Balance And The Brain
Difficulties with balance and walking are linked to the brain changes that take place with PD. For people who dont have PD, balance is automatic, a reflex. But Parkinsons affects the basal ganglia . To compensate, the brain assigns another brain area an area used for thinking to take over. The thinking part of the brain, mainly the frontal cortex, cant control balance automatically. The result: for many people with PD, balance becomes less automatic.
This means that when people experience freezing and fall, they cant adjust their balance automatically. Taking small steps to try and regain balance can make things worse, because it involves shifting weight with each step. The brain changes from PD inhibit their ability to take a big step to catch their balance and avoid a fall. For some, the drug levodopa can help prevent freezing, but does not improve balance.
A person whose balance is less automatic must pay more attention while walking. For everyone, walking slows down when were talking and thinking slows down when were walking. This is called the dual-task cost and its higher in people with PD. That tells us that people with PD are using more attention and more cognitive control for balance and gait.
Patients Grouped By Mmse
Table reports demographical and clinical data of patients subdivided according to MMSE.
Table 1. Demographical and clinical data of patients subdivided according to MMSE.
Passing from MMSE 2730 to MMSE 2126 and MMSE 20, age and H&Y significantly increased as the MMSE was lower and years of education decreased , while no difference was observed in levodopa equivalent dose . No relationships between baseline score on the MMSE and sex or the most affected side were found .
Figures reports admission and discharge values for all outcome variables, with differences and percentage change, for every MMSE group.
Figure 1. Admission, discharge and delta for all the outcome variables in patients grouped according to MMSE: Total UPDRS, UPDRS III, UPDRS II, 6MWT, BBS, TUG, PDDS. Data are reported as median , lower and upper quartile . The percentage value of delta is reported in brackets. The p values are pertaining to the comparison discharge vs. admission. Abbreviations: MMSE, Mini Mental State Examination; UPDRS, Unified Parkinsons Disease Rating Scale; 6MWT, Six Minutes Walking Test; BBS, Berg Balance Scale; TUG, Timed Up and Go Test; PDDS, Parkinsons Disease Disability Scale.
For the remaining outcome variables, namely UPDRS II, 6MWT and TUG no between groups significant differences were observed in the percentage changes .
Cognitive Impairment In Parkinson’s Disease: A Complex Picture
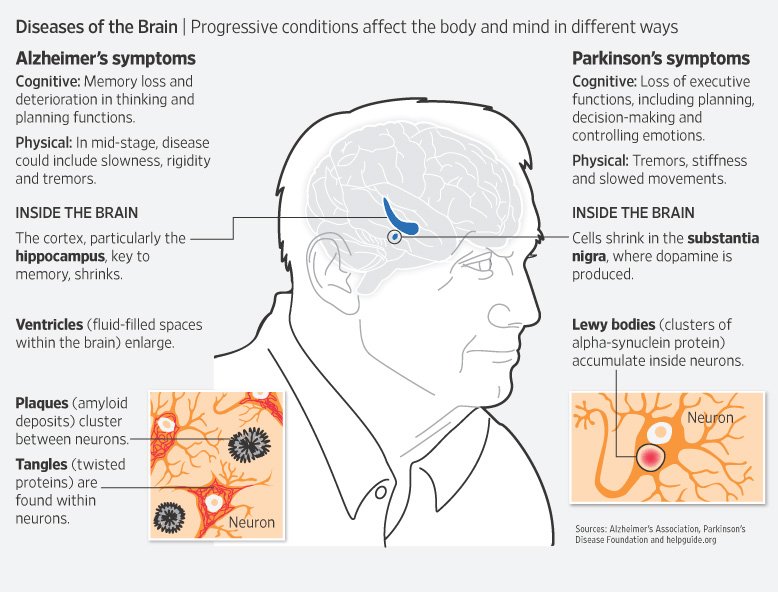
The presence of marked heterogeneity in neuropsychological deficits observed among PD patients makes it difficult to establish a comprehensive unique model for cognitive decline in PD . To understand the nature and evolution of these cognitive alterations it is important to interpret the interplay between cognitive, anatomical, neurochemical and neuropathological entities associated with these deficits. Indeed, intriguing overlaps in biochemical, clinical, and imaging findings among different conditions such as PD and Alzheimer’s disease question the concept of underlying mechanisms acting as distinct entities and instead suggest a continuum along which individuals express PD-typical patterns and AD-typical patterns to a variable degree. In this regard, metabolic imaging studies support the notion of Parkinson’s disease dementia and dementia with Lewy bodies as overlapping disease entities, characterized by the presence of mixed neuropathology and differentiated only by the time course of symptoms . Only few neuropathologic studies of PDMCI are available, but results suggest a heterogeneous pathologic basis for the cognitive deficits .
Can Parkinsons Disease Make You Aggressive
Parkinsons disease Dementia or PD Dementia can make a patient very aggressive. Parkinsons Dementia Aggression germinating from Parkinsons disease Dementia can lead patients to behave erratically, experience sudden anger outbursts, feel constantly irritated, and always be in a state of restlessness. Outbursts are generally in the form of:
- Shouting
- Falling
Want To Learn More About The Latest Research In Parkinsons Disease Ask Your Questions In Our Research Forum
Cognitive impairment can occur due to stress, particularly if the patient feels they are a burden to their caregiver, are experiencing a decline in daily functioning, have a worsening quality of life, are dealing with rising medical costs, or are concerned about their mortality.
According to the National Parkinson Foundation, some of the common cognitive issues people living with Parkinsons disease face include:
- Slowness of thinking
- Struggling to find the right words in conversations
- Declining visual perception
- Lack of reasoning skills
- Declining general intelligence
Some Parkinsons disease medications can help with areas such as motivation and concentration, but there are no medications that can improve memory function.
MORE:How does Parkinsons disease affect the brain?
Parkinsonss News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Neurochemical Deficits In Pdd
Degeneration of subcortical nuclei in PD leads to dopaminergic, cholinergic, noradrenergic, and serotoninergic deficits. Of them, cholinergic deficits due to degeneration of the nucleus basalis of Meynert have been the most involved in PDD. In early neuropathological studies, PDD patients showed more NMB cholinergic neuronal depletion when compared with AD and non-demented PD., A greater reduction of choline acetyltransferase activity in frontal and temporal cortex was found in PDD than in PD without dementia. Mattila et al reported reduced choline acetyltransferase activity in the hippocampus, prefrontal cortex, and temporal cortex in PD. Reduction in the frontal cortex correlated signicantly with the degree of cognitive impairment. Not only pathological studies but also neuroimaging studies have pointed out a role for a cholinergic deficit in cognition in PD. Both PD and PDD have cholinergic neuron decits with vesicular acetylcholine transporter and acetylcholinesterase , imaging being the decreased VAChT more important and extensive in the cerebral cortex of PDD subjects.
There are not consistent findings supporting an association between dementia and other monoaminergic systems.
Behaviors Seen In Parkinsons Disease Dementia
As dementia progresses, managing disorientation, confusion, agitation, and impulsivity can be a key component of care.
Some patients experience hallucinations or delusions as a complication of Parkinsons disease. These may be frightening and debilitating. Approximately 50 percent of those with the disease may experience them.
The best thing to do when giving care to someone experiencing hallucinations or delusions from Parkinsons disease dementia is to keep them calm and reduce their stress.
Take note of their symptoms and what they were doing before they exhibited signs of hallucinating and then let their doctor know.
This element of the disease can be particularly challenging for caregivers. Patients may become unable to care for themselves or be left alone.
Some ways to make caregiving easier include:
- sticking to a normal routine whenever possible
- being extra comforting after any medical procedures
- limiting distractions
- using curtains, nightlights, and clocks to help stick to a regular sleep schedule
- remembering that the behaviors are a factor of the disease and not the person
What Is Needed For A Parkinson’s Disease Dementia Diagnosis
There is no definitive medical test that confirms cognitive decline or dementia in Parkinson’s disease. The most accurate way to measure cognitive decline is through neuropsychological testing.
- The testing involves answering questions and performing tasks that have been carefully designed for this purpose. It is carried out by a specialist in this kind of testing.
- Neuropsychological testing addresses the individual’s appearance, mood, anxiety level, and experience of delusions or hallucinations.
- It assesses cognitive abilities such as memory, attention, orientation to time and place, use of language, and abilities to carry out various tasks and follow instructions.
- Reasoning, abstract thinking, and problem solving are tested.
- Neuropsychological testing gives a more accurate diagnosis of the problems and thus can help in treatment planning.
- The tests are repeated periodically to see how well treatment is working and check for new problems.
Imaging studies: Generally, brain scans such as CT scan and are of little use in diagnosing dementia in people with Parkinson’s disease. Positron emission tomographic scan may help distinguish dementia from depression and similar conditions in Parkinson’s disease.
Patients Grouped By Fab
The same analysis was carried out dividing patients according to FAB. Table reports basal values for demographical and clinical variables in patients with normal executive functions and pathological executive functions .
Table 2. Demographical and clinical data of patients subdivided according to FAB.
Passing from normal to pathological executive functions, age and H&Y significantly increased , years of education decreased , while no difference was observed in levodopa equivalent dose . No different distribution of sex and most affected side was found .
Figures reports admission and discharge values for all outcome variables, with differences and percentage change, for both groups.
Figure 2. Admission, discharge and delta for all the outcome variables in patients grouped according to frontal assessment battery : Total UPDRS, UPDRS III, UPDRS II, 6MWT, BBS, TUG, PDDS. Data are reported as median , lower and upper quartile . The percentage value of delta is reported in brackets. The p values are pertaining to the comparison discharge vs. admission. Abbreviations: MMSE, Mini Mental State Examination; UPDRS, Unified Parkinsons Disease Rating Scale; 6MWT, Six Minutes Walking Test; BBS, Berg Balance Scale; TUG, Timed Up and Go Test; PDDS, Parkinsons Disease Disability Scale.
How Can I Help Myself
Keeping physically active and mentally stimulated is very important when living with both Parkinsons and cognitive problems.
Avoiding stress is also important. Anything that puts you under pressure is likely to worsen memory problems, so try to take each day at a steady pace. Allow time for rest and relaxation, and make time to do the things you enjoy. Relaxing effectively can help to improve your concentration, attention span and ability to plan. Complementary therapies such as yoga and Tai Chi, together with exercise such as swimming may help with this.
We can all be forgetful and while this is often frustrating, a good quality of life can still be enjoyed if you make some adaptations.
You could begin by adapting your home and work environments to accommodate your needs. For example, removing clutter will reduce the number of visual distractions and make it easier for you to find your way around. Keeping furniture in the same place and having a regular daily routine may be helpful. At night, you may find it useful to keep a low-level night light on to minimise possible disorientation if you wake.
As time passes, carrying out more complex tasks is likely to become harder. Try writing down the various steps you have to go through in order to complete specific tasks, and follow these steps one by one.
The following tips may also help maintain brain function and improve quality of life:
Cognitive Interventions: Can They Help Cognition In Pd
There are several different types of cognitive interventions. Cognitive remediation or rehabilitation techniques include broad, multi-component approaches typically aimed at recovering an individuals abilities in the face of loss . Some approaches may be indirect ,,, and others involve multifaceted therapeutic techniques such as combining cognitive training, support groups, wellness education, and/or mental health counseling. Cognitive training refers to specific brain exercises that involve targeted practice with the goal of improving particular cognitive abilities and by using different cognitive training techniques or strategies . Cognitive training is based on the idea that cognitive functions can be strengthened over time with practice, similar to physical exercise strengthening muscles. Non-pharmacological approaches like cognitive training are of great interest, due to their potential to alleviate cognitive symptoms, provide individualized approaches, and avoid medication side effects. However, there has been rising public concern that many programs and products claim to stave off cognitive decline and dementia. Commissioned experts evaluated the science behind these interventions and noted that cognitive training was one of the few interventions to receive a positive recommendation and encouraging evidence from the National Academies of Sciences, Engineering, and Medicine committee.
Care Partners: Burden Assessment And Support
Care partners or caregivers are an invaluable healthcare resource. When caregivers are present, patients are less likely to move to nursing homes. Caregivers also improve participation rates and retention of people with PD in research studies, which helps advance the path towards finding more effective therapeutics. Furthermore, many clinical trials for PDD require a caregiver in the study inclusion criteria.
Informal caregivers are providers who supervise or assist with instrumental and/or basic activities of daily living without pay to someone who cannot do these activities independently due to cognitive, physical, or psychological impairment. However, caregivers provide much more than this formal definition states. They often provide medical care including administration of medications, emotional and social support, and advice on medical decision-making. About 90% of men and 80% of women with PD have caregivers during their physician visits, and most caregivers are spouses.
Despite existing therapeutic support and resources for caregivers, there are several challenges to overcome. These include sex disparities in caregiving and the substantial financial strain that can be associated with caregiving. Caregivers are frequently at the forefront of providing medical history and administering complicated medication regimens without formalized education or support.
What Are Parkinson’s Disease Dementia Medical Treatment And Medications

There is no specific therapy for dementia in Parkinson’s disease. Although cognitive symptoms initially may appear to respond to drugs that promote dopamine production, the improvement is mild and transient in contrast to the early responses to motor control improvement with medication in patients with Parkinson’s disease.
Parkinson’s disease dementia medications
Various medications are used to treat the movement disorders of Parkinson’s disease, some may exacerbate symptoms related to dementia.
- These include dopamine given in the form of levodopa; medications known as dopamine agonists that act on the dopamine receptor; and medications that slow down the metabolism of dopamine. They are often used in conjunction with monoamine oxidase inhibitors such as . In addition, anticholinergic drugs are sometimes used.
- Unfortunately, these drugs may affect cognitive symptoms and mood disorders.
- The anticholinergic drugs, for example, help balance levels of dopamine and acetylcholine, another neurotransmitter, in the brain. These drugs can improve movement disorders but often make memory loss worse.
The dementia of Parkinson’s disease may respond to drugs used in patients with disease. However, these drugs, called cholinesterase inhibitors , lead to only small and temporary improvements in cognition.
Mood disorders and psychoses are usually treated with other medication.
The Route To Better Walking
The good news for people with PD is that with exercise and physical therapy it is possible to cope better with freezing, turn and walk more normally and improve balance. Through practice and sessions, a physical therapist can help people with PD avoid tripping by helping them learn to take larger steps. Additionally, joining an exercise class tailored to people with PD can help. If you take levodopa, be sure to exercise while it is working the drug helps your body learn and remember motor skills.
Tricks that can help overcome freezing:
- Walk to a regular beat to help prevent freezing. Try a metronome.
- Take large, voluntary marching steps.
- Step over an imaginary line or laser pointer.
- Work with a therapist to find the solution that works best for you.
People respond differently to audio, visual or sensory cues. Dr. Horak and her team are testing a device that provides sensory feedback vibration on the foot to stimulate automatic stepping.
Another consideration for people who have freezing is anxiety, a common PD symptom. People who have anxiety experience freezing more often. It is a vicious circle being anxious about freezing can trigger it. Treating anxiety may help freezing.
What Is Aggressive Parkinsons Disease
As written above, Parkinsons dementia aggression is that form of Parkinsons which makes the patient exhibit aggressive behavior. They vent out their aggression either verbally or physically, in the various forms that have been written above. Besides verbal and physical outbursts, PD Dementia patients are also prone to hallucinating caused by the medication administered. Hallucinations in PD Dementia patients primarily occur because of the effects of dopaminergic agents for motor symptoms.
Loss of dopamine neurons in the ventral tegmental area is one of the likeliest of all neuropathological causes as changes in serotonin and norepinephrine systems are not. For the uninitiated, the ventral tegmental area is the origin of the mesolimbic dopaminergic projection. Plenty of studies have gone into analyzing the cause behind the aggression in PD Dementia patients. Depression in PD Dementia patients has been identified due to changes in the medial frontal cortex and the anterior cingulate. Akinetic-rigid variants have been found in patients showing signs of major depression.
What Is Parkinsons Disease
Parkinsons disease is a progressive brain disorder that affects mobility and mental ability. If you or a loved one has been diagnosed with Parkinsons, you may be wondering about life expectancy.
According to some , on average, people with Parkinsons can expect to live almost as long as those who dont have the condition.
Frontiers In Aging Neuroscience
National Hospital Organization Sendai Nishitaga Hospital, Japan
Reviewed by
Masahiko Tomiyam
Department of Neurology, Aomori Prefectural Central Hospital
The editor and reviewers’ affiliations are the latest provided on their Loop research profiles and may not reflect their situation at the time of review.
TABLE OF CONTENTS
Suggestions And Future Directions
These recent studies are encouraging and provide preliminary evidence supporting exercise effects on a variety of aspects of cognition for those with PD. However these findings must be replicated in phase III clinical trials. Further, all of these studies employed a range of cognitive outcome tasks, and improvements were limited to one or two executive function measures. Additionally, the number and size of the published studies of exercise effects in PD are limited, rendering definitive conclusions difficult to make. Based on evidence presented here, evaluating exercise’s effects on particular aspects of cognitive function that are implicated in PD is recommended. Such investigation should include tests of well-defined executive functions and language outcomes. Examining the effects of exercise over both longer and shorter intervals and doses, and more randomized clinical trials are necessary to elucidate which symptoms of PD are amenable to change. In particular, if the goal is to examine neural mechanisms of plasticity and improvement, observing changes in a range of cognitive and motor abilities in a group of PD participants over 6 month, or better, 12 month intervals is necessary. These recommendations, if observed, will begin to bring the research on exercise in PD in line with previous exercise research completed in older adults .
Perspectives On Cognitive Impairment From People With Parkinsons Disease And Care Partners In The Working Group
Quotes from people with PD:
Sometimes my brain freezes up, kind of like my legs sometimes do. Finding the words I want to say is very hard, and my thoughts seem like they are blank.
I wish that the doctor had told me that cognitive changes could be one of the results of the disease. My clinic visits have focused much more on physical signs and symptoms. The few times cognition has been addressed, the comments were very brief.
Quotes from PD care partners:
The most bothersome is attention, which we call chasing rabbits at our house. Early on this manifested as flitting from task to task without completion. However, cognitive symptoms have started to affect communication, which in turn affects our relationship. My husbands frustration in turn sparks irritation in both of us. I sometimes wonder if the same is not occurring with friends, and they are too polite to tell me.
My husband has lost his initiative in social situations. He listens but rarely contributes and may get confused in the conversation. I miss the social interactions that we used to have with friends with little planning. With just a suggestion, it used to happen.
Table 1 Questions for working group members
Association Between Cognitive Impairment And Motor And Non
In the first regression model , with cognitive impairment as dependent variable, two variables were found to be significant. Hoehn and Yahr stage and the motor exploration subscale in SCOPA-Motor scale showed a positive association with cognitive dysfunction. This model explained 49.0% of the variance.
Table 4. Binary logistic regression model for normal cognition vs. cognitive impairment .
The second regression model , with dementia as dependent variable, showed that dementia was positively associated with higher age and disease duration , an increased score in HADS-D , and more hallucination symptoms . The motor complications SCOPA-Motor subscale was negatively associated with the presence of dementia. This model explained 63.5% of the variance.
Table 5. Binary logistic regression model for dementia vs. no dementia .
Finally, in the multinomial model , there was a positive association between the presence of PD-MCI and HY stage . On the other hand, age , HY stage , and the depression HADS subscale were positively associated with the PDD group, whereas years of education was negatively associated. This model explained 61.6% of the variance.
Table 6. Multinomial logistic regression model .
Clinical Management Of Cognitively Impaired Pd Patients: The Role Of Non
Several largely sub-optimal pharmacological options have been tested for the treatment of cognitive impairment in PD, particularly for PDD. The positive effects of levodopa therapy could be either linked to general factors such as alertness, mood, and arousal or to more specific aspects of information processing, working memory, or internal control of attention . These beneficial effects of levodopa, however, may be complicated by adverse effects such as confusion and psychosis, more prominent in demented patients . So far, rivastigmine is the only drug approved by the Food and Drug Administration for PDD . The efficacy of Rivastigmine in PDD was demonstrated in a large randomized clinical trial , namely the EXPRESS study . This study demonstrated improvements in 541 PDD both in global cognition , as well as attention and executive functions from baseline to follow-up . However, the incidence of adverse events was also higher in the treatment than the placebo group. Given adverse events with pharmacotherapy, one might consider non-pharmacologic therapies as alternative, and if efficacious perhaps preferable, first-line treatment of cognitive impairment. Medications might then be used only after non-pharmacologic therapy has failed .
Ways To Decrease The Risk Of Parkinsons And Alzheimers
There is currently no cure for either disease. Parkinsons is considered a more treatable condition, however, especially in the early stages of the disease. Treatments include medication, physical therapy, and lifestyle modifications such as dietary changes. Research continues to suggest that a brain-healthy lifestyle can help prevent both Alzheimers and Parkinson’s. Here are some basic guidelines:
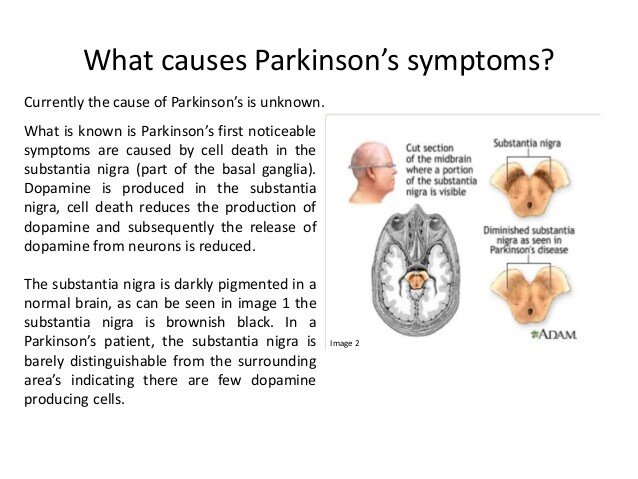
What Causes Parkinson Disease
Parkinson disease arises from decreased dopamine production in the brain. The absence of dopamine makes it hard for the brain to coordinate muscle movements. Low dopamine also contributes to mood and cognitive problems later in the course of the disease. Experts don’t know what triggers the development of Parkinson disease most of the time. Early onset Parkinson disease is often inherited and is the result of certain gene defects.
