Strengths And Limitations Of This Study
-
High-quality 3T MRI data in a very well phenotyped and longitudinally followed cohort of Parkinsons and rapid eye movement sleep behaviour disorder were acquired on the same MRI scanner, quite unique for a study of this duration.
-
Clinical longitudinal data are acquired every 18 months, information about conversion to Parkinsons of the at-risk individuals will be available, and MRI follow-up is ongoing.
-
Statistical maps of published results and support data relative to the analyses are available to share.
-
Oxford Parkinsons Disease Centre-MRI phenotyping is deep and relatively frequent, however, the size of the cohort is not at the level of population-level cohort studies.
-
MRI sequences are high quality, but could not exploit the latest advances in the field in order to maintain continuity.
Whats A Nuclear Medicine Scan
A nuclear medicine scan uses small amounts of radiation to create pictures of tissues, bones, and organs inside the body.
The radioactive material collects in certain areas of your body, and special cameras find the radiation and make images that help your medical team diagnose and treat cancer and other illnesses.
Other terms your doctor might use for a nuclear medicine scan are:
- Radionuclide imaging
Parkinsons Is A Clinical Diagnosis
It turns out that the clinical features of PD are unique to PD and often very easy to see via a neurologic exam in a doctors office. Rest tremor for example, is seen in virtually no other illness. The skill is being able to distinguish a rest tremor from other tremors, which neurologists are trained to do.
However, some people with PD do not have a rest tremor, which can make the diagnosis trickier. Nevertheless, some elements of the standard in-office neurologic exam are very characteristic, such as
- small handwriting, that decreases in size as the writing continues
- small, movements of the hands and the feet, worse on one side,
- characteristic stiffness of the arms and the legs, worse on one side,
- stooped posture
- the characteristic walk in which the whole foot is planted flat at one time instead of the heel being planted on the ground first
- the characteristic way of turning by taking multiple steps and not pivoting
If there are enough of these features present during an exam, with or without a rest tremor, especially if coupled with a history of certain non-motor symptoms that typically appear before the movement symptoms of PD, such as constipation, loss of smell and REM behavior sleep disorder, the practitioner will feel sure of the diagnosis.
Don’t Miss: Is There A Link Between Fibromyalgia And Parkinson’s
Parkinson’s Disease And Movement Disorders Center
Our center provides compassionate and timely treatment to patients with movement disorders, such as dystonia, ataxia, essential tremor and similar conditions. But our mission goes beyond patient care excellence. By offering educational events and support groups, we empower patients and caregivers to become better partners in their health.
What Are The Early Warning Signs Of Parkinson’s Disease
Parkinsons warning signs can be motor symptoms like slow movements, tremors or stiffness. However, they can also be non-motor symptoms. Many of the possible non-motor symptoms can appear years or even decades ahead of motor symptoms. However, non-motor symptoms can also be vague, making it difficult to connect them to Parkinson’s disease.
Non-motor symptoms that might be early warning signs include:
Recommended Reading: What Is Deep Brain Stimulation For Parkinson’s Disease
Mechanisms Underlying Fluctuations And Dyskinesias
PD patients show reduced putamen 18F-dopa uptake whether they have sustained or fluctuating motor responses to levodopa, but mean uptake is 20% lower in the latter group . There is, however, considerable overlap of individual levels of putamen 18F-dopa uptake in fluctuator and nonfluctuator cohorts, and so, loss of putamen dopamine terminal function cannot be the sole factor responsible for determining the timing of onset of motor complications.
11C-raclopride PET studies have reported that putamen D2 binding is initially increased by up to 20% in de novo PD but that after 6 mo of treatment with levodopa, D2 receptor availability returns to normal . 11C-SCH23390 PET reveals normal striatal D1 binding in de novo PD, whereas patients chronically exposed to levodopa show a 20% reduction . Striatal dopamine D1 and D2 receptor availability has been compared in dyskinetic and nondyskinetic groups of PD patients with similar clinical disease duration and severity who were receiving a similar daily dose of levodopa . Similar levels of D1 and D2 receptor binding were found, suggesting that onset of motor fluctuations and dyskinesias in PD is not driven by alterations in striatal postsynaptic dopamine receptor availability.
What Is A Datscan And What Role Does It Play In A Parkinsons Diagnosis
In 2011, the FDA approved the use of a scan called a dopamine transporter scan . A DaTscan is an imaging technology that allows visualization of the dopamine system in the brain. It is similar to an MRI, but looks at the function of the brain rather than the structure.
A DaTscan involves injection of a small amount of a radioactive drug that is then measured by a single-photon emission computed tomography scanner . The SPECT scanner measures the levels and location of the drug in the brain.
It is important to know that a negative DaTscan does not rule out PD, especially early in the disease, but a positive DaTscan can help confirm it. A positive DaTscan can differentiate PD from essential tremor as there is no dopamine deficiency in the latter. However, DaTscan abnormalities can be seen in PD as well as other forms of atypical parkinsonism that cause a loss of dopamine . This means that a positive result does not differentiate Parkinsons disease from other forms of atypical parkinsonism.
Recommended Reading: Benefits For Parkinson’s Patients
What Doctors Look For When Diagnosing Parkinsons
Certain physical signs and symptoms noticed by the patient or his or her loved ones are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctors office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinsons disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
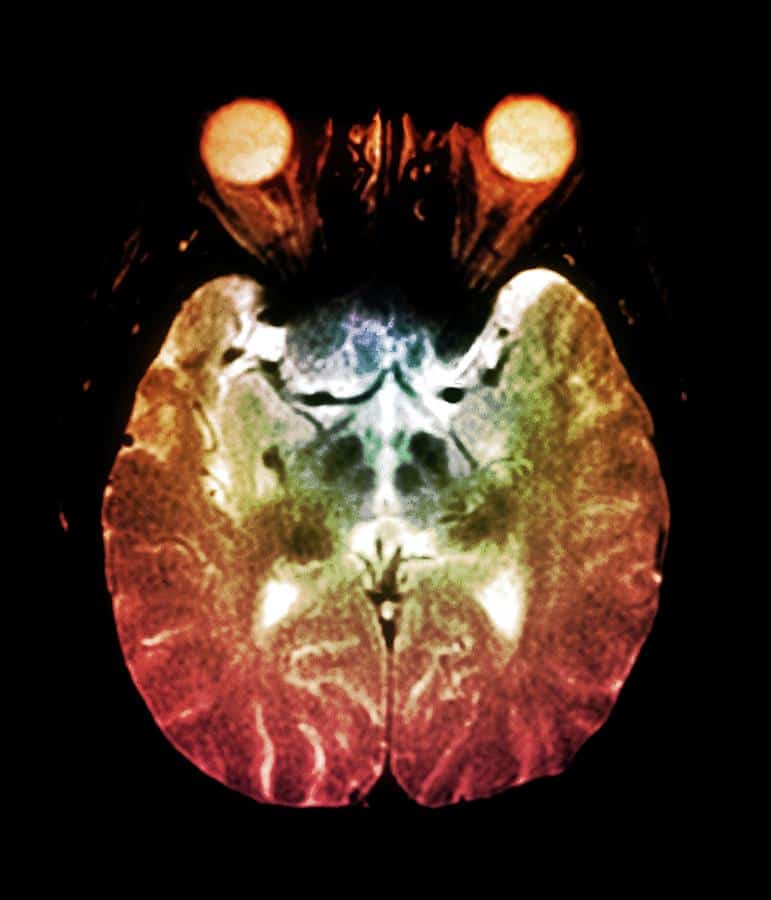
How Can Mris Be Used To Detect Early Onset Parkinsons
MRIs use magnets to create detailed images of the inside of the body. Brain MRIs can help doctors spot tumors, brain bleeding, and other brain health conditions. Recently, medical researchers have discovered that MRIs can also spot small changes in the brain that can indicate Parkinsons disease.
A 2019 study on MRIs and Parkinsons found that people with Parkinsons often have visibly damaged brain neurons. The damage to neurons is present before any brain atrophy begins, and before symptoms are present.
Using this information, doctors can prescribe appropriate treatments, such as Deep Brain Stimulation therapy, that can slow down decline and improve the quality of life for people with Parkinsons.
Don’t Miss: What Year Was Michael J Fox Diagnosed With Parkinson’s Disease
Patient And Public Involvement
The OPDC Discovery Cohort is designed by and for patients and is closely linked with the Parkinsons UK local support group. Patient representatives are also involved in the funding/renewal and strategic oversight processes, and sit on the data access panel with casting votes. Results are disseminated to the study participants through annual newsletters, the OPDC website, and series of talks at participants open days.
What Can I Expect On The Day Of The Ct Scan
Please allow at least one hour for your CT scan. Most scans take from 15 to 60 minutes.
Depending on the type of scan you need, a contrast material may be injected intravenously so the radiologist can see the body structures on the CT image.
After the contrast agent is injected, you may feel flushed, or you may have a metallic taste in your mouth. These are common reactions. If you experience shortness of breath or any unusual symptoms, please tell the technologist.
The technologist will help you lie in the correct position on the examining table. The table will then automatically move into place for imaging. It is very important that you lie as still as possible during the entire procedure. Movement could blur the images. You may be asked to hold your breath briefly at intervals when the X-ray images are taken.
After the test is performed the results are reviewed by a radiologist.
You May Like: What Can Cause Hand Tremors Besides Parkinson’s
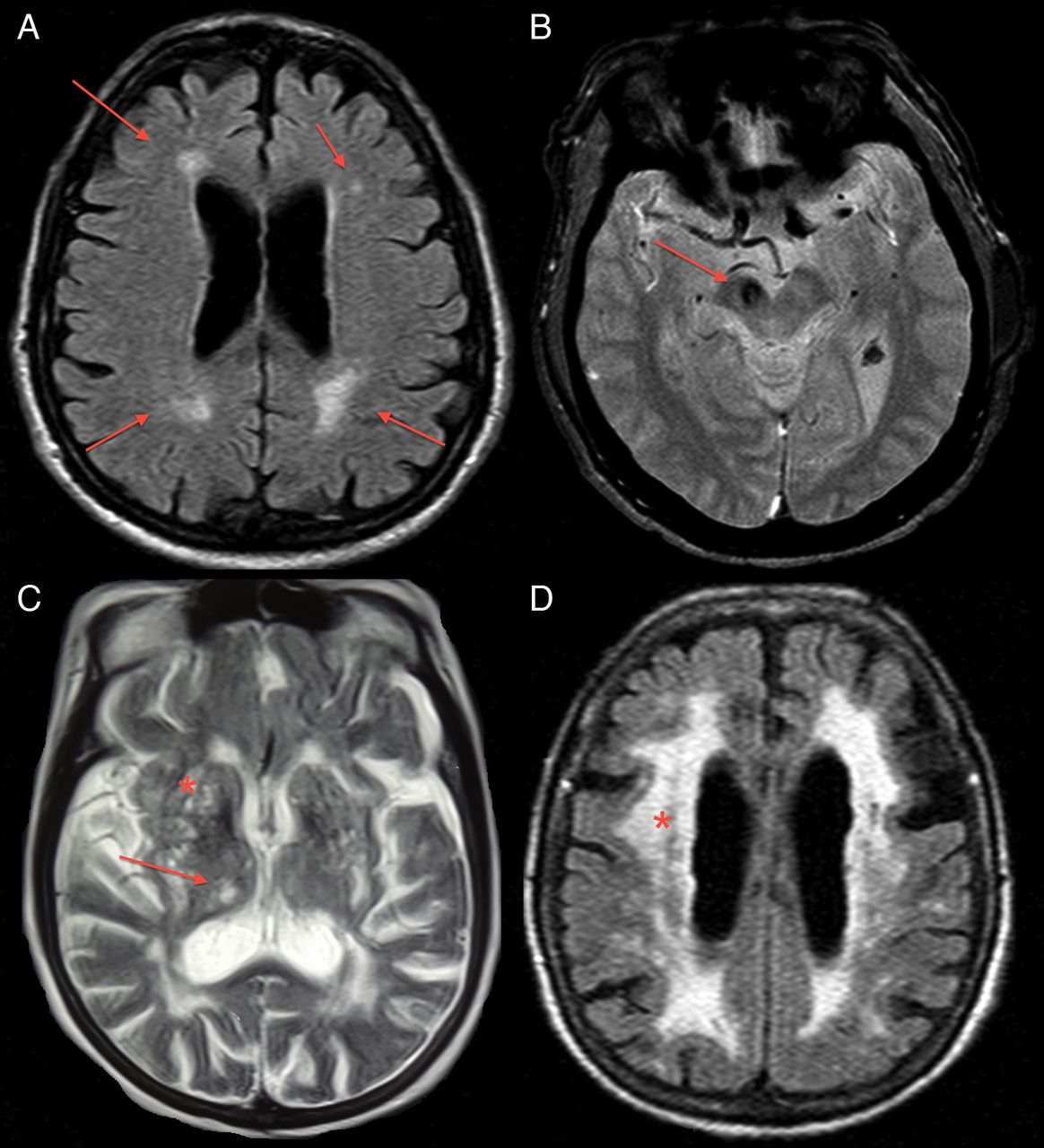
Clinical Application Of Brain Mri In The Diagnostic Work
aDepartment of Radiology and Nuclear Medicine, Radboud University Medical Center, Nijmegen, The NetherlandsbDepartment of Diagnostic Imaging, Medical Center of Postgraduate Education, Warsaw, PolandcDepartment of Neurology, Donders Institute for Brain, Cognition and Behaviour, Radboud University Medical Center, Nijmegen, The Netherlands
Keywords: Atypical parkinsonism, brain, magnetic resonance imaging, Parkinsons disease
ABSTRACT
Background: Differentiating Parkinsons disease and atypical parkinsonism on clinical parameters is challenging, especially in early disease courses. This is due to large overlap in symptoms and because the so called red flags, i.e. symptoms indicating atypical parkinsonism, have not developed. Brain MRI can aid to improve the accuracy and confidence about the diagnosis.Objective and Methods: In the current paper, we discuss when brain MRI should be performed in the diagnostic work-up of parkinsonism, our preferred brain MRI scanning protocol, and the diagnostic value of specific abnormalities.Results and Conclusions: The main purpose of brain MRI is to assess cerebrovascular damage, and to exclude other possible and sometimes treatable causes of parkinsonism, such as normal pressure hydrocephalus. Furthermore, brain MRI can support the possible or probable diagnosis of a specific form of atypical parkinsonism.
INTRODUCTION OF THE CLINICAL DILEMMA
DESCRIPTION OF THE TEST
DISCUSSION
ACKNOWLEDGMENTS
CONFLICT OF INTEREST
Does The Pet Scan Have Risks
Because radiation is part of a PET scan, there is always a small risk that cells or tissue may have received some damage following the procedure. However, the radiation levels from the tracer that is sent throughout the body are very low.
In addition, following the scan, patients may find that their arm is a little bit sore or that they experience redness where the IV was placed in the arm.
Read Also: Does 23andme Test For Parkinson’s
Differential Diagnosis Of Parkinsonian Syndromes Using Quantitative Biomarkers
Several studies have suggested that the combination of R2* and FA markers may better differentiate people with PD from healthy aged subjects with greater than 95% global accuracy .
In MSA-P, increased diffusivity and reduced anisotropy was found in the putamen, pons and middle cerebellar peduncle and greater iron deposition in the putamen, using phase-contrast susceptibility imaging or relaxometry .
Tauopathies Progressive Supranuclear Palsy And Corticobasal Degeneration
Formally described in 1964 by Steele, Richardson and Olszewski, PSP is a progressive neurodegenerative disease associated with axial rigidity, bradykinesia, postural instability, vertical supranuclear gaze palsy, speech and swallowing dysfunction, as well as fronto-executive cognitive and behavioural manifestations . Gait impairment typically progresses at an accelerated rate in PSP relative to PD, with early falls as a prominent feature. Several variants have been identified that challenge the classical clinicopathological characterization of the PSP syndrome. For example, unlike the classical syndrome , the PSP-parkinsonism variant exhibits more conspicuous limb rigidity with bradykinesia and/or tremor with moderate levodopa response in a proportion of patients, without early ocular or postural disturbances . Vertical gaze palsy is an important diagnostic feature of PSP, although it may not be evident at early disease stages . Histopathologically, evidence of neurofibrillary tangles composed of misfolded 4-repeat tau protein, neuropil threads and star-shaped tufted astrocytes are seen, mainly in the basal ganglia, brainstem and diencephalon .
Recommended Reading: How Do People Get Parkinson’s
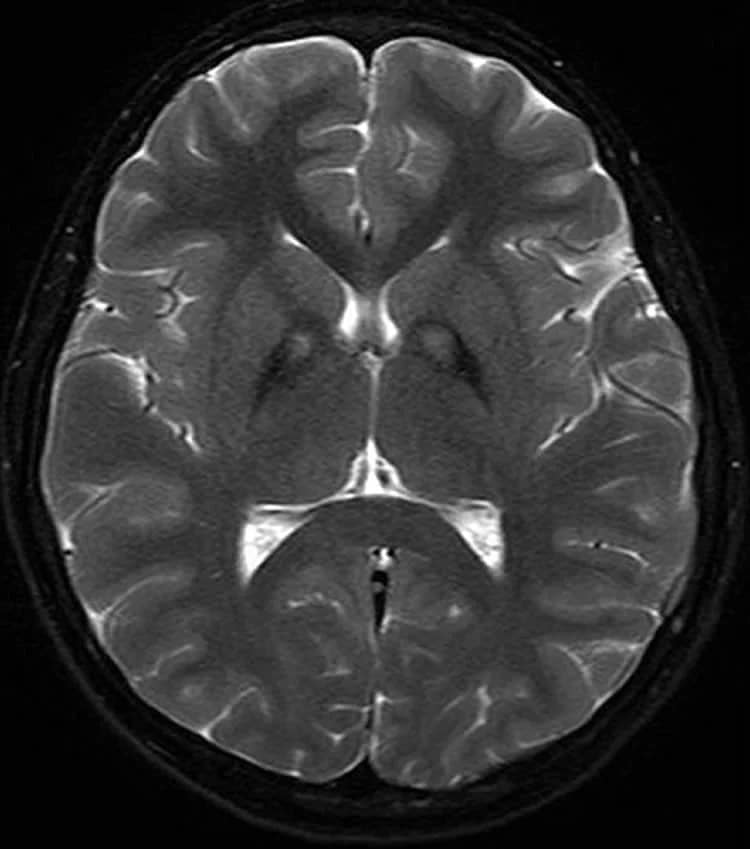
Functional Imaging And Atypical Pd
Imaging presynaptic dopaminergic terminal function with either striatal 18F-dopa uptake or a DAT SPECT marker shows high sensitivity for detecting atypical parkinsonian syndromes but only poor specificity for discriminating them from typical PD . The typical gradient of loss of dopaminergic function in PD, where the head of the caudate is relatively spared, is less evident in progressive supranuclear palsy and corticobasal degeneration patients . In progressive supranuclear palsy, there is a more symmetric pattern of nigrostriatal dysfunction than in other parkinsonian syndromes.
In contrast, measurements of resting glucose metabolism can be helpful for separating typical from atypical parkinsonian syndromes. In typical idiopathic PD, lentiform nucleus glucose metabolism is preserved or raised, whereas it is reduced in most atypical cases .
FIGURE 5.
18F-FDG PET images of PD and multiple-system atrophy patient. Multiple-system atrophy patient shows significant striatal reduction of glucose metabolism. MSA = multiple-system atrophy.
You May Like: Best Bed For Parkinsons Patients
What Are The Limitations Of The Test
Currently, DaTscan that is in clinical use is not quantitative, which means that the test is not designed to determine how impaired the dopamine system is just whether it is or not. This means that the test is not used to tell you whether the disease has progressed over time and is not used to follow a patients disease. It also is not used currently as a clinical test to screen for the disease before motor symptoms are evident. Because of these limitations, the search continues for additional measurable indicators, known as biomarkers, to help diagnosis and manage PD.
Recommended Reading: Parkinsons Stiffness In Morning
You May Like: Lewy Body Parkinson’s Prognosis
Determining Diagnosis Through Response To Parkinsons Medication
If a persons symptoms and neurologic examination are only suggestive of Parkinsons disease or if the diagnosis is otherwise in doubt, the physician may, nevertheless, prescribe a medication intended for Parkinsons disease to provide additional information. In the case of idiopathic Parkinsons, there is typically a positive, predictable response to Parkinsons disease medication in the case of some related Parkinsonian syndromes, the response to medication may not be particularly robust, or it may be absent entirely.
Unfortunately, there are no standard biological tests for the disease, such as a blood test. However, researchers are actively trying to find biomarkers in blood and other bodily fluids that could help confirm the diagnosis.
Dont Miss: What Foods Should Be Avoided When Taking Levodopa
Is Parkinson’s Diagnosed In The Brain
Parkinson’s disease is one of the most challenging neurological disorders to diagnose and treat. If your doctor suspects you have Parkinson’s disease, you will usually be referred to a neurologist for further tests. These tests will involve certain movements and exercises to check your symptoms.
A neurologist will look for motor symptoms such as:
- A tremor that occurs at rest
- Slowed movement
- Muscle stiffness
If you have two or more of these symptoms and your doctor has taken blood tests to rule out other causes, it’s likely you will be diagnosed with Parkinson’s disease. Your symptoms will be closely monitored to see any progression of Parkinson’s disease, which can take years.
Don’t Miss: What’s New In Parkinson’s
Is There Anything I Can Do To Slow The Progression Of Parkinsons Symptoms
Treatment for Parkinsons can help you manage your symptoms. Currently, theres no way to cure or stop the progression of Parkinsons. However, medical professionals have found ways to slow the progression of symptoms with therapies such as medications and deep brain therapy.
Diet and exercise are also known to slow down Parkinsons. Studies have shown that eating a nutritious diet, such as the Mediterranean diet, can help slow down the progression of Parkinsons disease.
Additionally, getting regular exercise has been shown to slow down symptom progression. People with Parkinsons should try to get at least 2.5 hours of exercise each week. A physical therapist or another medical professional can help you develop an exercise routine that meets your needs.
Imaging Studies Can Differentiate Parkinsons From Other Causes Of Parkinsonism
Catherine L. Gallagher, MD
Although Parkinsons disease remains a clinical diagnosis, imaging studies are an important ancillary test for differential diagnosis of movement disorders. Imaging studies may be used to rule out structural and other causes of parkinsonian symptoms. Single-photon emission computed tomography scans using labeled tracers for dopamine transporters can also be used to confirm parkinsonism or differentiate PD from secondary causes of parkinsonian motor symptoms. Finally, imaging studies are being used in research to better understand the pathophysiology of PD and elucidate causative mechanisms that could be therapeutic targets in the future.
You May Like: Does Parkinsons Medication Cause Hallucinations
Postsynaptic Dopamine D2 Receptor Imaging
Using SPECT with 123I-IBZM and 123I–5-iodo-7-N– carboxamido-2,3-dihydrobenzofuran as ligands, binding potentials for postsynaptic D2 receptors were identified to be within the normal range in levodopa-treated PD as well as in patients with essential tremor and DLB . Conversely, reduced binding potentials were detected among MSA and PSP patients versus controls . Striatal D2 receptors were upregulated in drug-naïve PD patients, likely in response to nigrostriatal denervation with the greatest increase in the posterior putamen . Studies generally find the density of D2 receptors to be preserved among CBS patients, although this finding was not reliably shown on an individual case-to-case basis. Using 123I-IBZM as a tracer, Klaffke et al. , Pirker at al. and Plotkin at al. respectively reported 7 out of 8 , 8/9 and 7/9 clinically-diagnosed CBS patients with normal D2 bindings, suggesting preservation of dopamine D2 receptors. It is important to consider that a normal D2 SPECT scan may not exclusively confirm or discount an atypical PS. Further studies with pathologically-proven samples are warranted to determine the true sensitivity and specificity of D2 SPECT in distinguishing atypical PS.
