Clinical Features Of Insomnia
Insomnia is defined as difficulties initiating sleep , sleep maintenance problem or early awakening . In studies, it has been reported that the frequency of insomnia in patients with PD varies from 27 to 80% . It has been reported that the most common types of insomnia in PD patients are sleep fragmentation , and early awakenings . It has been reported that insomnia may occur alone or accompany comorbid mental or systemic illnesses, and it is associated with disease duration and female gender . Sleep fragmentation is defined as a deterioration of sleep integrity , and it leads to a lighter sleep or wakefulness . In studies, it has been reported that sleep fragmentation is the most common sleep disorder in patients with PD .
Parkinsons Disease Linked To Sleep Disorders Sleep Disturbances
Written byDevon AndrePublished onFebruary 9, 2016
Parkinsons disease has been linked to sleep disorders and sleep disturbances. Parkinsons disease is characterized;by the loss of brain cells that control movement. Symptoms of Parkinsons disease can include tremors, stiffness, slowness of movements, as well as balance and coordination problems. Memory problems, depression, and sleep problems can all occur in Parkinsons disease, too.
Sleep problems and sleep disorders may occur as an early sign of Parkinsons disease, even before motor symptoms have started. Common sleep disorders experienced in Parkinsons disease include insomnia, excessive daytime sleepiness, nightmares, sleep attacks, REM sleep behavior disorder , periodic leg movement disorder, restless leg syndrome, sleep apnea, and nocturia, which is frequent nighttime urination.
Identifying Sleep Apnea In Someone With Parkinson’s
We already know that PD is linked to the parasomnia known as REM sleep behavior disorder .
If a person with PD presents symptoms that resemble sleepwalking, they are urged to have an overnight test in a sleep lab. Not only is this important for treating RBD, but research suggests that, in severe OSA, its symptoms may mimic those in RBD .
Nocturnal polysomnography , more commonly referred to as an overnight sleep study, is the gold standard diagnostic assessment used to identify OSA.
If someone with PD is diagnosed with OSA, the go-to treatment is a form of noninvasive ventilation, usually along the line of therapies known as PAP, or positive airway pressure. Current research continues to support the long-term use of PAP therapy to treat OSA in people with PD. Kaminska et al found that PAP therapies improved the overall non-motor symptom burden of PD .
Also Check: Essential Oils And Parkinson’s
The Critical Difference Between Sleepiness And Fatigue
Fatigue is a physical or psychological feeling where people feel weary and exhausted and lacking energy. EDS is about needing and having the urge to sleep.
Fatigue is something that people can experience along with EDS; however, people who experience fatigue on its ownthe feeling of being tired and out of energy do not also necessarily fall asleep when sedentary, as people who experience EDS often do.
It is estimated that EDS affects up to 50% to 75% of people living with Parkinsons and fatigue is estimated to affect 40% to 60%. Fatigue, however, is more likely to go undiagnosed.
Because the terms fatigue and sleepiness are so heavily linked, and sometimes used interchangeably, research has concluded that fatigue and EDS should be assessed separately in people with Parkinsons so that we can improve our understanding of their overlapping physiology.
With that knowledge, researchers from the University Hospital of Zurich, Switzerland designed a study to determine the overlap between fatigue and EDS and then associate them with other motor and non-motor symptoms as well as dopaminergic medication.
In their study of 88 outpatients, the researchers found that 72% experienced fatigue or EDS and just under half experienced both. Some of the key findings of the study include:
Sudden Onset Of Sleep And Eds
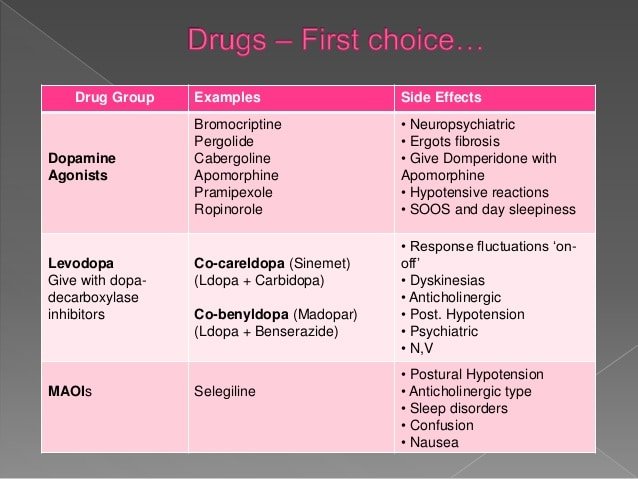
Sudden onset of sleep may warrant other measures, and those with high sleepiness scores should be advised to drive cautiously and not to drive alone or for long distances . Dopamine agonists when started should be titrated up slowly especially in older patients, and patients with excessive day-time sleepiness may respond to an alternative agonist. In patients with severe EDS, concurrent medications that may be sedating should be eliminated or reduced. Formal sleep studies may be required in some patients, and in those with a narcolepsy-like phenotype, modafinil may be useful. Modafinil, a sleepwake cycle activator, is non-stimulating and is the only drug which has shown efficacy in improving EDS without detrimental effect on PD when examined in double-blind placebo-controlled trials . A 7-week double-blind placebo crossover study of 200 mg modafinil followed by a 4-week open-label extension study by Adler et al. showed significant improvement in ESS with modafinil and improvement in clinical global impression scores for wakefulness in the open-label arm. Where EDS is thought to be secondary to the use of dopamine agonists, modafinil may allow the continuation of dopamine agonist therapy.
Recommended Reading: Does Diet Soda Cause Parkinson’s
Whats The Relationship Between Parkinsons And Sleep
Parkinsons disease and sleep are connected in complex ways that not even scientists completely understand quite yet.
Sometimes, Parkinsons disease directly causes sleep problems. According to one study, sleep-related symptoms may be one of the earliest signs of Parkinsons disease. These signs may include things like thrashing while youre asleep.
Other factors can also play a role. One thing is clear: For many people with Parkinsons disease, a restful nights sleep can be hard to find.
Sleep And Depression In Parkinson’s Disease
Depression;is seen in approximately 40% of PD patients in the course of their disease. Most persons with depression, including PD patients, also will experience problems with sleep. In depression, sleep does not refresh you like it used to, or you wake up too early in the morning. Dreams for depressed people are different, too–they are rare and often depict a single image.
Read Also: Parkinson Disease Autosomal Dominant
Changes In Sleep With Aging
As people age, they experience a number of changes in their circadian rhythms, and among the most noticeable are the changes in the sleep-wake cycle.; Older people tend to wake up earlier and go to bed earlier than they did when they were younger. ;They wake up more often during the night and have more difficulty going back to sleep than younger people.; They also tend to sleep more during the daytime hours.; Therefore, if one looks at total sleep time over the 24-hour day, the total time spent sleeping changes very little but the distribution of sleep may be quite different.; Younger people experience a consolidated nighttime episode with little or no daytime sleep, whereas older individuals experience sleep episodes throughout the 24-hour day.; Daytime sleepiness is affected by two major factors:; the amount and quality of nighttime sleep, and the strength of the circadian rhythm.; In addition, older people tend to have a reduced amount of N3 or deep slow wave sleep.
Here Are Some Sleep Hygiene Tips:
- Be mindful;of what you eat for dinner. High-protein foods may interfere with the absorption of medications for Parkinsons . This may make the medication wear off prematurely, causing symptoms to return in the night.
- High-protein foods, particularly meat and dairy, also take longer to digest. This could lead to reflux and other issues that could interfere with sleep.
- Reduce liquids a couple of hours before bed to try to reduce the number of times you need to get up in the night to use the toilet.
- Although regular exercise is associated with better sleep quality, its important to avoid strenuous activity too late in the evening as it may increase alertness and interfere with sleep.
- Avoid sources of blue light.
- Computers, tablets, smartphones and televisions emit light in the same spectrum associated with daylight . Spending time with these blue-light sources in the evening can sometimes fool your sensory system, tricking the brain into thinking that it is daytime and making it harder to fall asleep.
Also Check: Can Parkinson’s Run In The Family
Study Population And The Distribution Of Different Types Of Sleep Disorders
A total of 1006 patients with PD were enrolled in the study. The mean PD disease duration was 5.54±4.58 years. The mean modified HoehnYahr stage was 2.17±0.84 . The Unified Parkinsons Disease Rating Scale parts I, II, III, and IV scores were 3.06±2.82, 12.41±8.44, 25.50±15.51, and 3.20±3.66, respectively. Of the total cohort, 920 patients were taking levodopa, 563 were taking dopamine agonists, 39 were taking a MAO-B inhibitor, and 173 were taking a COMT inhibitor. Complete demographic data for the entire cohort are shown in Table .
Table 1 Characteristics of study participants classified by sleep disorders.
Hallucinations And Rem Sleep Disorders In Parkinson’s Disease
At timestamp 1:58 in this recording of Thrive: HAPS 2020 Caregiver Conference, you will find a one hour talk by neurologist;Joohi Jimenez-Shahed, MD.; In it she delves into what REM sleep behavior disorder is and is not, and the distinctions between hallucinations, delusions, and delirium.; Managment options for RBD and hallucinations are included.
You May Like: What Is The Life Expectancy Of Someone With Parkinson’s Disease
How Is Daytime Sleepiness Treated
Consider making certain lifestyle modifications, such as:
- Establish good sleep hygiene, including a set bedtime and wake-up time.
- Get exposure to adequate light during the day and darkness at night.
- Remember indoor lighting may not be sufficient to promote a normal circadian rhythm.
- Avoid sedentary activities during the day.
- Participate in activities outside the home. They may help provide stimulation to prevent daytime dozing.
- Get physical exercise appropriate to your level of functioning, which may also promote daytime wakefulness. Strenuous exercise, however, should be avoided six hours before sleep.
- Do NOT drive while sleepy if you experience excessive daytime sleepiness. Motor vehicle accidents increase during periods of drowsiness and may be associated with sudden onset of sleep .
- Talk to your doctor about possibly decreasing the dosage of dopamine agonists if you experience daytime sleepiness or sleep attacks.
- Talk to your doctor about decreasing stimulants like caffeine, modafinil and methylphenidate .
Sleep Disorders In Parkinson’s Disease By Amer G Aboukasm
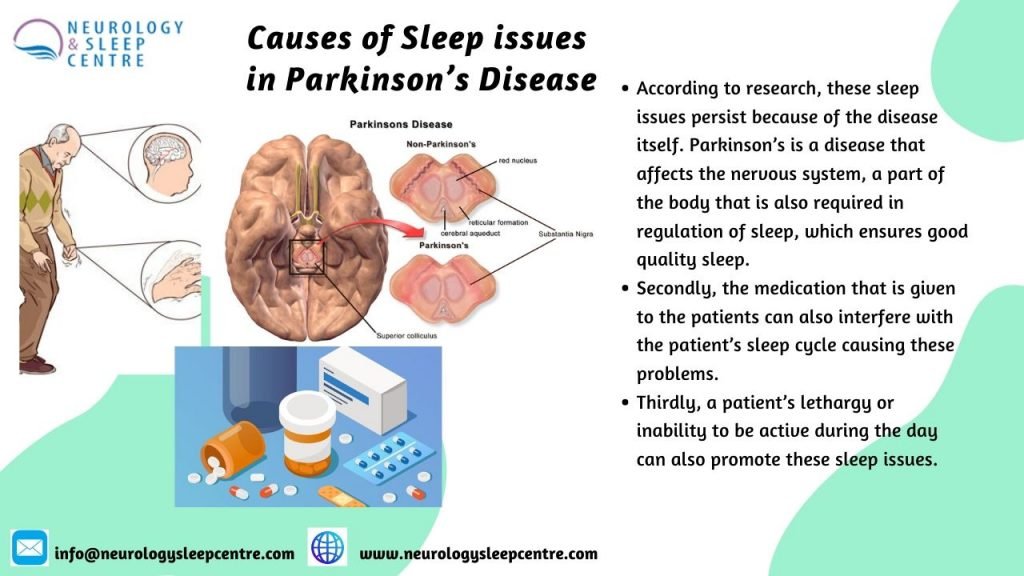
Although the daytime clinical manifestation of Parkinson’s disease have been well recognized for almost two centuries, the nocturnal symptoms, which occur in as many as 75% of patients and the associated sleep disorders were not studied until the 1960s. A variety of psychological and physiological processes can lead to disruption of the normal rhythm of the sleep-wake cycle in patients with Parkinsonism. First, the degenerative process in Parkinson’s disease affects the neurophysiological and neurochemical systems responsible for sleep organization, thus results in disruption of sleep. Second, the motor, respiratory and behavioral phenomena accompanying the disease may produce nocturnal symptoms. Third, the medication used in its treatment may induce new symptoms, such as nightmares or nocturnal movements. All these effects on sleep have implications for treatment planning.
Read Also: Parkinsons Disease Gene
Sleep Problems At Later Stages Of Pd
In addition to the conditions already mentioned, during the later stages of PD, you also may experience sleep problems related to higher doses of medications, such as;hallucinations.
As many as 33% of Parkinson’s patients during mid and later stages of the disorder experience hallucinations, related to medication side effects. Hallucinations tend to occur visually rather than hearing them . They are frequently associated with vivid dreams.
- Cartwright, R. . Dreaming as a mood regulation system. In: Principles and Practice of Sleep medicine. 4th edition, ; pps 565-572.
- Kumar, S., Bhatia, M., &;Behari, M. . Sleep disorders in Parkinson’s disease.;Mov Disord, 17, 775-781.
- Larsen, J. P., & Tandberg, E. . Sleep disorders in patients with Parkinson’s disease: epidemiology and management.;CNS Drugs, 15, 267-275.
- Olson, E. J., Boeve, B. F., & Silber, M. H. . Rapid eye movement sleep behaviour disorder: demographic, clinical and laboratory findings in 93 cases.;Brain, 123 ,;331-339.
- Pappert, E. J., Goetz, C. G., Niederman, F. G., Raman, R., & Leurgans, S. . Hallucinations, sleep fragmentation, and altered dream phenomena in Parkinson’s disease.;Mov Disord, 14, 117-121.
- Stacy, M. . Sleep disorders in Parkinson’s disease: epidemiology and management.;Drugs Aging, 19, 733-739.
Why Do Parkinsons Patients Have Trouble Sleeping
Despite having daytime tremors, Parkinsons patients do not shake in their sleep. However, both Parkinsons disease itself and the medications used to treat it can give rise to a number of sleep problems that lead to insomnia and excessive daytime sleepiness.
Patients with motor symptoms may have trouble adjusting sleeping positions to get comfortable.; Others may experience distressing nocturnal hallucinations when trying to fall asleep. These may be a result of medications or cognitive impairment.
In turn, excessive daytime sleepiness may occur as a consequence of sleeping poorly at night. It may also be triggered by medications. Parkinsons patients who suffer from EDS may be at a higher risk of accidents and unable to safely carry out activities such as operating a motor vehicle.
Since insomnia frequently goes hand-in-hand with anxiety and depression, it may be a contributing factor to sleep problems in people with Parkinsons disease. For that reason, doctors often look for mental health disorders in people with Parkinsons disease who have sleep problems.
Don’t Miss: Can Parkinson’s Run In The Family
Sleep Attacks And Medication Side Effects
In the last 10 years, the phenomena of sleep attacks in PD, defined as an event of falling asleep suddenly, unexpectedly and irresistibly while engaged in some activity have received a great deal of attention.
Compared to levodopa, the ergot agonists and non-ergot D2-D3 dopamine agonists show an increased risk of daytime sleepiness and episodes of unintended sleep . With the exception of a dose-related effect, levodopa is generally not sedating in PD or DLB . In a sample of 6,620 PD respondents to a questionnaire, 42.9% reported the sudden onset of sleep that was predicted by exposure to a non-ergot dopamine agonist . Factors contributing to sleepiness with dopamine agonists include older age, male gender, history of sleep problems, cognitive impairment, dysautonomia and an overall higher dopaminergic load . Unlike levodopa, the ergot and non-ergot dopamine agonists are more likely to aggravate cognitive impairment and may elicit or intensify hallucinations .
Polysomnography data reveal that sleep attacks are objectively characterized as intrusions of non-REM stage 1 and 2 sleep, and a subset are represented by microsleep episodes, which last 15-120 s . Whether sleep attacks are truly abrupt and occur in the absence of a history of sleep disturbance is a point of contention, particularly since patients often have reduced awareness of daytime sleepiness and microsleep episodes are often not perceived by patients .
How Does Parkinsons Disease Cause Sleep Problems
Researchers have yet to uncover every nuance of the Parkinsons and sleep connection. So far, medical experts believe several causes may contribute:
- Chemical changes in the brain: Ongoing research shows that Parkinsons disease may disrupt sleep-wake cycles. Changes to certain brain chemicals may cause people with Parkinsons to get less sleep.
- Medication: Some drugs that treat Parkinsons disease may make it harder to fall or stay asleep. A medication may also disrupt your sleep patterns by making you drowsy during the day .
- Mental health challenges: People with Parkinsons commonly deal with mood disorders, such as anxiety or depression. Any mood disorder may keep you up at night or make you sleep less soundly.
- Parkinsons symptoms: Pain, waking up at night to pee or other Parkinsons symptoms can make restful sleep harder to come by. Sleep apnea can also disrupt sleep.
Read Also: Can Parkinson’s Cause Hip Pain
Polysomnography And Multiple Sleep Latency Tests
In PD, overnight sleep studies using polysomnography reveal increased sleep fragmentation and a reduction in total sleep time, slow wave sleep and lower sleep efficiency . Although nocturia, dyskinesia, dystonia, parkinsonism severity, and wearing off phenomena may fragment night-time sleep and result in daytime sleepiness, these factors do not entirely account for reduced sleep efficiency or daytime sleepiness . We found a similar pattern in a cohort of 78 DLB patients in the early and middle stages of DLB, and 50% of the sample had sleep efficiency less than 70%. Although about half the sample met criteria for obstructive sleep apnea or periodic limb movements of sleep , 76% of the sample had five or more spontaneous arousals an hour, not accounted for by respiratory or motor issues. This suggests that a component of the sleep fragmentation in DLB may have a primary neurologic basis.
We carried out polysomnography and daytime MSLT in 31 DLB and 16 AD patients matched for gender and mild to moderate dementia . Results revealed both groups had a mean night-time sleep efficiency of 70%, but the DLB group was more likely to fall asleep on the MSLT, and those that did fall asleep, did so faster than the AD group. Specifically, mean ISL <10 min occurred in 81% of DLB vs. 44% of AD , and mean ISL <6 min occurred in 61% of DLB versus 19% of AD . These data are similar to the studies of PD and provide objective confirmation of abnormal daytime sleepiness in DLB.
Pathophysiology Of Excessive Daytime Sleepiness In Pd
It has been reported that there are three main causes of sleepiness in PD; deterioration of night sleep quality, neurodegeneration of sleepwake-related brain regions, as a result of disease pathology, and the side effects of antiparkinsonian medications . However, many of the abovementioned causes may be related to EDS.;For this reason, it is necessary to consider these causes in the diagnosis and treatment of EDS.
Don’t Miss: How To Help Someone With Parkinson’s
Mechanism Of Arousal In Parkinson’s Disease And Dementia With Lewy Bodies
Lewy body disease affects the brainstem and hypothalamic sleep-wake centers, and the pathology affects multiple neurotransmitter systems . Saper et al. have provided data and a theoretical framework for a neuroanatomic flip-flop switch that regulates the transition from sleep to wakefulness. It includes mutually inhibitory elements responsible for sleep initiation, and brainstem nuclei that promote arousal. One hypothesis for the daytime somnolence in PD and DLB may be associated with the disruption of the wakefulness centers, but perhaps also to damage to the mechanism that switches and maintains wakefulness, presumed to reside in the hypothalamic hypocretin neurons. Involvement of the latter may lead to difficulty keeping the arousal switch in place, which may result in trouble maintaining wakefulness and/or frequent brief transitions of sleep into wakefulness, or microsleeps.
