Caregiving For People Living With Parkinsons
Caring for a loved one with PD can be a challenging job, especially as the disease progresses. Former caregivers of a loved one with PD suggest doing the following : Get prepared, Take care of yourself, Get help , Work to maintain a good relationship with your loved one, and Encourage the person with PD for whom you care, to stay active.
Preparing for caregiving starts with education. Reading this fact sheet is a good start. More resources are available to you in theResources section of this fact sheet. Early Parkinsonâs disease usually requires more emotional support and less hands-on care. It is a good time for family members/caregivers to educate themselves about the disease.
Related Diagnosis: Lewy Body Dementia
Current research is helping to differentiate dementia related conditions in relationship to Parkinsonâs disease. Doctorâs use a 12-month arbitrary rule to aid in diagnosis. When dementia is present before or within 1 year of Parkinsonâs motor symptoms developing, an individual is diagnosed with DLB. Those who have an existing diagnosis of Parkinsonâs for more than a year, and later develop dementia, are diagnosed with PDD.
In the simplest terms, Lewy bodies are abnormal clumps of proteins that develop in nerve cells. Cholinesterase inhibitors, medications originally developed for Alzheimerâs disease, are the standard treatment today for cognitive DLB and PDD symptoms. Early diagnosis is important, as DLB patients may respond differently than Alzheimerâs disease patients to certain drug, behavioral, and dementia care treatments.
This challenging, multi-system disorder involving movement, cognition, behavior, sleep, and autonomic function requires a comprehensive treatment approach to maximize the quality of life for both the care recipient and their caregiver. It is very important to pay attention to symptoms of dementia and to search for an expert clinician who can diagnose the condition accurately.
What Are The Symptoms Of Parkinson’s Disease
Symptoms of Parkinson’s disease differ from person to person. They also change as the disease progresses. Symptoms that one person gets in the early stages of the disease, another person may not get until lateror not at all.
Symptoms most often start between the ages of 50 and 60. They develop slowly. They often go unnoticed by family, friends, and even the person who has them.
The disease causes motor symptoms and non-motor symptoms. Motor symptoms are those that have to do with how you move. The most common one is tremor.
Tremor and other motor symptoms
Tremor, or shaking, often in a hand, arm, or leg, occurs when you’re awake and sitting or standing still . It gets better when you move that body part.
- Tremor is often the first symptom that people with Parkinson’s disease or their family members notice.
- At first the tremor may appear in just one arm or leg or only on one side of the body. The tremor also may affect the chin, lips, and tongue.
- As the disease progresses, the tremor may spread to both sides of the body. But in some cases the tremor stays on just one side.
Emotional and physical stress tends to make the tremor more noticeable. Sleep, complete relaxation, and intentional movement or action usually reduce or stop the tremor.
The most common cause of non-Parkinson’s tremor is essential tremor. It’s a treatable condition that is often wrongly diagnosed as Parkinson’s.
Besides tremor, the most common symptoms include:
Read Also: Parkinson’s Awareness Month Color
What Are The Symptoms Of Parkinsons Disease
Symptoms of Parkinsons disease and the rate of decline vary widely from person to person. The most common symptoms include:
Other symptoms include:
- Speech/vocal changes: Speech may be quick, become slurred or be soft in tone. You may hesitate before speaking. The pitch of your voice may become unchanged .
- Handwriting changes: You handwriting may become smaller and more difficult to read.
- Depression and anxiety.
- Sleeping disturbances including disrupted sleep, acting out your dreams, and restless leg syndrome.
- Pain, lack of interest , fatigue, change in weight, vision changes.
- Low blood pressure.
Signs Of Parkinsons Disease
In 1817, Dr. James Parkinson published An Essay on the Shaking Palsy describing non-motor, as well as, motor symptoms of the illness that bears his name. Parkinsons is not just a movement disorder, explained Dr. Shprecher. Constipation, impaired sense of smell, and dream enactment can occur years before motor symptoms of Parkinsons. The latter, caused by a condition called REM sleep behavior disorder, is a very strong risk factor for both Parkinsons and dementia . This has prompted us to join a consortium of centers studying REM sleep behavior disorder.
You May Like: Growth Disorder Symptoms
How Is Parkinsons Diagnosed
Doctors use your medical history and physical examination to diagnose Parkinson’s disease . No blood test, brain scan or other test can be used to make a definitive diagnosis of PD.
Researchers believe that in most people, Parkinson’s is caused by a combination of environmental and genetic factors. Certain environmental exposures, such as pesticides and head injury, are associated with an increased risk of PD. Still, most people have no clear exposure that doctors can point to as a straightforward cause. The same goes for genetics. Certain genetic mutations are linked to an increased risk of PD. But in the vast majority of people, Parkinsons is not directly related to a single genetic mutation. Learning more about the genetics of Parkinsons is one of our best chances to understand more about the disease and discover how to slow or stop its progression.
Aging is the greatest risk factor for Parkinsons, and the average age at diagnosis is 60. Still, some people get PD at 40 or younger.
Men are diagnosed with Parkinsons at a higher rate than women and whites more than other races. Researchers are studying these disparities to understand more about the disease and health care access and to improve inclusivity across care and research.
Aging is the greatest risk factor for Parkinsons, and the average age at diagnosis is 60. Still, some people get PD at 40 or younger.
The Michael J. Fox Foundation has made finding a test for Parkinsons disease one of our top priorities.
When People Talk About Parkinsons They May Mention The Effects It Has On The Substantia Nigra But Did You Know That There Are Other Areas Of The Brain That Are Affected By The Condition
Parkinsons is a condition that causes the gradual loss of the dopamine-producing brain cells of the substantia nigra an area of the brain located just above where the spinal cord meets the midbrain. It is these cells that produce and release the neurotransmitter dopamine, which has a key role in turning thought about movement into action.
While this definition of the condition is useful to briefly explain Parkinsons, the whole story is somewhat more complex. Over the last 30 years, it has become accepted that Parkinsons also causes a number of non-motor symptoms, such as changes in sleep, smell and even the way we think, which likely involve other areas of the brain.
Now scientists are looking at the broader effects of the condition on the brain in an attempt to better understand why people experience different symptoms. The finding could lead us to new treatments that tackle more than just the motor symptoms of the condition.
Also Check: Rapid Onset Parkinsonism
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinsons disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinsons disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinsons disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
How Is Parkinsons Disease Diagnosed
There are no blood tests or imaging tests used to diagnose Parkinsons disease. Diagnosis is based upon a person’s signs and symptoms, medical history, and physical and neurologic examination.
Two of the three primary symptoms must be present to make the diagnosis, with one of the symptoms being slow movement.
Other characteristics of symptoms that support the diagnosis of Parkinsons disease include:
- Symptoms began on one side of the body
- Tremors occur when the person’s limb is resting
- Symptoms can be controlled with Parkinsons disease medications
- If the diagnosis of Parkinsons disease is uncertain, a medication challenge test may be recommended
- A medication commonly used to treat Parkinsons symptoms is given for at least two months
- If the person’s symptoms improve, a diagnosis of Parkinsons disease is likely
- People with Parkinsons disease-like symptoms caused by other diseases usually do not improve with medication
Imaging tests such as magnetic resonance imaging may be used to rule out other possible diagnoses.
Dopamine transporter single-photon emission computed tomography imaging is a brain imaging test that can diagnose a condition called essential tremor that may cause similar symptoms to Parkinsons disease.
Also Check: What Are Early Warning Signs Of Parkinson’s Disease
Who Gets Parkinsons Disease
Parkinsonâs disease, documented in 1817 by physician James Parkinson, is the second most common neurodegenerative disease after Alzheimerâs disease. Estimates regarding the number of people in the United States with Parkinsonâs range from 500,000 to 1,500,000, with 50,000 to 60,000 new cases reported annually. No objective test for Parkinsonâs disease exists, so the misdiagnosis rate can be high, especially when a professional who doesnât regularly work with the disease makes the diagnosis.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
You May Like: What Are Early Warning Signs Of Parkinson’s Disease
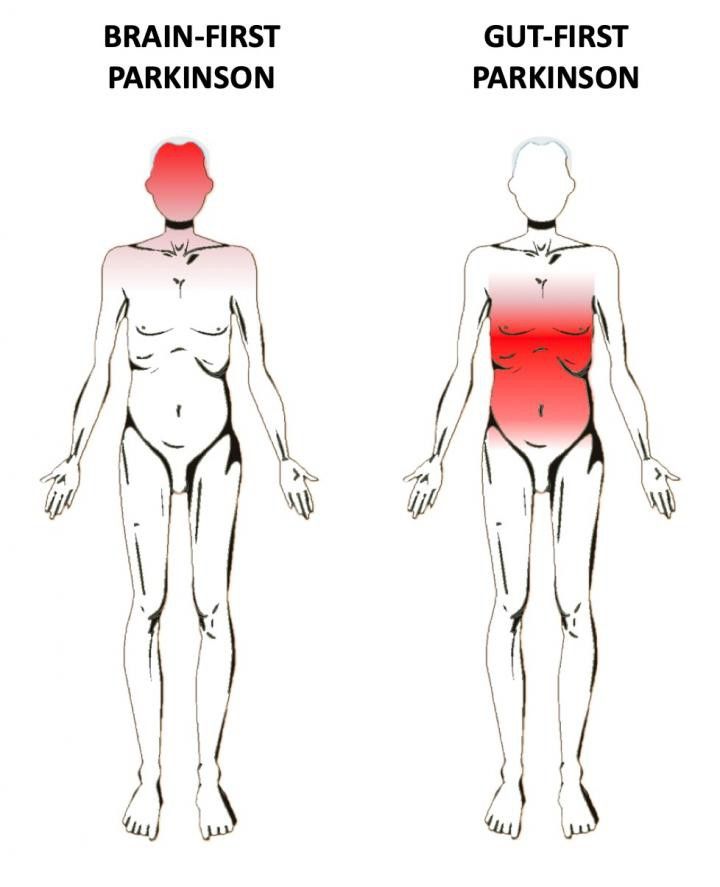
Does Parkinsons Disease Start In The Gut Or In The Brain
During most of the 20th century, Parkinsons disease was thought to be brain disorder – more specifically, a dopamine deficiency disorder leading to the characteristic motor symptoms, which defines the disease. In this millennium, however, our understanding of PD has become much more refined. We know now that many people with Parkinsons display a stereotypical distribution of brain pathology, suggesting that the initial pathology may have arisen in the nerves of the gut and nose.
Animal studies have shown that the prototypical PD pathology, i.e. assemblies of the protein alpha-synuclein, can spread from neuron to neuron. If such pathology is introduced into the gut, either by injecting it in the gut wall or by the animals directly ingesting these proteins, the pathology readily spreads to the brain and involves key structures also known to be affected in the human condition. Alpha-synuclein pathology has been found in the gut of PD patients many years before they became symptomatic. Also, nationwide registry studies have demonstrated that surgical cutting of the vagus nerve, i.e. the most important putative gut-to-brain spreading route, reduces the risk of PD by as much as 50%.
Per Borghammer, MD, PhD, DMSc presented at the 5th World Parkinson Congress in Kyoto, Japan. He is currently a senior consultant and Professor in the Department of Nuclear Medicine & PET at Aarhus University Hospital in Denmark.
What Is The Treatment For Parkinson’s Disease
There is currently no treatment to cure Parkinson’s disease. Several therapies are available to delay the onset of motor symptoms and to ameliorate motor symptoms. All of these therapies are designed to increase the amount of dopamine in the brain either by replacing dopamine, mimicking dopamine, or prolonging the effect of dopamine by inhibiting its breakdown. Studies have shown that early therapy in the non-motor stage can delay the onset of motor symptoms, thereby extending quality of life.
The most effective therapy for Parkinson’s disease is levodopa , which is converted to dopamine in the brain. However, because long-term treatment with levodopa can lead to unpleasant side effects , its use is often delayed until motor impairment is more severe. Levodopa is frequently prescribed together with carbidopa , which prevents levodopa from being broken down before it reaches the brain. Co-treatment with carbidopa allows for a lower levodopa dose, thereby reducing side effects.
In earlier stages of Parkinson’s disease, substances that mimic the action of dopamine , and substances that reduce the breakdown of dopamine inhibitors) can be very efficacious in relieving motor symptoms. Unpleasant side effects of these preparations are quite common, including swelling caused by fluid accumulation in body tissues, drowsiness, constipation, dizziness, hallucinations, and nausea.
Don’t Miss: Parkinson Disease Genes
Confusion With Essential Tremor
The tremor of Parkinsons disease is often confused with the tremor of a condition called Essential Tremor, or Benign Familial Tremor . Katherine Hepburn had Essential Tremor, and was originally misdiagnosed with Parkinsons. Ronald Reagan also had Essential Tremor. Both had a head tremor and a vocal tremor. In Essential Tremor, the hands are most commonly involved, followed by the head and then the voice. Essential Tremor can also cause the jaw to tremor, and it may be difficult to figure out if a jaw tremor is from Essential Tremor or Parkinsons. Unfortunately, some people may have both disorders. Some authorities believe that there is, in fact, an increased association between the two conditions, so that more people with Parkinsons disease have Essential Tremor than would be expected by chance alone, but this has not been established.
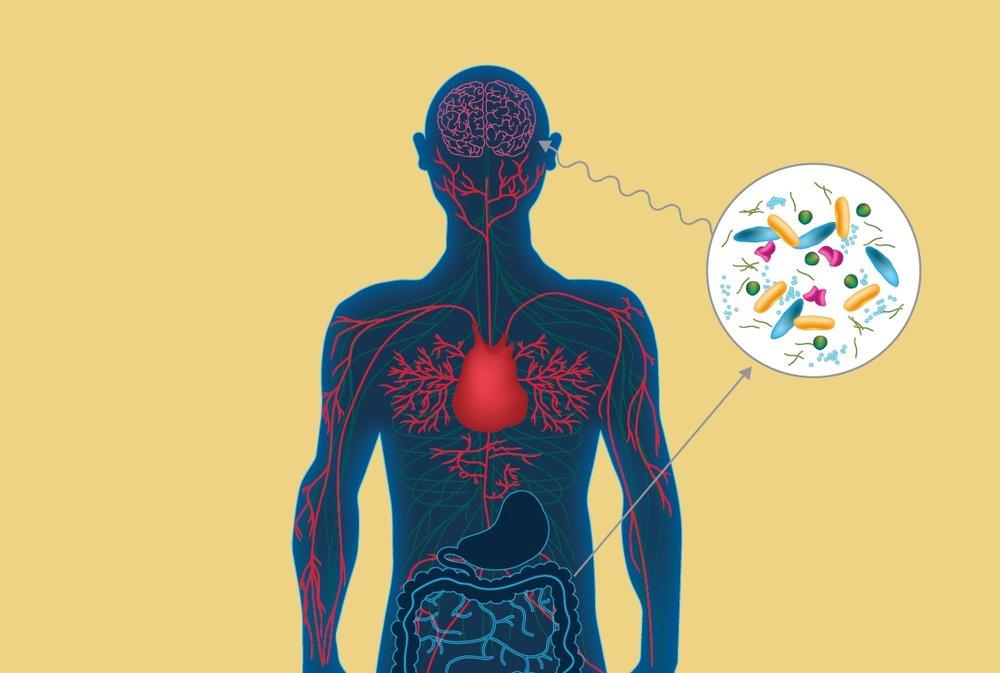
A Role For Inflammation
Yet another idea holds that that intestinal inflammation, possibly from gut microbes, could give rise to Parkinsons disease. The latest evidence supporting this idea comes from a large epidemiological study, in which Inga Peter, a genetic epidemiologist at the Icahn School of Medicine at Mount Sinai, and her colleagues scanned through two large U.S. medical databases to investigate the overlap between inflammatory bowel diseases and Parkinsons.
Their analysis compared 144,018 individuals with Crohns or ulcerative colitis and 720,090 healthy controls. It revealed that the prevalence of Parkinsons was 28 percent higher in individuals with the inflammatory bowel diseases than in those in the control group, supporting prior findings from the same researchers that the two disorders share genetic links. In addition, the research team discovered that in people who received drugs used to reduce inflammationtumor necrosis factor inhibitorsthe incidence of the neurodegenerative disease dropped 78 percent.
This study further validates the theory that gut inflammation could drive Parkinsons pathogenesis, says Madelyn Houser, a graduate student in neuroscientist Malú Tanseys lab at Emory University. The anti-TNF finding in particular, she adds, suggests that the overlap between the two diseases might be primarily mediated by inflammation.
Read Also: Parkinson\’s Stage 5 Life Expectancy
Symptoms Of Parkinson’s Disease
You can attribute the symptoms of Parkinson’s to a deficiency of a chemical in your brain called dopamine. The four classic motor symptoms of Parkinson’s include:
Shaking and tremors while you are resting is typically the first sign of Parkinson’s disease, but about one-third of patients won’t experience those symptoms. These symptoms tend to be worsened by emotional and physical stress. Sleep or moving can help reduce these issues.
Parkinson’s disease is both chronic and progressive with symptoms generally getting worse as time goes on. As it progresses, other disabilities can develop, including:
- Difficulty talking and swallowing
- A sudden inability to move,
Some sufferers also have symptoms that don’t affect their motor skills, including:
- Mental health issues such as anxiety, depression and memory loss
- Loss of smell
- Trouble sleeping, including thrashing and other sudden movements
- Change in blood pressure
What Are The Causes
The cause of Parkinson’s is largely unknown. Scientists are currently investigating the role that genetics, environmental factors, and the natural process of aging have on cell death and PD.
There are also secondary forms of PD that are caused by medications such as haloperidol , reserpine , and metoclopramide .
Recommended Reading: What Color Represents Parkinson’s Disease
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinsons disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinsons.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinsons disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinsons disease has a tremor, nor is a tremor proof of Parkinsons. If you suspect Parkinsons, see a neurologist or movement disorders specialist.
Tremors
Rigidity
Bradykinesia
Postural Instability
Walking or Gait Difficulties
Dystonia
Vocal Symptoms
