms of Parkinsons and the rate of progression differ among individuals. Early symptoms of this disease are subtle and occur gradually. For example, people may feel mild tremors or have difficulty getting out of a chair. They may notice that they speak too softly, or that their handwriting is slow and looks cramped or small. Friends or family members may be the first to notice changes in someone with early Parkinsons. They may see that the persons face lacks expression and animation, or that the person does not move an arm or leg normally.
People with Parkinson’s disease often develop a parkinsonian gait that includes a tendency to lean forward take small, quick steps and reduce swinging their arms. They also may have trouble initiating or continuing movement.
Symptoms often begin on one side of the body or even in one limb on one side of the body. As the disease progresses, it eventually affects both sides. However, the symptoms may still be more severe on one side than on the other.
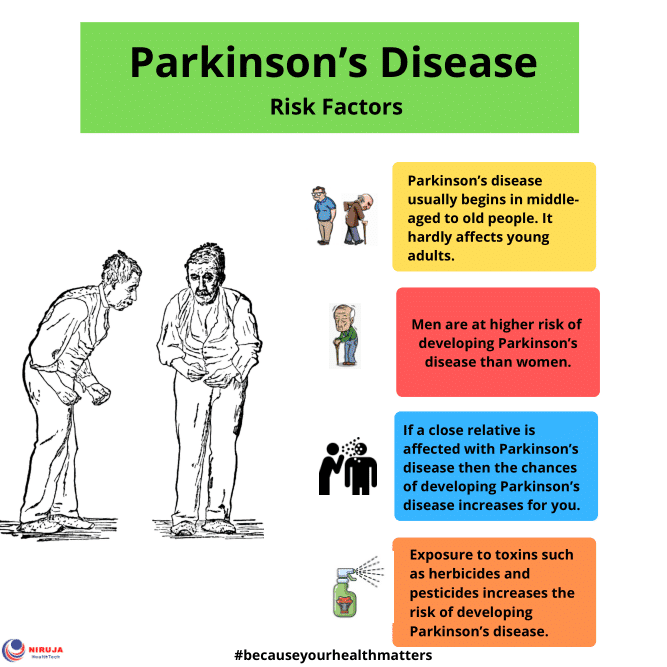
Parkinson’s Disease Risk Factors
Although a primary cause for Parkinson’s disease is yet to be identified, a number of risk factors are clearly evident.
Advancing age– Although there is the occasional case of the disease being developed as a young adult, it generally manifests itself in the middle to late years of life. The risk continues to increase the older one gets. Some researchers assume that people with Parkinson’s have neural damage from genetic or environmental factors that get worse as they age.
Sex- Males are more likely to get Parkinson’s than females. Possible reasons for this may be that males have greater exposure to other risk factors such as toxin exposure or head trauma. It has been theorised that oestrogen may have neuro-protective effects. Or, in the case of genetic predisposition, a gene predisposing someone to Parkinson’s may be linked to the X chromosome.
Family history– Having one or more close relatives with the disease increases the likelihood that you will get it, but to a minimal degree. This lends support to the idea that there is a genetic link in developing Parkinson’s.
– Post menopausal who do not use hormone replacement therapy are at greater risk, as are those who have had hysterectomies.
Low levels of B vitamin folate– Researchers discovered that mice with a deficiency of this vitamin developed severe Parkinson’s symptoms, while those with normal levels did not.
2002-2012©Parkinson’s Disease Information.
Don’t Miss: Michael J Fox Foundation Parkinson’s 360
What Else Do We Know
As scientists try to learn what’s at the root of Parkinson’s, they’re looking far and wide to pick up clues where they can.
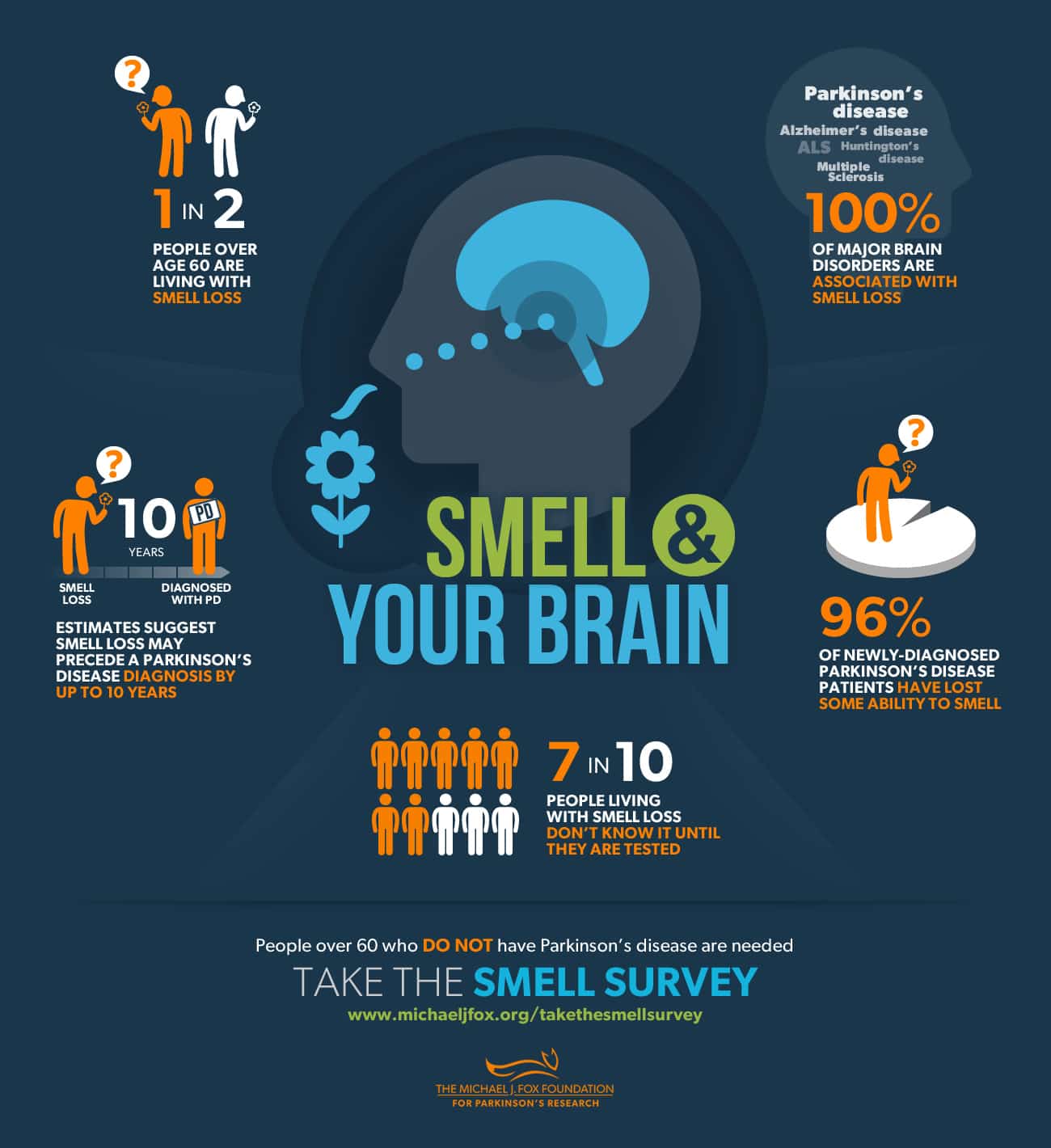
They’ve found that people with Parkinson’s tend to have something called Lewy bodies in their brain. These are unusual clumps of a protein called alpha-synuclein. The protein itself is normal, but the clumps are not. And they’re found in parts of the brain that affect sleep and sense of smell, which could explain some symptoms of Parkinson’s not related to movement.
Your gut may also have a part in it, as some of its cells make dopamine, too. Some doctors think that this might be where the earliest signs of Parkinson’s show up, but that idea needs more research.
Show Sources
What Can I Expect If I Have This Condition
Parkinsons disease is a degenerative condition, meaning the effects on your brain get worse over time. However, this condition usually takes time to get worse. Most people have a normal life span with this condition.
Youll need little to no help in the earlier stages and can keep living independently. As the effects worsen, youll need medication to limit how the symptoms affect you. Most medications, especially levodopa, are moderately or even very effective once your provider finds the minimum dose you need to treat your symptoms.
Most of the effects and symptoms are manageable with treatment, but the treatments become less effective and more complicated over time. Living independently will also become more and more difficult as the disease worsens.
How long does Parkinsons disease last?
Parkinsons disease isnt curable, which means its a permanent, life-long condition.
Whats the outlook for Parkinsons disease?
Parkinsons disease isnt fatal, but the symptoms and effects are often contributing factors to death. The average life expectancy for Parkinsons disease in 1967 was a little under 10 years. Since then, the average life expectancy has increased by about 55%, rising to more than 14.5 years. That, combined with the fact that Parkinsons diagnosis is much more likely after age 60, means this condition doesnt often affect your life expectancy by more than a few years .
Also Check: Parkinson’s And Panic Attacks