Signs Of Dying In The Elderly With Dementia
Dementia is a general term for a chronic or persistent decline in mental processes including memory loss, impaired reasoning, and personality changes. Alzheimers disease is the most common form of dementia, accounting for 60-80% of all cases of dementia. It is also the 6th leading cause of death in the United States, and over 5 million Americans are currently living with Alzheimers disease.
Alzheimers disease and most progressive dementias do not have a cure. While the disease inevitably worsens over time, that timeline can vary greatly from one patient to the next.
Caring for a loved one can be challenging and stressful, as the individuals personality changes and cognitive function declines. They may even stop recognizing their nearest and dearest friends and relatives. As dementia progresses, the individual will require more and more care. As a family caregiver, its important to be able to recognize the signs of dying in elderly with dementia. Hospice can help by offering care wherever the individual resides, providing physical, emotional and spiritual care to the patient and support their family.
Stage : Moderately Severe Dementia
When the patient begins to forget the names of their children, spouse, or primary caregivers, they are most likely entering stage 6 of dementia and will need full time care. In the sixth stage, patients are generally unaware of their surroundings, cannot recall recent events, and have skewed memories of their personal past. Caregivers and loved ones should watch for:
- Delusional behavior
Dementia With Lewy Bodies And Parkinson Disease Dementia
, MD, PhD, Department of Neurology, University of Mississippi Medical Center
Dementia with Lewy bodiesParkinson disease dementia
Dementia is chronic, global, usually irreversible deterioration of cognition.
Dementia with Lewy bodies is the 3rd most common dementia. Age of onset is typically > 60.
Lewy bodies are spherical, eosinophilic, neuronal cytoplasmic inclusions composed of aggregates of alpha-synuclein, a synaptic protein. They occur in the cortex of some patients who have dementia with Lewy bodies. Neurotransmitter levels and neuronal pathways between the striatum and the neocortex are abnormal.
Lewy bodies also occur in the substantia nigra of patients with Parkinson disease, and dementia may develop late in the disease. About 40% of patients with Parkinson disease develop Parkinson disease dementia, usually after age 70 and about 10 to 15 years after Parkinson disease has been diagnosed.
Because Lewy bodies occur in dementia with Lewy bodies and in Parkinson disease dementia, some experts think that the two disorders may be part of a more generalized synucleinopathy affecting the central and peripheral nervous systems. Lewy bodies sometimes occur in patients with Alzheimer disease, and patients with dementia with Lewy bodies may have neuritic plaques and neurofibrillary tangles. Dementia with Lewy bodies, Parkinson disease, and Alzheimer disease overlap considerably. Further research is needed to clarify the relationships among them.
Recommended Reading: Treating Parkinson’s Disease With Ultrasound
Is Parkinsons Disease Inherited
Scientists have discovered gene mutations that are associated with Parkinsons disease.
There is some belief that some cases of early-onset Parkinsons disease disease starting before age 50 may be inherited. Scientists identified a gene mutation in people with Parkinsons disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinsons disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinsons disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinsons disease.
Scientists think that about 10% to 15% of persons with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
How To Manage Symptoms At The End Of Life
At the end of life, good practice is to plan for any potential symptoms that may arise. The most common symptoms anticipated are pain, dyspnoea, nausea and vomiting, agitation, anxiety, delirium and noisy respiratory secretions.18 For patients with PD particular considerations should be given to the more commonly used medicines, specifically anticholinergics and antidopaminergics. These are usually prescribed for treatment of respiratory secretions and nausea and vomiting. Alternatives are available for respiratory secretions, and include glycopyrronium, in preference to hyoscine hydrobromide. Although this is an anticholinergic, only a small proportion crosses the blood brain barrier.
For nausea and vomiting, ondansetron,19 cyclizine, domperidone have all been suggested in PD.20 However, ondansetron has been shown to be inferior to domperidone in the pre-treatment of apomorphine.21 Cyclizine has anticholinergic properties and may exacerbate confusion, especially when comorbid psychosis or cognitive impairment are present. Levomepromazine, although it has antidopaminergic effects, has been shown to be effective for nausea with rotigotine in a case report.22
Agitation, dyspnoea and pain can all be managed with the same anticipatory medications as recommended.20 Specifically relating to PD, several case reports have supported the intraoperative use of midazolam, during sedation, for tremor and dyskinesias,23,24 as well as for agitation at the end of life.20
Read Also: Can Parkinson’s Be Detected By Mri
Starting Palliative Care In Patients With Pd
Patients with PD benefit early from palliative care in view of the impact of the disease impairing autonomy and quality of life. The provision of palliative care in patients with PD focuses on unmet needs and should be aligned with patient priorities. It is recommended that a palliative care approach should be applied from the early phase, throughout the course of the disease, complementing but not replacing other treatments . However, like other patients with chronic neurological condition, the individual needs may vary over time, therefore it is suggested that a model of dynamic involvement of palliative care services should be adopted . The services can be triggered at times of particular symptoms or psychosocial issuessuch as the start of new interventions or at the very end of life.
For patients with complex physical, social, psychological and/or spiritual needs that do not respond to simple or established protocols of palliative care, there should be access to the support from specialist palliative care service .
However, rate of use of hospice in PD patients has been low . Caregivers often considered palliative care services to be synonymous with hospice care, and hence they did not consider this service option . Health care workers also have uncertainty about timing of palliative care, such that it was often not introduced until a crisis point .
Hospice Care For Patients With End Stage Parkinsons Disease
The goal of hospice services is to provide a quality, peaceful death while allowing the person with Parkinson Disease to remain in a familiar environment such as their home, assisted living or long-term care facility. Hospice provides ongoing education related to caring for a loved at home. It can be overwhelming to care for a loved one that is no longer able to do the things that they normally were able to do in the earlier stages of the disease. Unfortunately, in the later stages of PD patients eventually lose the ability to care for themselves and require assistance with most activities of daily living. Some families struggle seeing their loved ones deteriorate and often feel helpless as PD symptoms are irreversible. Unfortunately, there is no cure for PD but certain medications have been approved to help with symptoms and slow down the progression of the disease.
Also Check: How Early Can Parkinson’s Disease Be Detected
Theory Of Pd Progression: Braaks Hypothesis
The current theory is that the earliest signs of Parkinsons are found in the enteric nervous system, the medulla and the olfactory bulb, which controls sense of smell. Under this theory, Parkinsons only progresses to the substantia nigra and cortex over time.
This theory is increasingly borne out by evidence that non-motor symptoms, such as a loss of sense of smell , sleep disorders and constipation may precede the motor features of the disease by several years. For this reason, researchers are increasingly focused on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Ryan Barmore, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
Also Check: What Medications Can Cause Parkinsons
Hospice Care Late Stage Parkinsons
It is important to know your options for hospice care for late stage Parkinsons patients. Our article regarding in home health care for Parkinsons explains some of the basic facts and ideas to maintain quality of life once diagnosed. However, we offer specialized in home care from diagnosis through the final stages of the disease.
The Life of Parkinsons Crossing the bridges & facing forks in the road. Get the most out of life and adjust your lifestyle to make every day as good as possible.
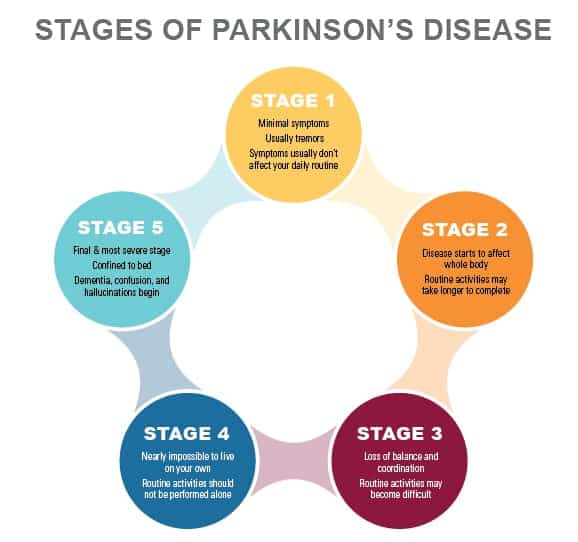
Parkinsons disease is degenerative. Because the disease progresses with time there are basic stages that occur.
Don’t Miss: Diseases That Mimic Parkinson’s
Stage Four: Symptoms Are Severe And Disabling And You Often Need Assistance To Walk Stand And Move
Stage Four Parkinsons disease is often called advanced Parkinsons disease. People in this stage experience severe and debilitating symptoms. Motor symptoms, such as rigidity and bradykinesia, are visible and difficult to overcome. Most people in Stage Four arent able to live alone. They need the assistance of a caregiver or home health aide to perform normal tasks.
How Is Parkinson Disease Treated
Parkinson disease cant be cured. But there are different therapies that can help control symptoms. Many of the medicines used to treat Parkinson disease help to offset the loss of the chemical dopamine in the brain. Most of these medicines help manage symptoms quite successfully.
A procedure called deep brain stimulation may also be used to treat Parkinson disease. It sends electrical impulses into the brain to help control tremors and twitching movements. Some people may need surgery to manage Parkinson disease symptoms. Surgery may involve destroying small areas of brain tissue responsible for the symptoms. However, these surgeries are rarely done since deep brain stimulation is now available.
Read Also: Is Psp Worse Than Parkinsons
Also Check: How Many Stages In Parkinson’s Disease
How Can I Support Someone With Parkinson’s Towards The End Of Life
In the advanced stages of Parkinsons, your patients care needs may be more complex and require careful planning along with the patient, their family and other health and social care professionals involved.
Palliative care should be holistic, considering the whole person to support the personal, social, psychological and spiritual needs of your patient and their family. It should give your patient some control and choice over areas such as treatment options and where they will be cared for, as well as providing advice and support to all the people involved in their care.
Palliative care in Parkinsons may be supported by a number of professionals, including a Parkinsons nurse specialist, local hospice or specialist palliative care team, physiotherapist, occupational therapist, speech and language therapist or dietitian. Many people with Parkinson’s also find complementary therapies beneficial.
It is important that you find out whether the person has a care plan in place regarding their preferences for how the issues surrounding advanced Parkinsons should be managed. This could include legal documentation such as a Lasting Power of Attorney and an advance care plan. Advance care plans include information on what the persons wishes and preferences are for their care in the future. They may include decisions on any treatments the person does not want to have in the future this is called an Advance Directive, Advance Decision to Refuse Treatment or Living Will.
My Parkinsons Story: Advanced Parkinsons
This 10-minute video alternates between an interview with a man and his wife and his palliative care team, including a doctor, nurse, clerg and social worker. The man and his wife shares his experience with late stage Parkinsons. The palliative care team explains that their job is to support the best physical, emotional and spiritual wellbeing of the immediate family as well as help the family make end of life decisions.
Also Check: Can Young People Get Parkinson’s
A Guide To Understanding End
Crossroads Hospice & Palliative Care created guidelines to help family caregivers better understand the physical changes of the end-of-life process, as well as the emotional and spiritual end-of-life changes taking place.
The following describes the physical symptoms you may observe. Here are end-of-life signs and helpful tips:
Pdd Vs Dementia With Lewy Bodies
Another type of dementia is called Dementia with Lewy Bodies , which has similar symptoms to PDD. DLB is associated with abnormal deposits of a protein called alpha-synuclein in the brain. Lewy bodies are also found in the brains of people diagnosed with PDD.
However, DLB is diagnosed when cognitive decline happens before the motor symptoms of Parkinsons, or when motor symptoms and cognitive decline occur and progress closely together.
Don’t Miss: How Long Can A Person Live With Stage 5 Parkinson
What Can I Expect If I Have This Condition
Parkinsons disease is a degenerative condition, meaning the effects on your brain get worse over time. However, this condition usually takes time to get worse. Most people have a normal life span with this condition.
Youll need little to no help in the earlier stages and can keep living independently. As the effects worsen, youll need medication to limit how the symptoms affect you. Most medications, especially levodopa, are moderately or even very effective once your provider finds the minimum dose you need to treat your symptoms.
Most of the effects and symptoms are manageable with treatment, but the treatments become less effective and more complicated over time. Living independently will also become more and more difficult as the disease worsens.
How long does Parkinsons disease last?
Parkinsons disease isnt curable, which means its a permanent, life-long condition.
Whats the outlook for Parkinsons disease?
Parkinsons disease isnt fatal, but the symptoms and effects are often contributing factors to death. The average life expectancy for Parkinsons disease in 1967 was a little under 10 years. Since then, the average life expectancy has increased by about 55%, rising to more than 14.5 years. That, combined with the fact that Parkinsons diagnosis is much more likely after age 60, means this condition doesnt often affect your life expectancy by more than a few years .
How Is Parkinsons Disease Dementia Diagnosed
No single test can diagnose Parkinsons disease dementia. Instead, doctors rely on a series or combination of tests and indicators.
Your neurologist will likely diagnose you with Parkinsons and then track your progression. They may monitor you for signs of dementia. As you get older, your risk for Parkinsons dementia increases.
Your doctor is more likely to conduct regular testing to monitor your cognitive functions, memory recall, and mental health.
Read Also: How Long Does A Person Live With Parkinson’s Disease
Many Techniques Used Include:
- Shifting patients every two hours. Adjusting how patients are seated or supine helps prevent their weight from opening wounds on the skin.
- Toileting. Besides walking patients to the bathroom, caregivers help them undress and clean up afterwards.
- Changing diapers. If the patient is confined to bed, their diapers need to be checked and changed every two hours to prevent serious infections.
- Bathing and grooming. Patients who cant get in and out of the shower require sponge baths. Patients also need help trimming their nails, combing their hair, and brushing their teeth.
- Assistance with eating. Eating can be very challenging for patients. Caregivers may have to push patients to eat, offering small portions of whatever foods they can consume. Because of difficulties experienced when chewing and swallowing, soft foods may be all they can eat at this stage. Oatmeal, scrambled eggs, yogurt, applesauce, mashed potatoes, and smoothies are frequent choices solid food is cut up into bite-sized pieces to ensure patients can eat safely.
- Keeping patients hydrated. Patients need to drink 6-10 glasses of water a day to stay properly hydrated. Caregivers assist with the process, holding bottles, cups and straws as needed.
- Organizing medications. Patients are usually prescribed several medications to reduce shakes and control movement. Medications need to be carefully organized and all caregivers need to be briefed on their instructions.
What Are The Symptoms Of Parkinson’s Towards The End Of Life
Parkinsons progresses in stages: diagnosis, maintenance, advanced and palliative. Professionals should have talk to people with Parkinsons about advance care planning in the earlier stages of the disease. This can allow them to express their wishes and preferences for their care in the later stages of the disease and make plans for the future.
Although the condition progresses differently and at a different speed for each person, the advanced stage can potentially cover a long period of time.
Problems that affect someone with advanced Parkinsons may include:
- medicines being less effective at managing symptoms than before
- having to take lots of medicines to manage symptoms and side effects
- more off periods when the effects of medication are reduced, and people experience movement fluctuations and involuntary movements
- increased mobility problems and falls
- swallowing difficulties
- less control of their Parkinsons symptoms, which become less predictable
Some of the more advanced symptoms can lead to increased disability and poor health, which can make someone more vulnerable to infection, such as pneumonia. People with Parkinsons most often die because of an infection or another condition, usually caused by Parkinsons.
Don’t Miss: The New Definition And Diagnostic Criteria Of Parkinson’s Disease
