What Is Needed To Meet These Challenges
Progress of the recent years was only possible due to sincere and open-minded collaboration of many scientists in different fields. We will need to further combine forces. Cohort studies will need to cross epidemiological, clinical and basic science boundaries, so that we move beyond clinical markers of prodromal disease. Harmonization of assessments, an integrative attitude towards other disciplines, and deeper data sharing and analyses will be essential.
Last, but definitely not least, the current criteria are established as research criteria and have been mainly disseminated to specialists in the field. However, advances in this field are not hidden in our information society. As the general public begins to grasp our evolving understanding of early PD stages, new challenges will emerge related to potential for harm. Identifying oneself or ones loved one as being in prodromal stages of neurodegeneration, without any preventative treatment can lead to excessive distress, overplanning , use of unproven preventative therapies, discrimination at work, inability to obtain insurance, etc. Until preventative therapy is developed, we must become increasingly prepared to help those directly affected by our research findings.
I Have Pd And Several Symptoms Should I Get A Datscan
Likely no. There is no need for DaTscan when your history and exam suggest Parkinsons disease and you meet the diagnostic criteria. Occasionally, if signs and symptoms are mild or you dont meet the diagnostic criteria, your doctor will refer you for a DaT scan. Keep in mind that ultimately the diagnosis is based on your history and physical exam. The DaT scan is most commonly used to complete the picture and is not a test for a diagnosis.
The Perilous Concept Of Prodromal Pd
Based on these data, prodromal PD criteria represent a promising tool for research purposes, to better investigate the possible risk to develop PD in presymptomatic patients. However, future methods to detect prodromal PD likely will require a multivariate hierarchical approach, and its power will depend on accessing markers over multiple possibly independent domains, such as genetic features, motor and non-motor symptoms, and ancillary diagnostic tests . Nonetheless, further investigations are requested to better understand the effective role of the different markers in research studies, such as those which have been recently conducted in REM SBD patients in order to identify new potential -synuclein biomarkers .
Read Also: Focused Ultrasound Therapy For Parkinson’s
Definition Of Terms Used In The Analysis
Sensitivity: Proportion of patients with a final diagnosis of Parkinson’s disease who were previously diagnosed as having Parkinson’s disease: A/.
Specificity: Proportion of patients without a final diagnosis of Parkinson’s disease who were previously diagnosed as not having Parkinson’s disease: D/.
Positive predictive value: Proportion of patients with a previous diagnosis of Parkinson’s disease who received a final diagnosis of Parkinson’s disease: A/.
Negative predictive value: Proportion of patients with a previous diagnosis of not having Parkinson’s disease who received a final diagnosis of not having Parkinson’s disease: D/.
Motor Circuit In Parkinson Disease
The basal ganglia motor circuit modulates the cortical output necessary for normal movement .
Signals from the cerebral cortex are processed through the basal ganglia-thalamocortical motor circuit and return to the same area via a feedback pathway. Output from the motor circuit is directed through the internal segment of the globus pallidus and the substantia nigra pars reticulata . This inhibitory output is directed to the thalamocortical pathway and suppresses movement.
Two pathways exist within the basal ganglia circuit, the direct and indirect pathways, as follows:
-
In the direct pathway, outflow from the striatum directly inhibits the GPi and SNr striatal neurons containing D1 receptors constitute the direct pathway and project to the GPi/SNr
-
The indirect pathway contains inhibitory connections between the striatum and the external segment of the globus pallidus and between the GPe and the subthalamic nucleus striatal neurons with D2 receptors are part of the indirect pathway and project to the GPe
The STN exerts an excitatory influence on the GPi and SNr. The GPi/SNr sends inhibitory output to the ventral lateral nucleus of the thalamus. Dopamine is released from nigrostriatal neurons to activate the direct pathway and inhibit the indirect pathway. In Parkinson disease, decreased striatal dopamine causes increased inhibitory output from the GPi/SNr via both the direct and indirect pathways .
Read Also: What Pesticides Are Linked To Parkinson’s Disease
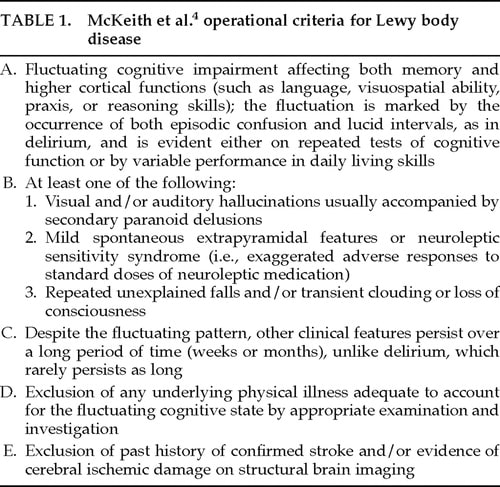
The Evolution Of Critical Symptoms Involved In Diagnostic Procedures Of Pd
- Diagnostic criteria: presence of bradykinesia and at least one of the following symptoms: muscular rigidity, 46 Hz rest tremor and postural instability
- Exclusion criteria: history of repeated strokes or head injury, encephalitis, early severe autonomic involvement or dementia, Babinski sign, negative response to levodopa treatment and MPTP exposure
- Supportive criteria : unilateral onset, rest tremor, progressive course, persistent asymmetry, excellent response to dopaminergic therapy, levodopa-induced dyskinesia, positive levodopa response five years or more and clinical course of ten years or more
Patients With A Previous Diagnosis Other Than Parkinson’s Disease
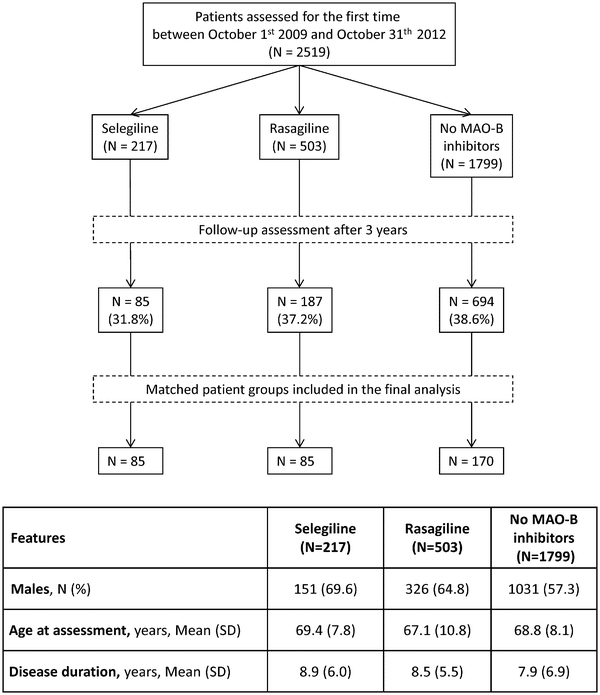
Among all patients seen, two were referred for diagnostic purposes without a previous diagnosis, and 69 of 202 patients had a previous diagnosis other than Parkinson’s disease . Among these, 56 patients had been given a diagnosis of non-parkinsonian tremor, two of vascular parkinsonism, one of atypical parkinsonism, and 10 had been prescribed an antiparkinsonian drug for parkinsonian features without a specific diagnosis . Thirteen of the 69 patients with different diagnoses and the two patients referred for diagnostic purposes fulfilled strict clinical criteria for Parkinson’s disease . In two additional patients who had a previous diagnosis of non-parkinsonian tremor, a diagnosis of possible Parkinson’s disease was made . If only patients who had at some point in the past seen a specialist were considered, the diagnosis was changed to probable Parkinson’s disease in five and to possible Parkinson’s disease in one .
Sensitivity, specificity, and predictive values for the overall sample* and by type of clinician
Recommended Reading: What Does Parkinson’s Affect
Predictive Values For Clinical Diagnoses Under Different Scenarios
demonstrates how the positive and negative predictive values for each of the main three diagnoses vary as the prevalence of the specific diagnosis alters. The most dramatic effect is seen for IPD, which had a negative predictive value of 90% in the UKPDSBRC sample. When applied to a normal population sample, where IPD is a priori likely to be the most likely diagnosis, this propensity to overdiagnose less common causes of parkinsonism amongst pathologically proven IPD has an important detrimental effect on the negative predictive value. In absolute terms, however, this would still only result in 81 falsenegative diagnoses in every 1000 cases. The relatively good positive predictive values for both MSA and PSP are markedly attenuated in the community sample, where these disorders are far less common. The clinical predictive value in Table , scenario 3, designed to reflect a specialist movement disorder clinic, is much more like that observed from the UKPDSBRC sample.
Brief Survey Among Movement Disorder Experts
Figure 1. Schematic representation of the three questions posed to the movement disorder experts during the brief survey.
Figure 2. Schematic representation of the senior movement disorder experts answers to the three questions of the brief survey. Legend: Y, yes N, no NA, not available.
This informal brief survey provides current simple information about real-life differences in the approach to the clinical diagnosis of PD among clinicians. Possible limitations of the here reported international audit consist the restricted number of participants and that only experts not directly involved in the production of the criteria have been interviewed, configuring a possible negative bias. In summary, we suggest that the diffusion of the new criteria should be better implemented not only among general neurologists, but also among movement disorders specialists. Although the revised MDS-PD criteria have been published since 2015, many colleagues do not apply these criteria in routine clinical practice because of scarce knowledge and probably also for some prejudices.
Recommended Reading: Does Parkinson’s Affect Your Eyes
Patients In Whom A Diagnosis Of Parkinson’s Disease Was Or Was Not Previously Made
Patients in whom a diagnosis of Parkinson’s disease was previously made had a longer disease duration and greater disease severity , with more severe akinesia , postural instability, and rigidity than those in whom the diagnosis was not made before. They were also more likely to be depressed , to have experienced dyskinesias , and to live alone or with their family than in a nursing home .
From Prodromal To Overt Parkinsons Disease: Towards A New Definition In The Year 2040
Issue title: The Times They Are a-Changin: Parkinsons Disease 20 Years from Now
Guest editors: Patrik Brundin, J. William Langston and Bastiaan R. Bloem
Article type: Review Article
Authors: Berg, Danielaa b * | Postuma, Ronald B.c *
Affiliations: Department of Neurology, Christian-Albrechts-University of Kiel, Kiel, Germany | Department of Neurodegeneration, Hertie-Institute for Clinical Brain Research Tuebingen, Germany | Department of Neurology, Montreal General Hospital, Montreal, Quebec, Canada
Correspondence: Correspondence to: Daniela Berg, MD, Department of Neurology, Christian-Albrechts-University of Kiel, Arnold-Heller-Str. 3 24105 Kiel, Germany. E-mail: . and Ronald B. Postuma, MD, MSc, Department of Neurology, L7-305 Montreal General Hospital, 1650 Cedar Ave, Montreal, Canada H3G1A4. E-mail: .
Keywords: Prodromal Parkinsons disease, higher-specificity markers, big data approaches, progression markers, subtypes, population-based screening, neuroprotective trials, gene-specific therapy, individual mechanism-specific therapy
DOI: 10.3233/JPD-181457
Journal: Journal of Parkinson’s Disease, vol. 8, no. s1, pp. S19-S23, 2018
Abstract
Recommended Reading: How Does Parkinson’s Work
Likelihood Of Referral According To Final Diagnosis
Overall, 74% of all cases with a diagnosis of Parkinson’s disease had been seen by a specialist. However, when these cases were classified by final diagnosis , it was observed that, paradoxically, fewer cases with atypical disease had been seen by a specialist compared with those with classical Parkinson’s disease p = 0.02).
Sensitivity Specificity And Predictive Value Of A Previous Diagnosis Of Parkinson’s Disease
Of 126 patients with a pre-existing clinical diagnosis of probable and possible Parkinson’s disease in the overall sample , 111 were confirmed as having Parkinson’s disease, resulting in a sensitivity of 88.1% similarly, it was confirmed that 54 of 74 patients did not have Parkinson’s disease, resulting in a specificity of 73.0% . The positive and negative predictive values of a previous clinical diagnosis of Parkinson’s disease were 84.7% and 78.3% . In other words, in 85% of patients with a previous diagnosis of Parkinson’s disease this diagnosis was confirmed, and 78% of patients with a diagnosis other than Parkinson’s disease did not have the disease .
When this was broken down by a specialist or other doctor diagnosis, the diagnostic validity was as follows. Neurologists and geriatricians had a sensitivity and specificity of 93.5% and 64.5% , respectively, compared with 73.5% and 79.1% for non-specialists. The positive predictive values were greater for specialists than for other doctors , but the negative predictive values were equivalent v non-specialist 79.1% ).
You May Like: What Disease Is Like Parkinson’s
Utility Of The New Movement Disorder Society Clinical Diagnostic Criteria For Parkinson’s Disease Applied Retrospectively In A Large Cohort Study Of Recent Onset Cases
The MDS diagnostic criteria for Parkinson’s Disease were tested retrospectively in a large cohort study.
-
Over 90% of cases diagnosed clinically as PD fulfilled MDS diagnostic criteria for PD.
-
Over 60% were categorized Clinically established PD under 30% were Clinically probable PD.
-
Cases categorized as not PD had more severe, less therapy responsive parkinsonism.
-
Categorization as PD by the MDS criteria was 85% stable after 2.5 years of follow-up.
Diagnostic Parameters For The Main Clinical Diagnoses
Overall, 122 out of 143 cases were clinically diagnosed correctly, giving an overall positive predictive value of 85.3% . Other than vascular parkinsonism, which was based on two cases, the clinical diagnosis of IPD showed the best overall sensitivity and positive predictive value , followed by MSA and then PSP. The figures for CBD and vascular parkinsonism are based on very small numbers. The specificity for all the major diagnoses was extremely high with little difference for any of the groups, indicating that these neurologists were extremely good at correctly ruling out these specific diagnoses.
Read Also: What Helps With Parkinson’s Disease
Limitations And Shortcomings Of The Current Understanding And Model
The prodromal PD criteria are meant to be research criteria, and constitute a first step in what should be a continually-updated process.
Several shortcomings have been noted, both at the time of publication and as several groups have studied the criteria. These include:
This is even more significant as the current prodromal criteria are primarily based on clinical signs with no opportunity to include brain autopsy as ultimate diagnostic confirmation.
The New Definition And Diagnostic Criteria Of Parkinson’s Disease
@article, author=nther Deuschl and Thomas Gasser and Christopher G. Goetz and Glenda M. Halliday and Lawrence Joseph and Anthony E. Lang and Inga Liepelt-Scarfone and Irene Litvan and Kenneth Marek and Wolfgang Hermann Oertel and C. Warren Olanow and Werner Poewe and Matthew B. Stern}, journal=, year=, volume=, pages=}
- View 2 excerpts, cites methods and background
- Movement disorders : official journal of the Movement Disorder Society
- View 1 excerpt, cites background
- View 2 excerpts, cites background
- View 1 excerpt, cites background
- View 1 excerpt, cites background
- View 1 excerpt, cites background
- Movement disorders : official journal of the Movement Disorder Society
You May Like: Do All Parkinson’s Patients Have Lewy Bodies
Patients With A Previous Diagnosis Of Parkinson’s Disease
The diagnosis of probable Parkinson’s disease was confirmed in 109 of the 131 patients with this diagnosis , including three in whom atypical features were found but were insufficient to invalidate the diagnosis of Parkinson’s disease . Two additional patients were found to have possible Parkinson’s disease. However, in 20 of the 131 patients the diagnosis of Parkinson’s disease was unequivocally rejected . The alternative diagnoses were non-parkinsonian tremor in four patients , vascular parkinsonism in six , progressive supranuclear palsy in four , and multiple system atrophy in three . Two patients received a diagnosis of idiopathic torsion dystonia, and one of dementia without parkinsonism. When only those patients who had seen a specialist at some point in the past were considered, the diagnosis was changed from Parkinson’s disease to a different diagnosis in 11%.
Patients with an initial diagnosis of Parkinson’s disease
From The Ukpdsbb To The Gelb Diagnostic Criteria
Only one study directly compared sensitivity, specificity, PPV, negative predictive value , and accuracy of UKPDSBB and Gelb criteria with a definite diagnosis of PD . Diagnostic PPV and NPV were similar in UKPDSBB and Gelb criteria for possible and probable PD , while specificity was low in both criteria . Sensitivity was higher in UKPDSBB and Gelb criteria for possible PD compared to Gelb criteria for probable PD . Global accuracy was 84% for UKPDSBB criteria, 82% for Gelb criteria for possible PD, and 69% for Gelb criteria for probable PD , with a high number of false positive and false negative cases. In addition, two detailed systematic reviews on the diagnosis of PD carried out in Scotland , and Italy were unable to find comparative studies between the two diagnostic criteria and diagnoses of expert clinicians, except for the above-mentioned study by Hughes et al. in which it was only possible to compare PPV . However, a more recent meta-analysis indicated that the accuracy of the clinical diagnosis by an expert is similar to UKPDSBB criteria , with a lower sensitivity , but higher specificity .
Recommended Reading: What Is Vascular Parkinson’s Disease
Rationale And Construct Of The Mds
In this view, in 2015 the ad hoc MDS task force proposed new clinical diagnostic criteria for PD . These criteria were specifically designed for use in research, but they also might be adopted as a general guide to the clinical diagnosis of PD in a routine setting . Examination of all cardinal manifestations should be carried out as described in the MDS-Unified Parkinson Disease Rating Scale . In the MDS-PD criteria, the classical signs of the motor syndrome remain the core features of the disease. The essential criterion is the presence of parkinsonism, which is defined as bradykinesia, in combination with at least one between rest tremor and rigidity . However, many non-motor manifestations, often dominating the clinical presentation of the disease, have now been incorporated into the diagnostic criteria . Based on the assumption that the pathological process of PD may begin in non-dopaminergic structures of the brain or peripheral nervous system, a new diagnostic category has been configured, prodromal PD : prodromal PD is considered to represent a true initial stage of PD .
Table 1. Supportive criteria, absolute exclusion criteria, and red flags for the diagnosis of Parkinsons disease, according to the revised International Parkinson and Movement Disorder Society diagnostic criteria .
Table 2 provides a brief synopsis reporting the main features of the different diagnostic criteria and guidelines developed to improve the diagnosis of PD.
Tests To Rule Out Other Conditions
Blood tests can help rule out other possible causes of the symptoms, such as abnormal thyroid hormone levels or liver damage.
An MRI or CT scan can check for signs of a stroke or brain tumor, which may cause similar symptoms.
Hydrocephalus due to atrophy can occur with some types of dementia and would be visible with one of these imaging tests. If the person has neurologic symptoms but a normal scan result, Parkinsons disease may be present.
The doctor a lumbar puncture to rule out inflammation or a brain infection.
Recommended Reading: Nyu Parkinson’s And Movement Disorders Center
New Diagnostics For Pd Might Allow Early Diagnosis Prevention
A new way of diagnosing Parkinsons disease based on manifestations that appear decades before motor symptoms the current hallmarks for diagnosis might allow early diagnosis and even prevention.
The study, From Prodromal to Overt Parkinsons Disease: Towards a New Definition in the Year 2040, was published in the Journal of Parkinsons Disease.
Parkinsons disease is characterized by progressive loss of coordination and movement. Currently, a person is diagnosed when those symptoms appear. However, there are some risk factors and symptoms that precede motor manifestations and constitute the early stages of the disease .
Brilliant work of many in different scientific fields has paved the way for the concept of prodromal that is, a phase of years to decades in which non-motor and subtle motor symptoms may indicate spreading PD pathology, but do not meet the threshold for diagnosis according to the classic motor-based clinical criteria, researchers said.
The development of new diagnostic criteria that allow the identification of prodromal Parkinsons might help to better understand disease progression, lead to early diagnosis and treatment, and prevent classic motor symptoms.
