Treatment Of Atrial Fibrillation And Wpw Syndrome
-
Direct-current cardioversion
The treatment of choice for Wolff-Parkinson-White syndrome is direct-current cardioversion Direct-Current Cardioversion-Defibrillation The need for treatment of arrhythmias depends on the symptoms and the seriousness of the arrhythmia. Treatment is directed at causes. If necessary, direct antiarrhythmic therapy, including antiarrhythmic… read more . The usual rate-slowing drugs used in atrial fibrillation are not effective, and digoxin and the nondihydropyridine calcium channel blockers are contraindicated because they may increase the ventricular rate and cause ventricular fibrillation. If cardioversion is impossible, drugs that prolong the refractory period of the accessory connection should be used. IV procainamide or amiodarone is preferred, but any class Ia, class Ic, or class III antiarrhythmic drug Drugs for Arrhythmias The need for treatment of arrhythmias depends on the symptoms and the seriousness of the arrhythmia. Treatment is directed at causes. If necessary, direct antiarrhythmic therapy, including antiarrhythmic… read more can be used.
Key Points About Wpw Syndrome
- WPW syndrome is a rapid heartbeat due to an extra electrical pathway connecting the upper and lower chambers of the heart.
- While some people might not experience WPW syndrome, those who do can experience fainting, tiredness, and shortness of breath. These symptoms can disappear over time but can be treated by your doctor through medication or surgery.
- WPW is caused by a gene mutation or is present at birth.
Are There Complications Of Wolff
Some people may experience low blood pressure during episodes of rapid heartbeat. A rare complication of Wolff-Parkinson-White syndrome is sudden cardiac death.
If you have any symptoms of Wolff-Parkinson-White syndrome, see your provider. Getting timely care for this condition can help avoid complications.
You May Like: What Are The Signs Of Parkinson’s
How Is Wpw Syndrome Diagnosed
People experiencing a fluttering or racing heartbeat usually tell their doctors. The same applies to those experiencing chest pain of difficulty breathing. However, if you dont have symptoms, the condition may go unnoticed for years.
If you have a racing heartbeat, your doctor will likely perform a physical exam and conduct tests that measure your heart rate over time to check for tachycardia and diagnose WPW syndrome. These heart tests may include:
Pearls And Other Issues
Patients with atrial fibrillation and rapid ventricular response are often treated with amiodarone or procainamide. Procainamide and cardioversion are accepted treatments for conversion of tachycardia associated with Wolff Parkinson White syndrome . In acute AF associated with WPW syndrome, the use of IV amiodarone may potentially lead to ventricular fibrillation in some reports and thus should be avoided.
AV node blockers should be avoided in atrial fibrillation and atrial flutter with Wolff Parkinson White syndrome . In particular, avoid adenosine, diltiazem, verapamil, and other calcium channel blockers and beta-blockers. They can exacerbate the syndrome by blocking the heart’s normal electrical pathway and facilitating antegrade conduction via the accessory pathway.
An acutely presenting wide complex tachycardia should be assumed to be ventricular tachycardia if doubt remains about the etiology.
Recommended Reading: How Close Are We To Finding A Cure For Parkinson’s
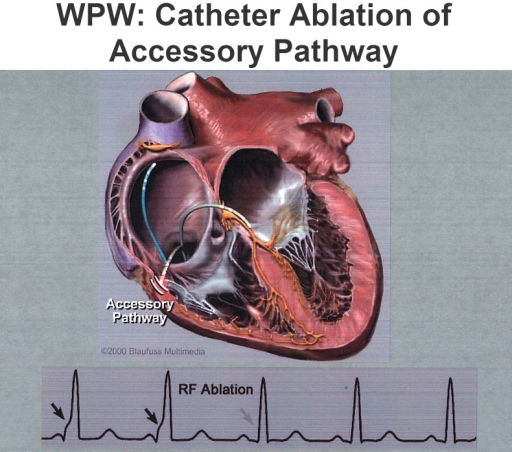
Catheter Ablation Of Accessory Pathways
Lesh, MD, Van Hare, G, Scheinman, MM. Comparison of the retrograde and transseptal methods for ablation of left free-wall accessory pathways. J Am Coll Cardiol. vol. 22. 1993. pp. 542-9.
Jackman, WM, Wang, X, Friday, KJ. Catheter ablation of accessory atrioventricular pathways by radiofrequency current. N Engl J Med. vol. 324. 1991. pp. 1605-11.
Kuck, KH, Schluter, M, Geiger, M. Radiofrequency current catheter ablation of accessory atrioventricular pathways. Lancet. vol. 337. 1991. pp. 1557-61.
Calkins, H, Langberg, J, Sousa, J. Radiofrequency catheter ablation of accessory atrioventricular connections in 250 patients: abbreviated therapeutic approach to Wolff-Parkinson-White syndrome. Circulation. vol. 85. 1992. pp. 1337-46.
Kay, GN, Pressley, JC, Packer, DL. Value of 12-lead electrocardiogram in discriminating atrioventricular nodal reciprocating tachycardia from circus movement atrioventricular utilizing a retrograde accessory pathway. Am J Cardiol. vol. 59. 1987. pp. 296-300.
Tchou, PJ, Lehmann, MJ, Donga, J. Effect of sudden rate acceleration on the human His-Purkinje system: adaptation of refractoriness in a damped oscillatory pattern. Circulation. vol. 73. 1986. pp. 920-9.
Drago, F, DeSantis, A, Grutter, G, Silverti, MS. Transvenous cryothermal catheter ablation of re-entry circuit located near the atrioventricular junction in pediatric patients. J Am Coll Cardiol. vol. 45. 2005. pp. 1096-103.
What Can I Expect If I Have Wolff
You will work with your healthcare provider to manage any symptoms of Wolff-Parkinson-White syndrome. Youll have regular appointments to make sure your symptoms are under control or havent gotten worse. Make sure to attend all your appointments and follow your providers instructions. Let your provider know right away if you experience new or worsening symptoms.
Don’t Miss: Is Finger Twitching A Sign Of Parkinson’s
Are There Any Specific Tachycardias Associated With Accessory Pathways
Cain, ME, Luke, RA, Lindsay, BD. Diagnosis and localization of accessory pathways. Pacing Clin Electrophysiol. vol. 15. 1992. pp. 801-24.
Reyes, W, Milstein, S, Dunnigan, A. Indications for modification of coexisting dual atrioventricular node pathways in patients undergoing surgical ablation of accessory atrioventricular connections. J Am Coll Cardiol. vol. 17. 1991. pp. 1561-7.
Klein, GJ, Bashore, TM, Sellers, TD. Ventricular fibrillation in the Wolff-Parkinson-White syndrome. N Engl J Med.. vol. 301. 1979. pp. 1080-5.
Dreifus, LS, Haiat, R, Watanabe, Y. Ventricular fibrillation: a possible mechanism of sudden death in patients with Wolff-Parkinson-White syndrome. Circulation. vol. 43. 1971. pp. 520-7.
Wellens, HJJ, Durrer, D. Wolff-Parkinson-White syndrome and atrial fibrillation. Am J Cardiol. vol. 34. 1974. pp. 777-82.
Campbell, RWF, Smith, R, Gallagher, JJ. Atrial fibrillation in the preexcitation syndrome. Am J Cardiol. vol. 40. 1977. pp. 514-20.
Sharma, AD, Klein, GJ, Guiraudon, GM. Atrial fibrillation in patients with Wolff-Parkinson-White syndrome: incidence after surgical ablation of the accessory pathway. Circulation. vol. 72. 1985. pp. 161-9.
Dagres, N, Clague, JR, Lottkamp, H. Impact of radiofrequency catheter ablation of accessory pathways on the frequency of atrial fibrillation during long-term follow-up: high recurrence rate of atrial fibrillation in patients older than 50 years of age. Eur Heart J. vol. 22. 2001. pp. 423-7.
What Are The Typical Electrophysiologic Findings Of Wpw Syndrome
Electrophysiology study in patients with WPW syndrome can help to confirm the presence of an AP, differentiate this condition from other forms of SVT, and to localize the pathway participating in the tachycardia for ablative therapy.
Retrograde conduction over most APs is nondecremental. Hence, in the absence of intraventricular conduction delay or the presence of multiple bypass tracts, the VA conduction time is the same over a range of pace cycle lengths. The exception to this is the slowly conducting decremental posteroseptal pathway found in the permanent form of junctional reciprocating tachycardia, in which the VA conduction time increases with increasing ventricular pacing rate.
It is important and often challenging to differentiate retrograde conduction over septal pathway from conduction over the normal AV system. One maneuver that can make this differentiation is differential pacing and measuring the VA conduction time.
Retrograde conduction over the normal AV conduction system is fastest when pacing from the apex because conduction can occur rapidly over the His-Purkinje system. VA intervals are longer when the pacing site is moved from the apex to the base. The converse is true in the presence of an AP, with VA intervals shortest when pacing from the base, closer to the site of pathway insertion than from the apex. The technique of para-Hisian pacing is useful in differentiating the septal pathway from AVNRT.
Also Check: What Are The Beginning Signs Of Parkinson’s Disease
Further Information And Support
You can get in touch with the Arrhythmia Service on extension 5298, email them on or contact them via MyGOSH once you have registered. More information about MyGOSH is at www.gosh.nhs.uk/your-hospital-visit/mygosh
There are various organisations in the UK that support people with heart problems.
The biggest is the British Heart Federation their helpline is on or you could visit their website at www.bhf.org.uk
SADS UK can also offer help and support call them on or visit their website at www.sadsuk.org.
Managing Episodes Of Supraventricular Tachycardia At Home
Its important that you are able to recognise the potential signs and symptoms of SVT and we will teach you how to do this. If appropriate, we will also teach you and your child vagal manoeuvres which can include blowing in a straw or a balloon. These work on the vagal nerve which regulates the heartbeat.
Most episodes of supraventricular tachycardia only last for a few minutes and do not need urgent treatment. Some episodes may last longer and children may be affected by these. If an episode is prolonged or the person experiences any of the red flag symptoms, they should be taken to the nearest Accident and Emergency department immediately.
The doctors will try some ‘tricks’ to try to slow the heart such as blowing into a syringe, if these are not successful or the SVT is causing other concerns such as low blood pressure, they may use a medication. As a last resort, a shock can be given as a life-saving option.
Red flags
You May Like: Severe Hip Pain Parkinson’s
How Is The Problem Treated
See supraventricular tachycardia. Patients may be treated with heart medicines to prevent episodes of SVT. In general, infants are treated until their first birthday and then the medicines can be stopped. In older children, radiofrequency ablation has become first line treatment as it is safe with high success rates.
What Causes Wpw Syndrome
When the heart beats, its muscular walls contract to force blood out and around the body. They then relax, allowing the heart to fill with blood again. This is controlled by electrical signals.
In WPW syndrome, there’s an extra electrical connection in the heart, which allows electrical signals to bypass the usual route and form a short circuit. This means the signals travel round and round in a loop, causing episodes where the heart beats very fast.
The extra electrical connection is caused by a strand of heart muscle that grows while the unborn baby is developing in the womb.
It’s not clear exactly why this happens. It just seems to occur randomly in some babies, although rare cases have been found to run in families.
Recommended Reading: Can You Die From Parkinson’s Disease
What Are The Signs And Symptoms Of Wolff
The extra electrical connection causes episodes where the heart rate suddenly quickens to an abnormally fast rate, often around 200 beats per minute. The fast heart rate can cause chest pain, breathing difficulties and heart flutters.
The symptoms of SVT occur in episodes, which can last for a few seconds to a number of hours. Children may report feeling chest flutters or palpitations, a very fast pulse, breathlessness and dizziness. In babies or children who are not able to communicate they may seem breathless, pale, irritable or unsettled, and you may be able to feel their heart racing by placing a hand on their chest.
In the majority of cases, the heart rate corrects itself to return to a normal rhythm. The frequency and length of episodes varies from person to person. Fainting or blacking out is rare and usually only occurs after a prolonged period of heart racing, lasting more than 30 minutes.
Wolff-Parkinson-White syndrome has an increased risk of heart racing later in life and a small risk of sudden death. Part of the evaluation from the Cardiology team will be to ensure that patients who maybe at increased risk are identified.
How Is Wpw Syndrome Treated
If youre diagnosed with WPW syndrome, you have several treatment options, depending on your symptoms. If youre diagnosed with WPW syndrome but dont have any symptoms, your doctor may recommend that you wait and continue follow-up appointments. If youre having symptoms, the treatment may include the following:
Recommended Reading: Are The Symptoms Of Parkinson’s Disease
Risk Factors For Developing Wpw
Risk factors for developing WPW include:
- Having a family member with pre-excitation or WPW: This is because mutations in certain genes can cause WPW.
- Congenital heart defect: Some people who are born with a specific heart defect known as “Ebstein’s anomaly” can develop WPW. This can occur if their mother was taking certain medications while she was pregnant.
Prevalence Symptoms And Prognosis Of Wpw Syndrome
An electrocardiographic pattern of preexcitation occurs in the general population at a frequency of around 1.5 per 1000. Of these, 50% to 60% of patients become symptomatic. Approximately one-third of all patients with paroxysmal supraventricular tachycardia are diagnosed as having an AP-mediated tachycardia. Patients with AP-mediated tachycardias most commonly present with the syndrome of PSVT.
Population-based studies have demonstrated a bimodal distribution of symptoms for patients with preexcitation, with a peak in early childhood followed by a second peak in young adulthood. Nearly 25% of infants who demonstrate preexcitation and/or have AP-mediated arrhythmias will lose evidence of preexcitation and/or become asymptomatic over time as the conduction property of the AP can degenerate with time.
Pappone et al reported that during a mean follow-up of 37.7 months, 18.2% and 30% of noninducible patients have lost the anterograde and retrograde conduction, respectively. The mean age of these patients was 33.6 ± 14.3. Compared to others who had persistent conductibility through the AP, these patients were asymptomatic, noninducible, and had longer minimal 1:1 conduction cycle length through the AP during the baseline EPS.
You May Like: Physical Therapy Parkinson’s Certification
What Are The Symptoms Of Wolff
Wolff-Parkinson-White syndrome symptoms vary. You might not have any symptoms at all. Or you may experience:
These tests give your healthcare provider information about your heart rate, rhythm and presence of any conduction abnormalities. Your provider can see visible heartbeat differences in a Wolff-Parkinson-White EKG versus a normal EKG.
How Is This Problem Diagnosed
Clinical features: See Supraventricular tachycardia.
Physical findings: Most of the time the physical examination is normal when the child is not having an episode. In about 15% of children, the problem is associated with a heart defect. In this case the child has physical findings associated with that defect.
Medical tests: One of the first tests usually done is an electrocardiogram. This is a safe a painless test that involves putting some stickers across the chest. The stickers are connected to a machine that records the hearts electrical activity. In WPW, the resting ECG shows pre-excitation. This finding is quite specific for WPW and helps to confirm the diagnosis. Sometimes, pre-excitation is found on a routine ECG in a person who has no symptoms.
It may be important to record an ECG at the time of symptoms. This is done by device called a transtelephonic ECG recorder. There are different models of these devices available, but they are all able to record an ECG at the time of symptoms. The tracing can then be sent over the phone to a cardiology center where it can be reviewed. Other tests that may be done include a Holter monitor, echocardiogram, and/or exercise test.
Read Also: Alternative Cure For Parkinson’s Disease
Pathophysiology Of Wolff Parkinson White Syndrome
Under normal conditions, the conduction of the electrical impulse from the atria to the ventricles of the heart follows a pathway consisting of the atrio-ventricular node and bundle of His.
The atrio-ventricular node has electrophysiological characteristics of conduction velocity and refractoriness time such as to constitute a filter capable of protecting the ventricles from the conduction of too rapid and potentially dangerous atrial impulses.
In some cases there are accessory conduction pathways between the atria and ventricles that can be located at various sites of the tricuspid and mitral valve rings.
Because of their electrophysiological characteristics, similar to the cells of the common cardiac muscle, these accessory pathways do not perform the filtering function typical of the atrioventricular node, and in certain cases can conduct impulses to the ventricles at very high frequencies.
During sinus rhythm, an accessory pathway manifests itself on the electrocardiogram as ventricular pre-excitation and the presence of a delta wave: conduction through the accessory pathway does not slow down as in the atrioventricular node, and the PQ interval on the electrocardiogram is shorter than normal .
If You Develop Any Symptoms Of Wpw
You should see your physician right away or consider going to the emergency room if you develop symptoms such as a fluttering sensation in the chest, chest pain, shortness of breath, lightheadedness, or dizziness. Your physician can order testing to see if you have WPW or another abnormal heart rhythm and can offer the appropriate treatment.
Also Check: Ashwagandha And Parkinson’s Disease
What Are The Effects Of This Problem On My Child’s Health
The information about supraventricular tachycardia applies to children with WPW. In babies, the problem resolves on its own about 50% of the time.
Rarely, WPW can cause sudden cardiac death. This can occur only if 1) the extra pathway can conduct an electrical signal very quickly from the atria to ventricles and 2) the person has an arrhythmia called atrial flutter/fibrillation. In atrial fibrillation/flutter, the upper chambers of the heart beat very fast, from 300 to 600 beats per minute. If the pathway can conduct very rapidly to the lower chambers , it could result in a life-threatening heart rhythm called ventricular fibrillation. In patients without WPW, the ventricles are protected from the fast atrial rates by the AV-node since is can only conducts a fraction of the signals . Sudden cardiac death from WPW is extremely rare in the first few years of life.
How Can We Tell The Location Of The Ap Based On The Superficial 12 Lead Ecg
Gallager, JJ, Pritchett, ELC, Sealy, WC. The preexcitation syndromes. Prog Cardiovasc Dis. vol. 20. 1978. pp. 285-327.
Ross, DL, Uther, JB. Diagnosis of concealed accessory pathways in supraventricular tachycardia. Pacing Clin Electrophysiol. vol. 7. 1984. pp. 1069-85.
Arruda, MS, McClelland, JH, Wang, X. Development and validation of an ECG algorithm for identifying accessory pathway ablation site in Wolff-Parkinson-White syndrome. J Cardiovasc Electrophysiol. vol. 9. 1998. pp. 2-12.
Fitzpatrick, AP, Gonzales, RP, Lesh, MD. New algorithm for the localization of accessory atrioventricular connections using a baseline electrocardiogram. J Am Coll Cardiol. vol. 23. 1994. pp. 107-16.
Lindsay, BD, Crossen, KJ, Cain, ME. Concordance of distinguishing electrocardiographic features during sinus rhythm with the location of accessory pathways in the Wolff-Parkinson-White syndrome. Am J Cardiol. vol. 59. 1987. pp. 1093-1102.
Cain, ME, Luke, RA, Lindsay, BD. Diagnosis and localization of accessory pathway. Pacing Clin Electrophysiol. vol. 15. 1992. pp. 801-24.
DAvila, A, Brugada, J, Skeberis, V. A fast and reliable algorithm to localize accessory pathways based on the polarity of the QRS complex on the surface ECG during sinus rhythm. Pacing Clin Electrophysiol. vol. 18. 1995. pp. 1615-27.
Xie, B, Heald, SC, Bashir, Y. Localization of accessory pathways from the 12-lead electrocardiogram using a new algorithm. Am J Cardiol. vol. 74. 1994. pp. 161-5.
Recommended Reading: Restless Legs And Parkinson’s
