Daytime Tips For Better Sleep
- Wake up at the same time every day, using an alarm if you have to.
- Get out of bed right after you wake up. Too much time spent in bed can lead to more waking at night.
- Eat regular, healthy meals, and eat at the same time every day. Three to four small meals are better than 1-2 large meals.
- Limit daytime napping to a 40-minute NASA nap . Too many or too-long naps can make sleep at night more difficult.
- Do not drink coffee, tea, sodas, or cocoa after noon. They contain caffeine and can interfere with normal sleep.
- Do not drink alcohol after dinner. It may help you fall asleep faster, but makes sleep shallower later in the night. Alcohol can also make snoring and sleep apnea worse.
- Use caution when taking headache and cold medicines. Some contain stimulants that can affect sleep.
- Stop smoking. Cigarette smoking stimulates the body and makes sleep difficult.
- Increase or start doing daily exercise. Regular exercise helps to deepen sleep. Avoid heavy exercise 2 hours before bedtime.
Causes Not Related To Parkinsons
There are a number of other causes of sleep problems that are not related to Parkinsons, such as pain not connected to Parkinsons or sleep apnea. People with sleep apnea experience frequent interruptions in their breathing as they sleep, which can further fragment sleep and cause low levels of oxygen in the blood.
Finally, simply failing to prepare the bedroom for rest by minimizing outside light and activities as well as reducing noise can have a major impact on sleep quality. Exercising too late in the afternoon or evening can sometimes make it difficult to fall asleep. Similarly, drinking too many liquids, especially alcohol or caffeine, can interfere with sleep at night.
Highlights From The Episode
In case you missed it, the August broadcast of Dr. Gilbert Hosts was a very informative conversation, and we encourage you to watch the full episode. For your convenience, weve listed the topics and questions from the episode below with timestamps, so you can skip to what may interest you most:
00:48 Introduction of Dr. Ospina
01:27 Dr. Ospinas presentation about sleep issues
23:37 My husband sleeps fairly well at night but sleeps a lot during the day. How do we get him to not sleep so much during the day?
25:19 My father has had much improvement in his sleep by taking CBD. What is your opinion on this?
27:20 Discussion of OFF time
31:23 Will Prozac affect my sleep? Is it better to take it in the morning or at lunch rather than at night?
32:48 Does deep brain stimulation help insomnia and sleep issues?
35:13 I wake up frequently with leg and foot cramps/dystonia. How should I treat this?
36:51 Is it OK to take Nyquil for insomnia? Melatonin? If so, how much melatonin should I take?
38:05 Could numbness in the feet be associated with restless leg syndrome?
39:36 Can you get accustomed to sleep medications whereby the medication is no longer effective?
40:40 What should I do if Im wide awake in the middle of the night? Should I try to be active and get something done, or should I try to stay in bed?
Don’t Miss: What Can You Do To Prevent Parkinson’s Disease
Sleep Matters: A Review Of Sleep Issues In Parkinson’s
Sleep disorders are present in 66-99% of people with Parkinson’s disease . In this 1-hour webinar Okeanis Vaou, MD, describes common sleep disorders in PD and how to treat them. Disorders described include REM sleep behavior disorder, daytime sleepiness, insomnia, nocturnal motor fluctuations, and restless leg syndrome. Dr. Vaou ends the webinar with tips on how to maintain good sleep hygiene.
Sleep And Parkinsons Disease
The Palo Alto Parkinsons Disease support group February 2020 meeting featured Dr. Emmanuel During, a Stanford sleep medicine neurologist. During the meeting, Dr. During discusses sleep disturbances that can occur in PD, such as insomnia, restles legs syndrome, sleep apnea, and REM sleep behavior disorder , along with available treatments. There’s a question and answer session.
Don’t Miss: Can Parkinson’s Be Reversed With Diet
How Is Sleep Apnea Treated
A continuous positive airway pressure machine, a machine that blows air into your airway at a pressure that is sufficient to keep the airway open during sleep, is the most consistently effective treatment for obstructive sleep apnea. The CPAP machine is connected by a tube to a face mask worn when sleeping through the night. It controls pressure in ones throat to prevent the walls of the throat from collapsing, creating better sleep quality. CPAP should be worn for the entire night and for naps.
Sleep Tips From Survey Respondents
- Exercise helps me go to sleep, say more than an hour of brisk walking or an hour at the gym.
- Bedtime routine I find a bedtime routine helps most with getting to sleep. I dont go to bed too early, and must read for a while before trying to settle down.
- Specialised beds and bedding I have a silky sheet underneath me which helps me to turn over. I also have some bars which stop me falling out of bed.
You might be interested in reading more information and advice on sleep and early morning off on the following page of the Parkinsons UK website parkinsons.org.uk/information-and-support/sleep-and-parkinsons
You May Like: Does Parkinson’s Disease Hurt
Strategies That Improve Wakefulness During The Day
Non-pharmacologic interventions for EDS
- Encourage daily exercise and activities a person without an activity planned is much more likely to doze than one who is engaged in an activity. Be realistic about scheduling a person with advanced PD, but aim for at least one scheduled activity a day
- Light therapy Light therapy, in which a person is exposed to bright light via a light box, is used as a treatment modality for sleep disorders and psychiatric disorders not associated with PD. A small clinical trial testing its efficacy in PD was conducted and demonstrated an improvement in sleep and in excessive daytime sleepiness.
Pharmacologic interventions for EDS
There are no FDA approved medications for EDS in the context of PD. However, clinicians sometimes prescribe medication off-label for EDS. These include modafinil, methylphenidate, and caffeine. Istradefylline is a medication approved to treat motor symptoms of PD. A small trial demonstrated its potential improvement of EDS as well. Talk with your physician about the possibility of using a medication to maintain wakefulness during the day.
Recommended Reading: What Other Diseases Mimic Parkinsons
Rem Sleep Behavior Disorder
REM stands for rapid eye movement. This is the stage of sleep when dreams take place. People with REM sleep behavior disorder act out their dreams, which can be violent. RBD is one of the early warning signs of Parkinsons. Healthy people with RBD have a higher risk of developing Parkinsons. RBD can be treated with the drug clonazepam .
Also Check: How Do Doctors Test For Parkinson’s
Melatonin On Excessive Daytime Sleepiness
Excessive daytime sleepiness is one of the most common non-motor symptoms of PD. It has been reported that most PD patients suffer from excessive daytime sleepiness , which seriously impairs the quality of life of patients with PD . Because of sleep disorders, especially sudden sleep attacks, many activities are dangerous for patients with PD, such as driving a car or operating a machine.
Tips For Better Sleep
- Keep a regular sleep schedule go to bed at the same time and get up at the same time.
- Choose your bedtime based on when you want to get up. Plan to spend seven to eight hours a night in bed.
- Make a bedtime routine for example, snack, bath, tooth-brushing, toileting and follow it every evening.
- Spend time outdoors and exercise every day, in the morning if possible. Avoid exercise after 8:00 p.m.
- If you cant get outdoors, consider light therapy sitting or working near a light therapy box, available at drug stores and department stores.
- If you nap, try to do so at the same time every day, for no more than an hour, and not after 3:00 p.m.
- Sleep in a cool dark place and use the bed only for sleeping and sexual activity.
- Do not read or watch television in bed.
- Use satin sheets and pajamas to make moving in bed easier.
- Minimize drinking liquids for three hours before bedtime to avoid frequent nighttime urination.
- Go to the bathroom immediately before retiring.
- Place a commode next to the bed, to minimize the effort, and light to get up during the night.
Also Check: Occupational Therapy Intervention For Parkinson’s Disease
What Types Of Sleep Problems Do People With Parkinsons Disease Have
Parkinsons disease affects every person differently. It also impacts sleep in different ways. People with Parkinsons may have:
- Insomnia, finding it hard to fall asleep.
- Fragmented sleep, waking up many times over the night.
- Excessive daytime sleepiness, finding it hard to stay awake during the day.
- Very vivid dreams, which may cause hallucinations or confusion after waking up.
- Emotional dreams or nightmares, which may make you feel emotionally drained after waking up.
Hallucinations And Rem Sleep Disorders In Parkinsons Disease
At timestamp 1:58 in this recording of Thrive: HAPS 2020 Caregiver Conference, you will find a one hour talk by neurologist Joohi Jimenez-Shahed, MD. In it she delves into what REM sleep behavior disorder is and is not, and the distinctions between hallucinations, delusions, and delirium. Managment options for RBD and hallucinations are included.
Read Also: Parkinson’s Medical Alert Bracelet
Falling Asleep During The Day
Not getting enough restful sleep at night, some medications, and possibly the disease itself leading to neurodegeneration can lead to daytime sleepiness and even sleep attacks in people with Parkinsons disease.
Excessive daytime sleepiness is one of the most frequent sleep disorder symptoms in Parkinsons disease and can affect a patients quality of life.
Trying to get more restful sleep at night and adjusting medications can help with excessive daytime sleepiness.
A new therapy from Theranexus is also currently being investigated in a Phase 2 clinical trial to help with excessive daytime sleepiness.
Parkinsons News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Study Design And Participants
We performed a multicenter, observational, outpatient-based, cross-sectional study entitled, Nocturnal symptoms and quality of life in patients with Parkinsons disease in Shanghai . From June to November of 2019, the study recruited 1006 PD patients from the clinics of 40 hospitals in Shanghai. Patients had been diagnosed with PD according to the Movement Disorder Society PD Criteria. Patients with secondary Parkinsonism, stroke, brain tumor, or an alternative cause for parkinsonism symptoms were excluded. Written informed consent was obtained from all participants, and the study was performed with the approval of the Ethics Committee of Xinhua Hospital affiliated to the Shanghai Jiao Tong University School of Medicine and the Research Ethics Committee of each site in the SHAPD study group.
You May Like: Parkinson’s Disease And Hallucinations
Inclusion And Exclusion Criteria
The inclusion criteria were as follows: Study type: randomized controlled trials Participants: patients who were clinically diagnosed with PD Interventions: the experimental group was given melatonin or prolonged-release melatonin Control: the control group was given placebo or clonazepam and Outcome: at least one of the following 4 instruments was employed: Pittsburgh Sleep Quality Index , Epworth Sleepiness Scale , RBD questionnaire and polysomnography sleep parameters.
Exclusion criteria were: Non-randomized controlled trial Repeated publication and Studies whose outcomes did not meet our meta-analysis requirements.
Symptoms And Diagnostic Considerations
Rapid Eye Movement Sleep Behavior Disorder is a non-familial sleep disorder, characterized by the loss of the inherent muscle atonia observed during normal REM sleep. This phenomenon is often referred to as REM Sleep without Atonia . Whilst isolated RSWA is frequently an incidental finding in sleep studies, it forms the substrate of the dream enactment behavior which defines RBD. Here, individuals experience vivid dreams which they act out during sleep.
It is important to remember that dream enactment and limb movements during sleep can occur in the healthy population, often in the context of heightened emotional states . The same symptoms may also be experienced during withdrawal from sedatives or alcohol. In non-pathological dream enactment, individuals typically respond to dream content during the transition from REM sleep to the awake state and while maintaining REM atonia during much of the REM period. In contrast, RBD individuals will maintain REM sleep during and immediately after most of their dream enactments. As acute dream enactment is generally self-limiting, the chronicity of symptoms is a key distinguishing factor, and forms part of the diagnostic criteria for RBD .
Recommended Reading: Does Parkinson’s Cause Body Odor
Potential Therapy For Problems With Cognition Due To Parkinsons Disease
Notably, the trial involved a significant proportion of Parkinsons patients with REM sleep behavior disorder , a nonmotor Parkinsons symptom that has been associated with more severe cognitive burden.
The cognitive findings seen in the majority of patients with bode well for our plans to launch a larger and longer Phase 2b study in 2023 in this population, Ford said.
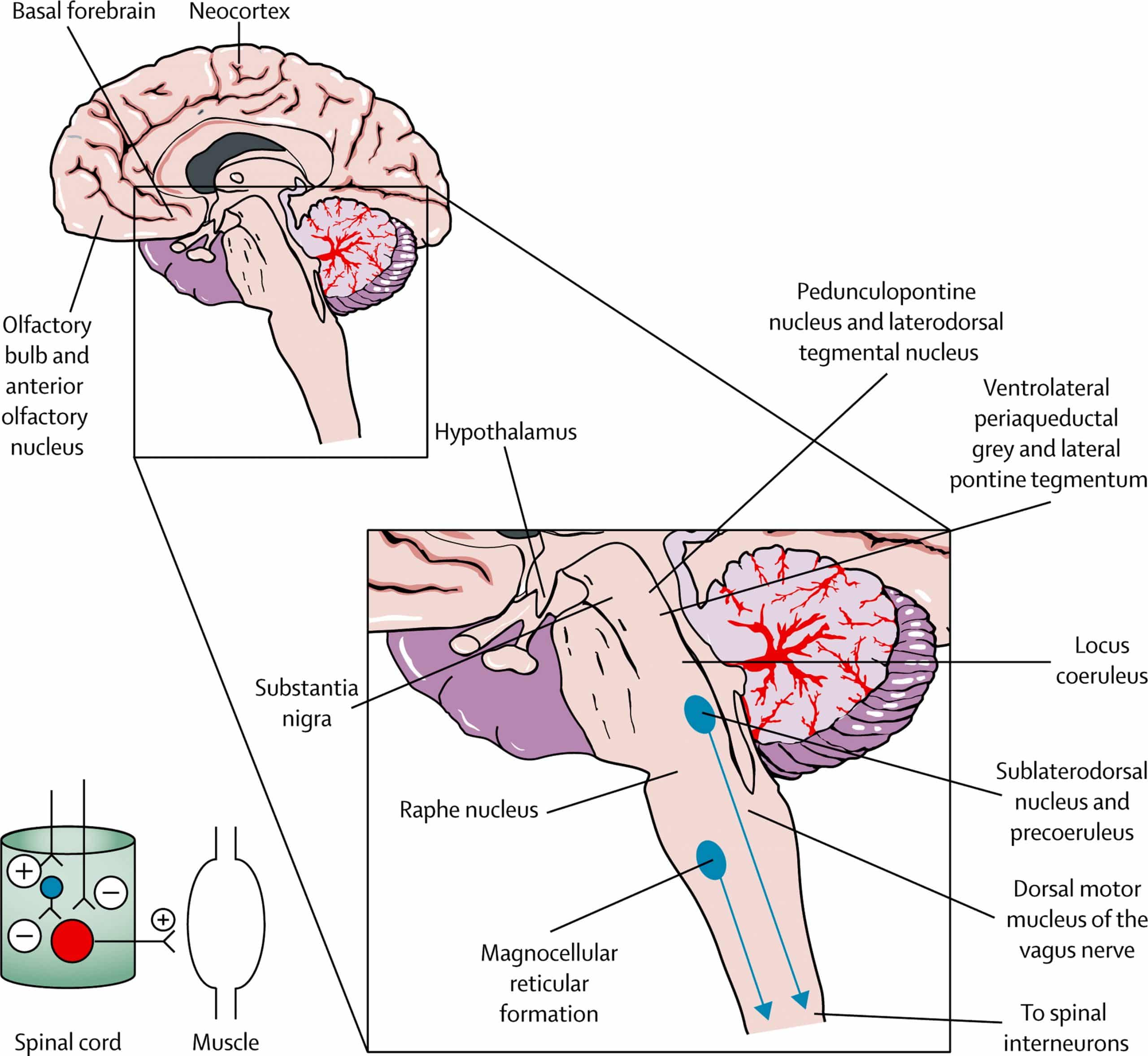
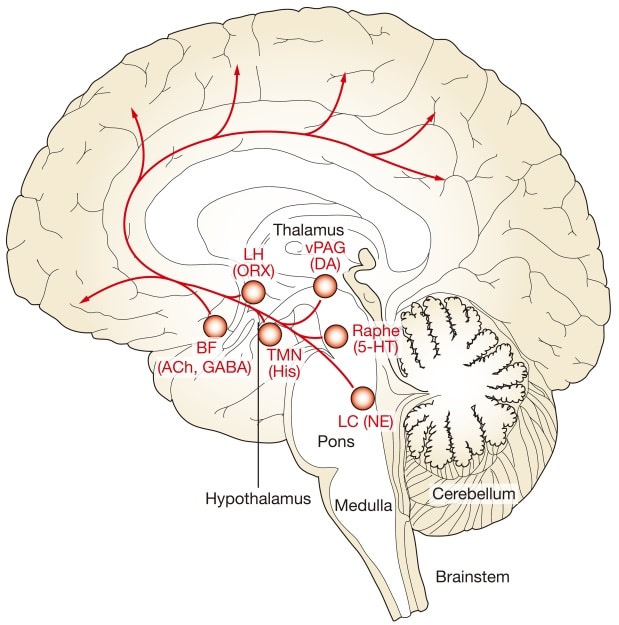
People with neurodegenerative diseases such as Parkinsons and Alzheimers disease experience early dysfunction in a brain region called the locus coeruleus, which may emerge years before disease symptoms appear.
The locus coeruleus is the key site for production of norepinephrine, a brain signaling molecule involved in processes like attention, learning, memory, and sleep. As such, patients with problems in this brain region experience a range of symptoms, including cognitive impairment.
CST-103 is an agonist, or activator, of B2-ARs, the receptors to which norepinephrine binds to exert its effects, that can enter the brain and spinal cord. Essentially, the oral treatment aims to mimic norepinephrines actions in the brain to easing cognitive symptoms.
However, activating these receptors in the rest of the body can lead to serious cardiometabolic side effects with long-term use.
The treatment was generally safe, without reports of the known side effects of B2-ARs agonists.
A Cheaper Quicker Form Of Assessment
Unlike the usual method of assessing the risk of Parkinsons disease, which is called dopamine transporter imaging, the current assessment is inexpensive and easy to apply.
Dopamine transporter imaging, explain Dr. Postuma and colleagues, assesses the integrity of the dopaminergic system, which typically becomes compromised in parkinsonism and Parkinsons disease. However, this test is complex and costly. In contrast, assessing for the risk factors that the current study considers is both quick and cost efficient.
We confirmed a very high risk of in people with REM sleep disorder and found several strong predictors of this progression, notes Dr. Postuma.
As new disease-modifying treatments are being developed for and related diseases, these patients are ideal candidates for neuroprotective trials.
Dr. Ron Postuma
You May Like: Home For Parkinson’s Patients
Detecting Parkinsons Disease Through Sleep
Researchers in the United States have discovered a way to use artificial intelligence to evaluate Parkinsons disease , a neurological disease that affects more than 10 million people worldwide.
PD is a progressive disorder that does not have a specific diagnostic test. PD is typically diagnosed based on patient reports of symptoms like tremors in the hand muscles or stiff arms or legs. However, these symptoms usually do not show up until several years after the disease has started, leading to late diagnosis and missed opportunities for early treatment.
There is a link between PD and breathing, though, and sleep breathing disorders often present years before PD symptoms. In the study, researchers used an AI-based system to look for abnormal nighttime breathing patterns in a set of data with over 7,500 people and nearly 12,000 nights. The breathing signals were collected using either a wearable device or nearable device .
Researchers found that for patients using the wearable device for one night, the AI system was about 80% accurate in identifying PD. For patients who used the nearable device for several nights, the accuracy was even higher.
The researchers from the study are hoping the AI-based system can lead to earlier diagnosis and treatment of PD. Using wearable or nearable technology could also be easier and less expensive for patients, both in diagnosing the disease and tracking its progression.
References
Somnolence And Excessive Daytime Sleepiness
Somnolence and EDS occur commonly in PD. Etiologies of somnolence in PD include reversal of the sleepwake cycle, the disease process itself, disrupted sleep due to a variety of motor and nonmotor causes, and the use of dopamine agonists and other antiparkinsonian medications. Several studies have found that dopamine agonists are more likely to cause somnolence than levodopa. The soporific effects of the commonly used dopamine agonists appear to be similar as assessed by Epworth Sleepiness Scale scores.36
EDS occurs in PD patients, and is usually associated with dopamine agonist use. EDS may occur with use of other PD medications, including levodopa/carbidopa. However, EDS as measured by the ESS does not always correspond to shortened sleep latency as quantified by the Multiple Sleep Latency Test .10 In addition, nocturnal sleep disturbance as measured by polysomnogram may not account for the severity of daytime sleepiness in PD patients with EDS.10
Recommended Reading: Reishi Mushroom Parkinsons Disease
Also Check: What Is The Best Food For Parkinson Disease
Insomnia And Nonmotor Symptoms Of Pd
Depression and anxiety affect between 30 and 60% of PD patients and appear to result from neurotransmitter changes as the disease progresses . Although early research suggested that decreases in dopamine and norepinephrine were involved in the development of depression in PD, recent literature suggests that serotonin plays a more prominent role . The presence of poor sleep and mood disturbances appears to have a reciprocal relationship, with the presence of one appearing to worsen the other . One study evaluated 98 patients with and without PD using the Insomnia Severity Index and Beck Depression Inventory to measure the impact of insomnia on depression . Total sleep time in patients with PD appeared to have a greater correlation with depression severity than that in controls which could reflect a synergistic effect of depression and PD on sleep duration .
Fig. 1
Treatment flow chart for insomnia in Parkinsons disease . Motor symptoms from PD such as tremor, dystonia, and rigidity can contribute to insomnia. The treatment of nocturnal symptoms typically employs long-acting forms of antiparkinsonian medication to last through a night of sleep. Nocturia is a symptom of PD that can significantly disrupt sleep and may be treated with behavioral modification and medications with low side effect profiles. Mood disturbances commonly contribute to insomnia and may be treated with a combination of nonpharmacologic measures and antidepressant medication
