Benefits For Veterans Exposed To Agent Orange
Veterans with PD who were exposed to Agent Orange during military service and their families may be eligible for VA health care, disability, or survivor payments.7 VA offices and government websites can help locate available local services and forms needed to apply for medical, compensatory, and monetary benefits.
Study Examines Association Between Parkinson Disease Cancer
- Date:
- JAMA and Archives Journals
- Summary:
- A study that used a Utah genealogic database and a statewide cancer registry to examine the relationship between Parkinson disease and cancer suggests an increased risk of prostate cancer and melanoma in patients with PD and their relatives.
A study that used a Utahgenealogic database and a statewide cancer registry to examine the relationship between Parkinson disease and cancer suggests an increased risk of prostate cancer and melanoma in patients with PD and their relatives, according to a report published Online First by Archives of Neurology, a JAMA Network publication.
Neurodegenerative diseases, in particular PD, may share common pathogenic mechanisms with some cancers, according to the study background.
“Identifying a genetic relationship between PD and cancer is critical to understanding underlying pathophysiologic changes in both diseases. Understanding this relationship could allow clinicians to provide proper assessment of cancer risk in patients with PD and might also have implications for the counseling of relatives of patients,” the authors note in the study background.
To validate their observed associations, researchers also estimated the reciprocal RR for PD death among patients diagnosed with melanoma and their relatives, and estimated the RRs for death with PD among patients diagnosed with prostate cancer and their relatives.
Editorial: Families with Parkinson Disease, Cancer
Story Source:
Association Between Parkinson’s Disease And Prostate Cancer
Researchers have found compelling evidence that Parkinson’s disease is associated with an increased risk of prostate cancer and melanoma, and that this increased cancer risk also extends to close and distant relatives of individuals with Parkinson’s disease.
Although a link between Parkinson’s disease and melanoma has been suspected before, this is the first time that an increased risk of prostate cancer has been reported in Parkinson’s disease.
Parkinson’s disease is a progressive neurologic condition that leads to tremors and difficulty with walking, movement, and coordination. Most studies demonstrate that individuals with PD have an overall decreased rate of cancer, with the notable exception of melanoma, the most serious form of skin cancer.
Previous research has suggested a possible genetic link between PD and melanoma, but these studies have been limited to first-degree relatives who often share a similar environment, making it difficult to distinguish between genetic and environmental risk factors.
“Neurodegenerative disorders such as Parkinson’s disease may share common disease-causing mechanisms with some cancers,” says Stefan-M. Pulst at the University of Utah. “Using the Utah Population Database, we were able to explore the association of PD with different types of cancer by studying cancer risk in individuals with PD, as well as their close and distant relatives.”
REHACARE.de; Source: University of Utah Health Sciences
Family History And Genetic Factors
Inherited factors explain around 59% of prostate cancers, it is estimated. A mix of genetic/biological factors and increased diagnostic activity in affected families may underpin the familial risk. Prostate cancer risk is not associated with prostate cancer in an adoptive parent , but it is higher sooner rather than later after diagnosis in a family member, , cohort studies have shown.
Family history
Prostate cancer risk is 2.1-2.4 times higher in men whose father has/had the disease, meta-analyses have shown. Prostate cancer risk is 2.9-3.3 times higher in men whose brother has/had the disease, meta-analyses have shown. Prostate cancer risk is 1.9 times higher in men with a second-degree relative who has/had the disease, a meta-analysis has shown.
Familial prostate cancer risk is higher in men aged under 65 compared with older men, and in men with more than one affected first-degree relative or with an affected relative diagnosed aged younger than 60.
Prostate cancer risk is 19-24% higher in men whose mother has/had breast cancer, cohort studies have shown. Prostate cancer risk is not associated with breast cancer in a sister.
BRCA1 and BRCA2
Lynch syndrome
Prostate cancer risk is 2.1-4.9 times higher in men with Lynch syndrome, compared with the general population, a meta-analysis and cohort study have shown.
How Lyme Disease And Chronic Infections Can Lead To Cancer
Envita Medical Center has been treating cancer for nearly two decades, in that time they have tested and reviewed thousands of patients and their potential causes of cancer. This accumulation of clinical data has allowed Envita to notice a recurring trend between cancer patients and underlying chronic infections, leading to a published paper on the subject in the 2014 Open Journal of Medical Microbiology titled Cancer and Infectious Causes. Data is very clear that specific cancers are linked to certain infections, many people are aware that infections like HPV can lead to cervical cancer, and Epstein Barr can cause Hodgkin’s Lymphoma. What you may not know is that recent data suggests 25% of all infections may potentially lead to cancer and this statistic, in our clinical experience, could be an underestimate. Patients with chronic Lyme disease may not realize the potential cancer risk they are exposing themselves to. A surprisingly high number of Envita’s patients with late-stage cancer test positive for Lyme disease as well as its primary or secondary coinfections.
Envita Medical Centers doesn’t make any guarantee of outcomes. Results are not typical and will vary from person to person and should not be expected.
Prostate Cancer Treatment Linked To Dementia Risk
MONDAY, July 8, 2019 — Soon after a man is diagnosed with prostate cancer, that lower levels of testosterone are often offered as treatment, since testosterone fuels the ‘s growth.
But a major new study suggests that this approach might have an unwanted side effect: Higher odds for Alzheimer’s disease and other dementias.
“Our results suggest that clinicians need to raise their awareness about potential long-term cognitive effects of hormone therapy and discuss these risks with their patients,” said study author Ravishankar Jayadevappa.
He’s a research associate professor of geriatrics at the University of Pennsylvania’s Perelman School of Medicine in Philadelphia.
One expert said it does raise troubling questions.
“Most of us are becoming as afraid of getting as we are of getting cancer,” said Dr. Elizabeth Kavaler, a urology specialist at Lenox Hill Hospital in New York City. “When a study pits one debilitating condition against another, it instills fear in patients.”
But the treatment — called androgen-deprivation therapy — remains the “gold standard” for many cases of prostate cancer, according to Kavaler. Therefore, the new data means “tough decision-making” for patients and their physicians, she said.
When the team looked at diagnoses of all forms of dementia, 22% of those who’d received the therapy received such a diagnosis, compared to 16% of those who hadn’t undergone hormonal therapy.
Continued
The study was published online July 3 in JAMA Network Open.
Androgen Deprivation Therapy Did Not Increase The Risk Of Alzheimer’s And Parkinson’s Disease In Patients With Prostate Cancer
Division of Urology, Department of Surgery, Far Eastern Memorial Hospital, Banciao, Taipei, Taiwan
Graduate Program in Biomedical Informatics, College of Informatics, Yuan-Ze University, Chung-Li, Taiwan
Sleep Research Center, Taipei Medical University Hospital, Taipei, Taiwan
Sleep Research Center, Taipei Medical University Hospital, Taipei, Taiwan
School of Health Care Administration, Taipei Medical University, Taipei, Taiwan
School of Health Care Administration, Taipei Medical University, Taipei, Taiwan
Department of Internal Medicine, Cathay General Hospital, Hsinchu, Taiwan
School of Health Care Administration, Taipei Medical University, Taipei, Taiwan
Correspondence:
Kuan-Chen Chen, School of Health Care Administration, College of Medicine, Taipei Medical University, 250 Wu-Hsing St., Taipei 110, Taiwan.
Division of Urology, Department of Surgery, Far Eastern Memorial Hospital, Banciao, Taipei, Taiwan
Graduate Program in Biomedical Informatics, College of Informatics, Yuan-Ze University, Chung-Li, Taiwan
Sleep Research Center, Taipei Medical University Hospital, Taipei, Taiwan
Sleep Research Center, Taipei Medical University Hospital, Taipei, Taiwan
School of Health Care Administration, Taipei Medical University, Taipei, Taiwan
School of Health Care Administration, Taipei Medical University, Taipei, Taiwan
Department of Internal Medicine, Cathay General Hospital, Hsinchu, Taiwan
School of Health Care Administration, Taipei Medical University, Taipei, Taiwan
Mendelian Randomization Does Not Support A Causal Role For Different Cancers And Pd
We performed MR with the five cancers for which we had full summary statistics. We further included 10 additional cancers with limited summary statistics, resulting in 15 cancers being included in this part of the analysis . The variance in the exposure variables explained by SNPs ranged from 0.016 to 0.059 . All instruments had F-statistics of >10, which is the cut-off that most studies apply to indicate sufficient instrument strength . No causal effect of any cancer on PD was observed . Significant heterogeneity was apparent for cutaneous squamous cell carcinoma and combined analysis of keratinocyte cancers . There was some evidence for net horizontal pleiotropy for brain tumors and cutaneous squamous cell carcinoma which may have resulted in bias to IVW estimates, but the slopes from Egger regression were imprecisely estimated. MR-PRESSO identified potential outliers for cutaneous squamous cell carcinoma . The distortion test did not suggest significant changes in the effect estimates after these outliers were removed . The sensitivity analyses revealed no clear evidence for bias in the IVW estimate due to invalid instruments with other cancers.
Additionally, we performed reverse MR using PD-associated SNPs as exposure and cancer summary statistics as outcome and did not find any evidence of causal relationship .
Prospective Cohort Study Of Pd After Cancer
The characteristics of the 743 779 cancer patients and 419 432 persons in the comparison group in the cohort analysis are presented in Table 1a . The cancer patients were more likely to be older, male and selected later, but the racial/ethnicity distributions were similar. There were 2.1 million person-years of follow-up in the cancer patients and 2.4 million , in the comparison group.
Characteristics of cancer patients and non-cancer comparison group in prospective cohort analysis of Parkinsons disease following cancer
| . |
|---|
Overall there was no association with PD within 10 years after cancer diagnosis ; Table 2 ; Supplementary Tables 1 and 2 , for unadjusted HRs, and age-specific incidence rates in cancer patients and the comparison groups, respectively, available as Supplementary data at IJE online). There were slight inverse associations between cancer and subsequent PD in men and in those aged between 70 and 84 years at baseline; however, these associations did not withstand multiple testing corrections. The associations for selected cancers were similar across age groups .
Characteristics of cancer cases and non-cancer control group in retrospective case-control analysis of Parkinsons disease before cancer
| . |
|---|
Strengths And Limitations Of This Study
-
Unlike recent meta-analyses, this study stratifies analysis for smoking vs non-smoking cancers.
-
Heterogeneity between included studies was analyzed via meta-regression.
-
Despite best efforts, high heterogeneity in methodology and cohorts of included studies cannot be fully dealt with by statistical methods.
Parkinson’s Disease Associated With Higher Risk Of Certain Cancers
People with Parkinson’s disease and their relatives may be more likely to develop prostate cancer and melanoma. Researchers believe neurodegenerative diseases may share common mechanisms with the cancers.
To continue reading this article, you must log in.
- Research health conditions
- Prepare for a doctor’s visit or test
- Find the best treatments and procedures for you
- Explore options for better nutrition and exercise
Financial Disclosures Of All Authors
ZGO has received consulting fees from Lysosomal Therapeutics Inc., Idorsia, Prevail Therapeutics, Denali, Ono Therapeutics, Neuron23, Handl Therapeutics, Deerfield and Inception Sciences . None of these companies were involved in any parts of preparing, drafting and publishing this study. AJN received grants from the Barts Charity, Parkinsons UK and Aligning Science Across Parkinsons; and honoraria from Britannia, BIAL, AbbVie, Global Kinetics Corporation, Profile, Biogen, and Roche. The rest of the authors have nothing to report.
Is It Genetic Or Environmental
Underlying functional changes are part of the disease process for prostate cancer, PD and melanoma.1 PD and cancer seem to have opposite effects on cells. PD degenerates nerve cells, and cancer causes cells to grow out of control. Identifying any genetic links between these diseases may help direct future screening and development of treatment protocols. Similarly, environmental factors may play an influential role. The Utah study had a geographically-controlled and genetically-similar population.
Link Confirmed Between A Healthy Diet And Prostate Cancer Prevention
The Canadian Cancer Society estimates that more than 23,000 Canadians will be diagnosed with prostate cancer in 2020. Among other risk factors, more and more studies point to diet as a major factor in the development of prostate cancer, as it is for cardiovascular disease, diabetes, and obesity. Using data from a study conducted in Montreal between 2005 and 2012, a research team led by Professor Marie-Élise Parent of Institut national de la recherche scientifique has shown a link between diet and prostate cancer in the article “Dietary Patterns Are Associated with Risk of Prostate Cancer in a Population-Based Case-Control Study in Montreal, Canada,” published in Nutrients in June.
Three main dietary profiles analyzed
INRS Ph.D. student Karine Trudeau, the lead author of the study, based her analysis on three main dietary profiles: healthy , salty Western diet including alcohol, and sugar-rich Western diet with beverages. The first profile leans heavily towards fruits, vegetables, and plant proteins like tofu and nuts. The salty Western diet with alcohol includes more meat and beverages such as beer and wine. The third profile is rich in pasta, pizza, desserts, and sugary carbonated drinks. The study took age, ethnicity, education, family history, and date of last prostate screening into account.
Explore further
The Link Between Parkinson’s Disease And Breast And Prostate Cancers: A Meta
Purpose: Clinical observations have shown an increased morbidity for breast cancer or prostate cancer in patients with Parkinson’s disease , however, other reports have noted contradictory results. This pooled analysis was utilized to test whether PD is associated with the risk of breast or prostate cancer. Methods: We searched PubMed, Embase and Cochrane library and conducted a meta-analysis to clarify the correlation of PD with breast and/or prostate cancer risk. We identified 16 eligible articles from which odds ratios with 95% confident intervals were assessed as main measures in the pooled estimation. Subgroup analyses and cumulative meta-analysis were also performed. Results: Our results showed no PD risk associated with breast or prostate cancer in the overall population, which was supported by the results of cumulative meta-analyses. The subgroup analyses suggested no significant risk of breast or prostate cancer in patients with PD within relevant subsets, i.e. gender, ethnicity, PD diagnosis time or study design. No evidence of publication bias was observed across the involved studies. : This meta-analysis indicates a lack of association between PD and risk of breast or prostate cancer.
Common Elements To Both Designs
We assessed associations stratified by sex, race/ethnicity and age at time of selection , and separately for specific cancer sites and smoking-related and other cancers. Associations by age strata for selected cancer sites are also presented. We limited cancer-site specific analyses to sites with at least 20 PD cases.
All models were adjusted for: sex, race/ethnicity, age , cancer registry and frequency of physician visits. For cohort models, the baseline hazard was also stratified on birth year , and case-control analyses were adjusted for year of selection .
The first PD claim date was treated as the diagnosis date. PD risks were analysed across time intervals: < 1 year; 1< 5 years; 5< 10 years; and 0< 10 years after cancer ; and < 1 year; 1< 5 years; and 0< 5 years before cancer because some claims were limited to 5 years. Also, because patients with serious disease often receive heightened medical surveillance, we adjusted for physician visit frequency. In the cohort analyses, physician visits were counted during 6-month intervals between the selection and censor dates and, in the case-control analyses, we adjusted for the average number of visits across all intervals Claims by physicians with limited responsibility for direct patient care were excluded.
Studies Of Cancer Associated With Automobile Accident Injuries
To evaluate ascertainment bias, we examined the relationship between cancer and automobile accident injuries occurring both before and after cancer. We expected no associations because we were unable to suggest a plausible hypothesis biologically relating automobile injuries to cancer. We also examined the risk of prostate and breast cancer after automobile accidents, two cancers on which potential confounding by smoking or alcohol would have little impact. As an acute injury, automobile injury claims were based on one medical visit. In prospective cohort analyses of cancer followed by automobile injuries, cancer patients were excluded if they had previous automobile injuries. In other respects, the analyses followed the models for cancer and PD.
We applied the Bonferroni correction to account for multiple comparisons when interpreting results of all the sub-groups and site-specific cancers for the 010 year follow-up period in the cohort analysis and thus used a corrected P -value of P<0.0019 as a threshold for associations. P -values were based on two-sided tests. All analyses used SAS . This study was exempted by the National Institutes of Health Office of Human Subjects Research from institutional board approval.
What Has Research Found
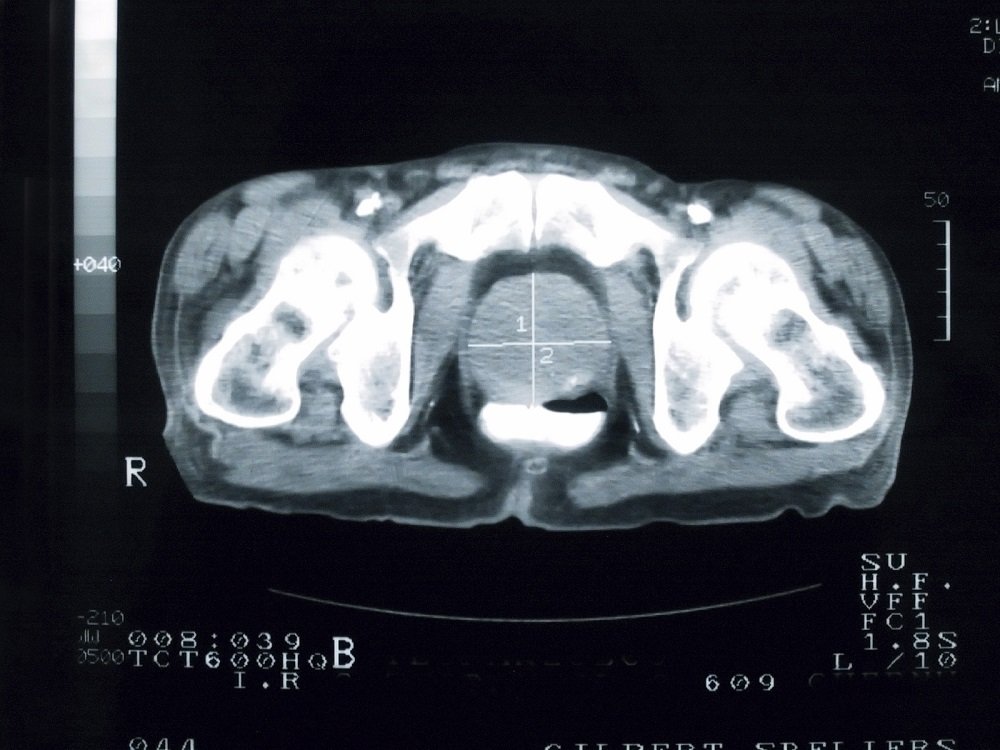
The Utah Population Data Base has extensive genealogical information on more than 2.2 million people over 15 generations. It is linked to the statewide cancer registry. A large-scale study out of the University of Utah reviewed records containing information on birth, death and relationships. They identified 3,000 people with 3 generations who had PD listed as the cause of death.
Results from this extensive data set suggest that the risk of prostate cancer and melanoma within the population was significantly higher than expected. In fact, the increased risk was also evident amongst of people with PD. The Utah database was able to assess risk in first, second and third-degree relatives.2 The findings are statistically significant with first- and second-degree relatives.
The study sought to validate its results by cross-examining data. Researchers identified people diagnosed with melanoma or prostate cancer and found that they were also at a significantly increased risk of death from Parkinsons disease.1
Novel Link Found Between Parkinsons Disease And Prostate Cancer
University of Utah School of Medicine researchers have found compelling evidence that Parkinsons disease is associated with an increased risk of prostate cancer and melanoma, and that this increased cancer risk also extends to close and distant relatives of individuals with Parkinsons disease. Although a link between Parkinsons disease and melanoma has been suspected before, this is the first time that an increased risk of prostate cancer has been reported in Parkinsons disease.
Parkinsons disease is a progressive neurologic condition that leads to tremors and difficulty with walking, movement, and coordination. Most studies demonstrate that individuals with PD have an overall decreased rate of cancer, with the notable exception of melanoma, the most serious form of skin cancer. Previous research has suggested a possible genetic link between PD and melanoma, but these studies have been limited to first-degree relatives who often share a similar environment, making it difficult to distinguish between genetic and environmental risk factors.
The Utah Population Database includes birth, death, and family relationship data for over 2.2 million individuals, including genealogy data from the original Utah pioneers. Some of the records in this computerized database extend back over 15 generations, making the UPDB a useful resource for studying genetic risk. The UPDB is also linked with the Utah Cancer Registry and Utah death certificates dating back to 1904.
Parkinsons Disease And Melanoma
Even in studies that have established a lower overall cancer risk in people with PD, the risk of certain specific types of cancers is higher than in the general population.
Melanoma is a type of skin cancer that has been consistently linked to PD. People who have had melanoma are at an increased risk for PD and people who have PD are at an increased risk of melanoma. The relationship between melanoma and PD is intriguing:
- The substantia nigra, or the black substance, is the area of the brain that contains the dopaminergic neurons that degenerate in PD. These neurons are full of neuromelanin, a dark pigment found in the brain which is related to melanin, a dark pigment found in the skin.
- Levodopa is a precursor for melanin and neuromelanin.
If a person regularly ingests Levodopa, he/she may be fueling the production of melanin, and possibly the production of melanin-containing cells, which in theory would increase the likelihood of melanoma. However, some studies have demonstrated that the increased melanoma risk is present in patients with PD even before Levodopa is started, suggesting that the relationship is not due to Levodopa intake but rather to a genetic link.
Epidemiological studies have shown an increased risk of non-melanoma skin cancers in PD patients as well.
What to do if you have an increased melanoma risk?
You should know what other melanoma risk factors you have. These include:
Linkage Disequilibrium Score Regression

To investigate whether there is overlapping genetic etiology between PD and the studied cancers we performed a search on the GWAS Catalog for publicly available full summary statistics using keywords cancer, carcinoma, glioma, lymphoma, leukemia, melanoma and selected GWASs with a minimum of 1000 cases and of European ancestry. Additionally, we contacted authors and requested for full summary statistics. Overall, we were able to collect full summary statistics for melanoma, breast, prostate, endometrial and keratinocytes cancers . Keratinocytes cancer summary statistics include meta-analysis of QSkin, eMERGE and UK Biobank cohorts with a total of 28,218 cases and 353,855 controls. Of the cancer studies with full summary statistics, endometrial cancer, melanoma and keratinocyte cancer studies included data from the UKB. We also used GWAS summary statistics from the latest PD GWAS excluding 23andMe and UKB data, to avoid potential bias due to overlapping samples. After the exclusions, a total of 15,056 PD patients and 12,637 controls were included in the summary statistics. We utilized the LDSC method as previously described., Summary statistics were formatted using the standard settings of the munge_sumstats.py script.
Possible Links Of Parkinson’s And Prostate Cancer
Parkinsons and prostate cancer are both age-related diseases. There have been studies demonstrating an association between having PD and an increased likelihood of developing prostate cancer. Genetic links, protein mutations, and certain medications continue to be evaluated.
Levodopa, the first line medication given to people with PD, is involved in production of melanin . These dopaminergic drugs may increase the and skin cancer, according to Dr. Susan Bressman from Beth Israel Deaconess Medical Center. There is evidence that people with PD treated with certain medication combinations had a higher incidence of prostate cancer than those in a control group.
Novel Link Between Parkinson’s And Prostate Cancer
Megan Brooks
September 04, 2012
September 4, 2012 Researchers from Utah have uncovered a novel association between Parkinson’s disease and prostate cancer, which extends to close and distant relatives. The relationship appears reciprocal, with relatives of individuals with prostate cancer at increased risk for PD.
In addition, the study confirms the known association between PD and melanoma, has extended it to close and distant relatives, and has determined that it, too, is reciprocal.
These results “strongly support a genetic link” between PD and these cancers, the authors note.
“The clinical implications suggest screening for melanoma and prostate cancer in appropriate PD patients and perhaps vice versa,” study coauthor Lisa Cannon-Albright, PhD, from the University of Utah, in Salt Lake City, told Medscape Medical News.
Dr. Lisa A. Cannon-Albright
Their findings are September 3 in Archives of Neurology.
Unique Data Source
Data for the study came from the Utah Population Database, which includes the genealogy of Utah pioneers and their descendants, consisting of more than 2 million individuals with some records dating back more than 15 generations. This information was linked to data from the Utah Cancer Registry, which was established in 1966.
This finding supports a recent meta-analysis, published in Neurology and reported byMedscape Medical News, which found a 2-fold increased risk for melanoma in association with PD.
Table. Estimated Risk for Melanoma With PD
