How Fast Does Parkinson’s Disease Progress
People tend to move through the Parkinson’s disease stages slowly, usually over the course of years. Research has shown that the disease tends to progress less rapidly in people who are diagnosed at a younger age than those diagnosed later in life.
What’s more, Parkinson’s disease may begin decades before a patient even notices a single motor symptom.
“We know that Parkinson’s disease actually starts many, many years before you see that tremor or that shuffling,”Lynda Nwabuobi, MD, assistant professor of clinical neurology at Weill Cornell Parkinson’s Disease and Movement Disorders Institute, tells Health. “We think at least 30 years.”
Parkinson’s Disease Diet And Nutrition
Maintaining Your Weight With Parkinson’s Disease
Malnutrition and weight maintenance is often an issue for people with Parkinson’s disease. Here are some tips to help you maintain a healthy weight.
- Weigh yourself once or twice a week, unless your doctor recommends weighing yourself often. If you are taking diuretics or steroids, such as prednisone, you should weigh yourself daily.
- If you have an unexplained weight gain or loss , contact your doctor. He or she may want to modify your food or fluid intake to help manage your condition.
- Avoid low-fat or low-calorie products. . Use whole milk, whole milk cheese, and yogurt.
Parkinson’s Disease And Palliative Care
This page outlines the decline of Parkinson’s disease and helps those coping with Parkinson’s understand what a palliative care team provides. There is a brief discussion of when and how to get palliative care, an online quiz to determine if palliative care is right for your family and a link to a palliative care provider search tool.
You May Like: Average Life Expectancy With Parkinson’s
What Are The Risks Of Not Receiving Any Dopaminergic Medication
There is the possibility of neuroleptic malignant-like syndrome , a life-threatening and distressing condition resulting in rigidity and fever, from withdrawal of therapy.31 This can also occur with sudden cessation of Deep Brain Stimulation .32,33,34 To reduce the risk of this, dopaminergic therapy at the end of life should be continued.27 It should also be noted that in a patient dying of another condition, whose PD is still responsive to dopaminergic medication, the cessation of this also risks aspiration pneumonia.35 Transdermal rotigotine can be used in patients in whom a NG tube may cause excessive distress or is not possible. The dose should be calculated with an accepted converter.36
My Parkinson’s Story: Advanced Parkinsons
This 10-minute video alternates between an interview with a man and his wife and his palliative care team, including a doctor, nurse, clerg and social worker. The man and his wife shares his experience with late stage Parkinson’s. The palliative care team explains that their job is to support the best physical, emotional and spiritual wellbeing of the immediate family as well as help the family make end of life decisions.
Also Check: Can Parkinson’s Run In The Family
What To Do With Deep Brain Stimulation At The End Of Life
Deep brain stimulation uses an Implantable Pulse Generator, usually placed in the infraclavicular area, connected to leads within the brain. There is a remote programmer, and also a charging unit in the case of a rechargeable device, which are given to the patient and their carer. It improves dyskinesias and also has a levodopa sparing effect.37
Deactivation of DBS may lead to increased symptom burden as mentioned in the section above and so awareness of features of PHS should be considered if there is failure at the end of life. Supportive treatment should be given if possible,38 and anticipation of symptoms of distress from rigidity and fever.
After death, deactivation of the device with the patients handheld programmer is required before removing the pulse generator and battery in the case of a cremation.
The 5 Stages Of Parkinsons Disease
Getting older is underrated by most. Its a joyful experience to sit back, relax and watch the people in your life grow up, have kids of their own and flourish. Age can be a beautiful thing, even as our bodies begin to slow down. We spoke with David Shprecher, DO, movement disorders director at Banner Sun Health Research Institute about a well-known illness which afflicts as many as 2% of people older than 65, Parkinsons Disease.
You May Like: End Stages Parkinsons
How Can I Stop Being Numb While Sleeping
Sleep with your arms at your sides instead of above your head. Sleeping with your arms above your head can cause numbness by cutting off circulation to your hands. Avoid folding your arms under your pillow while you sleep. The weight of your head can put pressure on your wrists or elbows and compress a nerve.
Managing Care In Late Stages
, March 3, 2017
What to expect in the late stages of Parkinson’s disease and the challenges of caring with those difficulties and needs. Tips for helping someone overcome freezing, accomplishing activities of daily living as long as possible, managing medications and swallowing issues, and ways to minimize caregiver stress.
Recommended Reading: Life Expectancy For Parkinson’s
Care Of Patients With Advanced Parkinsons Disease
Presenting at the UCSF 9th Annual Conference of Parkinsons Disease for Patients and Caregivers, Dr. Maya Katz spoke for 38-minutes about caring for those with advanced Parkinsons disease, including a definition of advanced PD, medication considerations, non-motor symptoms, wellness and exercise, goals of care and taking a supportive care approach.
How Can Parkinson’s Affect Someone At The Advanced Or Palliative Stage
Parkinsons progresses in stages: diagnosis, maintenance, advanced and palliative. Professionals should have talk to people with Parkinsons about advance care planning in the earlier stages of the disease. This can allow them to express their wishes and preferences for their care in the later stages of the disease and make plans for the future.
Although the condition progresses differently and at a different speed for each person, the advanced stage can potentially cover a long period of time.
Problems that affect someone with advanced Parkinsons may include:
- medicines being less effective at managing symptoms than before
- having to take lots of medicines to manage symptoms and side effects
- more off periods when the effects of medication are reduced, and people experience movement fluctuations and involuntary movements
- increased mobility problems and falls
- swallowing difficulties
- less control of their Parkinsons symptoms, which become less predictable
- pain.
Some of the more advanced symptoms can lead to increased disability and poor health, which can make someone more vulnerable to infection, such as pneumonia. People with Parkinsons most often die because of an infection or another condition, usually caused by Parkinsons.
Also Check: What Causes Dyskinesia In Parkinson’s
What You Can Do
As of 2021, there is no definite cure for Parkinsons disease. There is also no definite known cause. Its likely due to a combination of an individuals susceptibility and environmental factors. Most cases of Parkinsons disease happen without a genetic link.
According to research published in 2012, only report having a family member with the disease. Many toxins are suspected and have been studied, but no single substance can be reliably linked to Parkinsons.
However, research is ongoing. Its estimated that
What Is The Prognosis For Someone With Early
One of the challenges of early-onset Parkinsons disease is that you will inevitably live longer with the condition, as Parkinsons alone is not fatal. Early-onset Parkinsons disease does not always present the same way as late-onset Parkinsons disease, and there is no definite prognosis. Younger Parkinsons patients may be more at risk of developing non-motor symptoms, such as depression, sleep disorders, anxiety and urinary issues, which can cause health complications as the disease progresses.
However, early-onset patients also show slower disease progression, and it can take years to move between stages. Each case of Parkinsons is reviewed on an individual basis, so only your doctor can tell you your prognosis.
You May Like: Katharine Hepburn Parkinsons
What Are The Considerations For Pain Management In The Last Days Of Life In Pd
It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25 The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
How Do I Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinsons disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinsons disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinsons disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinsons disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinsons disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
What Are The Final Stages Of Parkinsons Disease
Quality of life declines rapidly in the final stages of Parkinsons disease. In addition to advanced motor symptoms, you may also begin experiencing greater speaking and memory issues, such as Parkinsons disease dementia. Incontinence issues become more common, and frequent infections may require hospital care.
You May Like: Can Parkinson’s Change Your Personality
Living With Parkinsons Disease
Depending on severity, life can look very different for a person coping with Parkinsons Disease. As a loved one, your top priority will be their comfort, peace of mind and safety. Dr. Shprecher offered some advice, regardless of the diseases progression. Besides movement issues Parkinsons Disease can cause a wide variety of symptoms including drooling, constipation, low blood pressure when standing up, voice problems, depression, anxiety, sleep problems, hallucinations and dementia. Therefore, regular visits with a neurologist experienced with Parkinsons are important to make sure the diagnosis is on target, and the symptoms are monitored and addressed. Because changes in your other medications can affect your Parkinsons symptoms, you should remind each member of your healthcare team to send a copy of your clinic note after every appointment.
Dr. Shprecher also added that maintaining a healthy diet and getting regular exercise can help improve quality of life. Physical and speech therapists are welcome additions to any caregiving team.
Parkinsons Disease Late Stages: What Will Happen To Me
With advanced Parkinsons disease, stage 5 life expectancy can be months or years depending on how your condition presents. You are likely to need round-the-clock care at this stage, and you may not be able to move around independently. Patients with late-stage Parkinsons disease are more susceptible to pneumonia, sepsis, pyelonephritis and decubitus ulcers. Late-stage Parkinsons also leads to Parkinsons disease dementia in 50% of cases. For all of these reasons, many late-stage Parkinsons patients are cared for by loved ones or in a hospice.
Also Check: How To Donate To Parkinson’s Research
Parkinsons Disease Is A Progressive Disorder
Parkinsons Disease is a slowly progressive neurodegenerative disorder that primarily affects movement and, in some cases, cognition. Individuals with PD may have a slightly shorter life span compared to healthy individuals of the same age group. According to the Michael J. Fox Foundation for Parkinsons Research, patients usually begin developing Parkinsons symptoms around age 60. Many people with PD live between 10 and 20 years after being diagnosed. However, a patients age and general health status factor into the accuracy of this estimate.
While there is no cure for Parkinsons disease, many patients are only mildly affected and need no treatment for several years after their initial diagnosis. However, PD is both chronic, meaning it persists over a long period of time, and progressive, meaning its symptoms grow worse over time. This progression occurs more quickly in some people than in others.
Pharmaceutical and surgical interventions can help manage some of the symptoms, like bradykinesia , rigidity or tremor , but not much can be done to slow the overall progression of the disease. Over time, shaking, which affects most PD patients, may begin to interfere with daily activities and ones quality of life.
How To Manage Symptoms At The End Of Life
At the end of life, good practice is to plan for any potential symptoms that may arise. The most common symptoms anticipated are pain, dyspnoea, nausea and vomiting, agitation, anxiety, delirium and noisy respiratory secretions.18 For patients with PD particular considerations should be given to the more commonly used medicines, specifically anticholinergics and antidopaminergics. These are usually prescribed for treatment of respiratory secretions and nausea and vomiting. Alternatives are available for respiratory secretions, and include glycopyrronium, in preference to hyoscine hydrobromide. Although this is an anticholinergic, only a small proportion crosses the blood brain barrier.
For nausea and vomiting, ondansetron,19 cyclizine, domperidone have all been suggested in PD.20 However, ondansetron has been shown to be inferior to domperidone in the pre-treatment of apomorphine.21 Cyclizine has anticholinergic properties and may exacerbate confusion, especially when comorbid psychosis or cognitive impairment are present. Levomepromazine, although it has antidopaminergic effects, has been shown to be effective for nausea with rotigotine in a case report.22
Agitation, dyspnoea and pain can all be managed with the same anticipatory medications as recommended.20 Specifically relating to PD, several case reports have supported the intraoperative use of midazolam, during sedation, for tremor and dyskinesias,23,24 as well as for agitation at the end of life.20
Don’t Miss: Adderall And Parkinson’s
What Not To Eat If You Have Parkinsons
Dont eat too many sugary foods and drinks as these can negatively impact your immune system. Opt for naturally sweetened food and reduce your sugar intake to manage Parkinsons symptoms. Dont eat too much protein. Consuming lots of beef, fish, or cheese may affect the effectiveness of certain Parkinsons medications.
What Is Parkinsons Disease
Parkinsons is a neurological illness caused by degeneration or breaking down of cells in the nervous system, explained Dr. Shprecher. The nature of Parkinsons Disease is progressive, meaning that it gets worse over time. To comprehend the natural progression of the disease, we should understand its five stages, as explained by the Parkinsons Foundation.
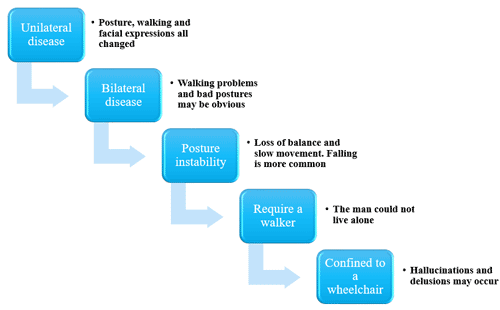
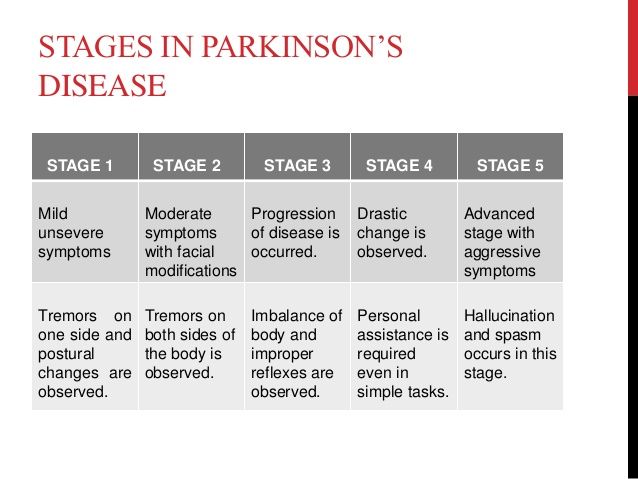
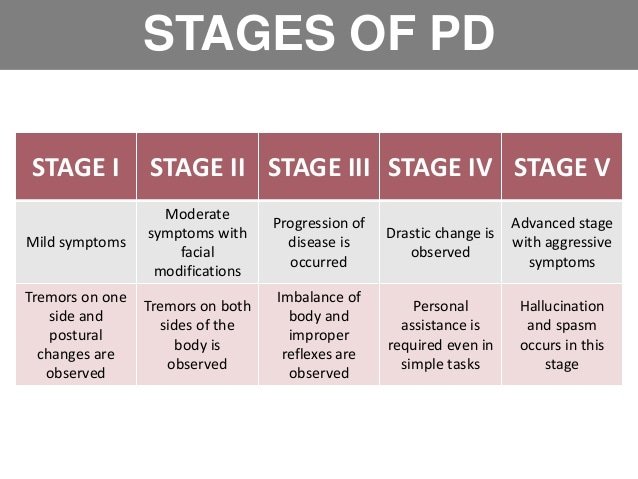
Stage One
Individuals experience mild symptoms that generally do not interfere with daily activities. Tremor and other movement symptoms occur on one side of the body only. They may also experience changes in posture, walking and facial expressions.
Stage Two
Symptoms worsen, including tremor, rigidity and other movement symptoms on both sides of the body. The person is still able to live alone, but daily tasks are more difficult and lengthier.
Stage Three
This is considered mid-stage. Individuals experience loss of balance and slowness of movements. While still fully independent, these symptoms significantly impair activities such as dressing and eating. Falls are also more common by stage three.
Stage Four
Symptoms are severe and limiting. Individuals may stand without help, but movement likely requires a walker. People in stage four require help with daily activities and are unable to live alone.
Stage Five
Recommended Reading: Effects Of Sugar On Parkinson’s Disease
Nutrition Hydration And Genitourinary Care
Malnutrition is a common problem in advanced PD patients. It is caused by difficulty feeding, altered satiety mechanism, diminished gastric and intestinal motility, inactivity, lack of appetite, dysphagia, and metabolic syndrome. In patients still able to eat independently, meal and portion sizes should be monitored in order to provide sufficient nutrition. Any effort, including compensatory strategies, should be considered to delay the PEG placement. Adequate hydration is another concern for late-stage PD patients, since even mild temperature change can lead to relative dehydration and exacerbate confusion and OH and cause syncope. Many patients become embarrassed when eating or drinking, and nursing assistance, can assure adequate nutrition and hydration through a nonjudgmental caregiver that assist patients with the administration of meals.
