Adverse Event Reporting And Harms
The STARTUP trial involves treatments that are well established in clinical practice therefore, AEs will be those observed in everyday practice associated with the condition. Expected AEs arising from the treatments are noted below and thus will not be collected as AEs but noted in the weekly follow-up data collection.
Urinary tract infection
All AEs and serious AEs will be assessed for seriousness, causality, severity and expectedness and will be reported to the relevant regulatory bodies.
How Does Parkinsons Affect The Bowel
Two out of three people with Parkinsons disease suffer from constipation, and the symptom can occur long before the diagnosis is made. Constipation is one of the most common non-motor symptoms of this condition.
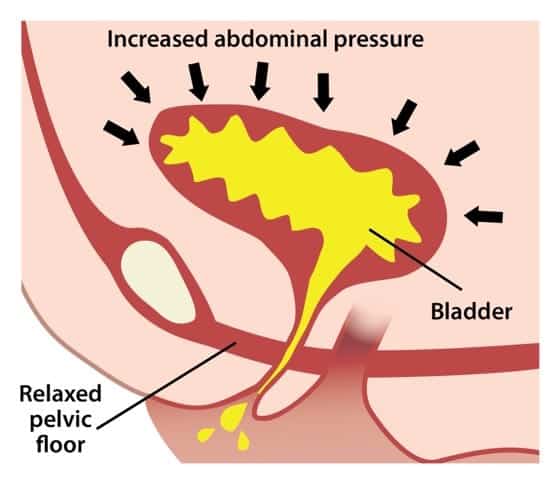
Many patients find it embarrassing to talk about their bowel problems, but it is important to seek help in managing constipation. Left untreated, constipation can lead to other problems. You may feelunwell and nauseous, exacerbating the constipation as you dont feel like eating or drinking.Constipation can also cause overactive bladder and urinary incontinence due to mechanical pressure on the bladder. Sometimes constipation makes it difficult to empty your bladder, and when urineremains in the bladder there is a risk of urinary tract infections.
We spoke to Ethan and Susan about their symptoms and how they manage it heres an excerpt from our free guides: Bladder and Bowel dysfunction when you have Parkinsons Disease
Ethans story
Susans story
Female and male anatomy are different, and the effects of Parkinsons disease may have different effects when it comes to bladder and bowel dysfunction.
The bladder and bowel also interact and effect the functioning of these processes. In these free guides, we look at the symptoms, effects and therapies available to manage this condition.
Bladder and Bowel dysfunction when you have Parkinsons Disease
Parkinsons Disease And Voiding Dysfunction
In this 54-minute webinar, urologist Dr. Sidney Radomski explains how voiding function is affected by Parkinsons disease in both men and women. He discusses how an enlarged prostate contributes to voiding problems and management options of voiding dysfunction for those with Parkinsons disease and MSA.
Read Also: Can An Mri Diagnose Parkinson’s
Way Of Producing Adult Nerve Cells Aids Memory Eases Anxiety In Mice
In a 2019 article for the University of Michigans health blog, author Jane Racey Gleeson noted that For PD patients, bladder issues are often due to fluctuations in dopamine levels affecting the bladder muscles and nerves, which are critical to how it functions. PD is also thought to impact the nerve pathway between the bladder and the area of the brain that controls bladder function.
My sister says that her bladder medication helps with her urgency issues most of the time, but not always. She wears incontinence pads, especially at nighttime.
All of this is so embarrassing, Bev said. I never thought this would be such a problem for me.
In addition to medication, other treatments for bladder control include deep brain stimulation and kegel exercises, which help strengthen the pelvic floor muscles that surround the bladder. Implants and percutaneous tibial nerve stimulation are also options.
Managing bladder problems can pose additional challenges for people with PD. Complicating the urgency issue are Bevs mobility problems. She cant always move quickly enough to get to the bathroom in time. I know that this is very frustrating for her.
Although this was a sensitive topic to write about, both Bev and I wanted others who may be experiencing the same issues to know theyre not alone.
You May Like: Signs Of Dehydration In Elderly With Dementia
Warning Disclaimer Use For Publication
WARNING: Please DO NOT STOP MEDICATIONS without first consulting a physician since doing so could be hazardous to your health.
DISCLAIMER: All material available on eHealthMe.com is for informational purposes only, and is not a substitute for medical advice, diagnosis, or treatment provided by a qualified healthcare provider. All information is observation-only. Our phase IV clinical studies alone cannot establish cause-effect relationship. Different individuals may respond to medication in different ways. Every effort has been made to ensure that all information is accurate, up-to-date, and complete, but no guarantee is made to that effect. The use of the eHealthMe site and its content is at your own risk.
If you use this eHealthMe study on publication, please acknowledge it with a citation: study title, URL, accessed date.
Recommended Reading: Best Balance Exercises For Parkinson’s Disease
Urinary Tract Infection In Parkinsons Disease
Article type: Review Article
Authors: Hogg, Elliota | Frank, Samuela | Oft, Jillianb | Benway, Brianc | Rashid, Mohammad Haruna | Lahiri, Shourid*
Affiliations: Department of Neurology, Cedars-Sinai Medical Center, Los Angeles, CA, USA | Department of Infectious Diseases, Cedars-Sinai Medical Center, Los Angeles, CA, USA | Department of Urology, Cedars-Sinai Medical Center, Los Angeles, CA, USA | Departments of Neurology, Neurosurgery, and Biomedical Sciences, Cedars-Sinai Medical Center, Los Angeles, CA, USA
Correspondence: Correspondence to: Shouri Lahiri, MD, Departments of Neurology, Neurosurgery, and Biomedical Sciences, Cedars-Sinai Medical Center, 8700 Beverly Blvd., Los Angeles, CA 90048, USA. E-mail: .
Keywords: Parkinsons disease, urinary tract infection, delirium, falls, exacerbation
DOI: 10.3233/JPD-213103
Journal: Journal of Parkinsons Disease, vol. Pre-press, no. Pre-press, pp. 1-15, 2022
Abstract
Recommended Reading: Azithromycin Urinary Tract Infection Dose
Information You Can Give The Doctor
A doctor can help identify the underlying cause of incontinence for treatment. A doctor can help write up a treatment plan to help cure or manage this condition. Bring notes to the appointment to help the doctor identify the underlying cause. Here are some things you may want to take note of:
- how long the person has been experiencing incontinence symptoms
- if the person has had episodes of incontinence in the past
- whether theyre experiencing urinary incontinence, fecal incontinence, or both
- whether its a trickle or a flood
- if incontinence is more pronounced at certain times of the day or night
- physical or mental barriers youve observed
- typical diet and how much fluid is consumed
You can also reach out to other health professionals for support. A nurse can provide advice on hygiene and management. A physical therapist can tell you more about equipment and adaptions. Talk to the doctor for recommendations.
Recommended Reading: Parkinsons Donations In Memory Of
Also Check: What’s The Treatment For Parkinson’s Disease
Cardiovascular Dysautonomia And Nocturia
An association is known to exist between orthostatic hypotension and nocturia, and nocturnal polyuria. In health, blood pressure is known to decrease at night, and this is often absent in patients with PD reporting autonomic failure. This may be mediated through inappropriate mineralocorticoid receptor activation. Consequent to this, pressure natriuresis occurs, resulting in increased urine output and the patient reports nocturia. OH and supine hypertension frequently coexist in PD, and older age, akinetic-rigid motor subtype, and pre-existing hypertension are independent risk factors for supine hypertension. Improvement of nocturia, however, has not been a consistent finding in studies evaluating treatments for supine hypertension,, , and therefore cardiovascular dysautonomia is likely to be only one of several mechanisms responsible for nocturia in PD.
Parkinsons Disease And Your Bladder
Many diagnosed with Parkinsons disease experience urinary tract issues. A Michigan Medicine urologist discusses treatment options for patients to consider.
Anne Pelletier-Cameron, M.D., often jokes to her patients that shes a female plumber of the lower urinary tract. On a more professional note, however, shes a urologist in the Michigan Medicine Department of Urology.
In this role, Pelletier-Cameron treats patients with a variety of lower urinary tract symptoms. Some of her patients have been diagnosed with Parkinsons disease, a progressive nervous system disorder that impacts movement. But the breakdown of nerve cells that characterize Parkinsons disease can also cause non-movement symptoms, including bladder issues.
Half of all women and 17% of men will experience urinary incontinence, or the inability to hold urine, she says, noting that for Parkinsons disease patients, those numbers escalate.
Many of my PD patients end up having other bladder problems, including issues with urgency and frequency, says Pelletier-Cameron. Nocturia, or the need to urinate many times during the night, is also common, along with difficulty in emptying the bladder.
Pelletier-Cameron says the impact of bladder symptoms cant be ignored.
You May Like: Drugs Cause Parkinsons Disease
Recommended Reading: What Are The Different Forms Of Parkinson’s Disease
Signs Of Parkinsons Disease
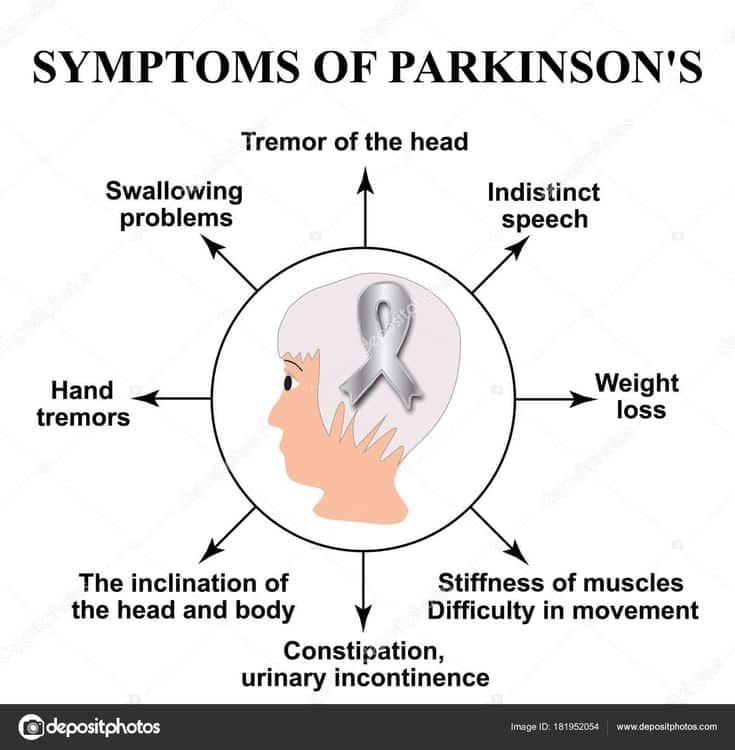
This condition is known for its three hallmarksymptoms:
- Muscle stiffness
But youll find a host of other symptoms that can appeardepending on the stage of illness and what area of the brain is currentlyaffected. This is why symptoms can varywidely between patients, but the progression of the disease is inevitable.
A Parkinsons diagnosis is far from simple. It often takesyears to arrive at a certain conclusion, because there is no single diagnostictest. Its a matter of assessing progressive symptoms and ruling out similarillnesses.
Treating And Managing Bladder Problems
It is important to discuss any bladder difficulties, including those listed below, with your doctor, even if this may appear embarrassing. Your doctor will then be able to properly assess and treat any problems, for example:
- inability or difficulty emptying the bladder even when it feels full
- significant, uncontrolled leakage of urine at any time
- unusually frequent urination
- an urgent, immediate need to urinate, or urine leaking if you do not immediately do so
- pain when urinating.
It may be helpful to write notes to discuss with your doctor, for example, the type of difficulties experienced, their frequency, when you first noticed a change, and your normal eating and drinking habits.
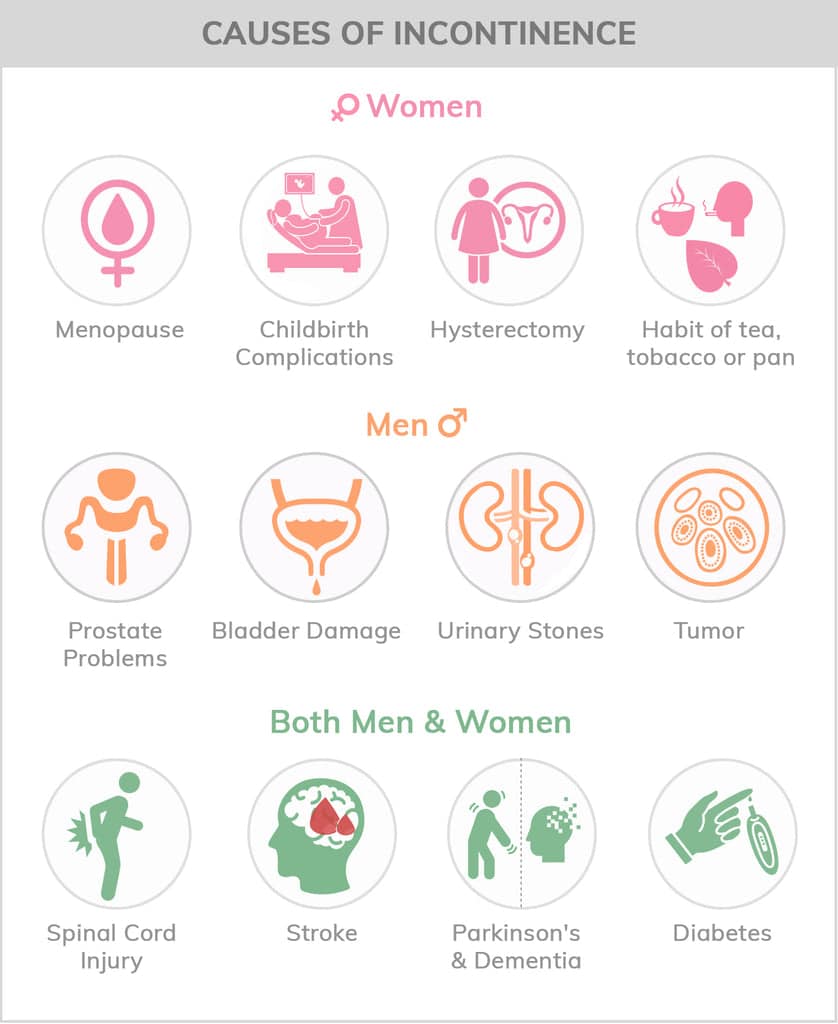
Bladder problems can occur for a number of reasons, so the first approach will be to eliminate causes other than Parkinsons, such as urinary infections and prostate problems in men.
Dont Miss: Weighted Silverware
You May Like: Does Parkinson’s Cause Muscle Wasting
Parkinsons Disease And Incontinence: Why It Happens And How To Cope
Constipation is a common side effect of Parkinson’s disease, but about 30-40% of patients also experience urinary difficulties, according to the Parkinson’s Foundation. A sudden or immediate urge to urinate is more than annoying. Without diagnosis and treatment, accidents may prevent you from running errands, visiting friends, or doing other activities you enjoy.
Fortunately, there are things you can do to reduce accidents, strengthen your pelvic floor, and improve your quality of life. In this article, we highlight symptoms to watch out for, discuss healthy lifestyle changes that you can make, and feature some of our best-selling products.
Strategies For Managing Nocturia In Pd
Despite the high prevalence of nocturia and impact on QoL, treatment options for managing this problem are currently limited and are often poorly tolerated or ineffective in PD. Guidance on nocturia treatment is limited, and most treatment options are derived from guidance around general management of urinary symptoms in neurological patients., ,
Recommended Reading: Parkinson’s Leg Cramps Treatment
The Impact Of Nocturia
Most studies have demonstrated that nocturia has a significant negative impact on quality of life., Awakening once at night is considered to be normal by many, and the degree of bother associated with nocturia increases with the frequency of nocturia. A recent population-based study demonstrated that having two voids or more per night was associated with impaired health-related quality of life . A number of community-based studies have demonstrated that a high proportion of patients with nocturia perceive this to be a troublesome complaint. In a large study, urinary incontinence was found to be major predictors of QoL in patients with PD using the 39-item Parkinson’s Disease Questionnaire however, the question regarding nocturia was not specifically evaluated in this study.
Few studies have evaluated the bother associated with nocturia in patients with PD, and nocturia was reported to be bothersome in 50% in one questionnaire-based study. QoL has been shown to be poor in PD patients reporting nocturia. In general, LUT symptoms have an immense impact on QoL measures, early institutionalization, and health-related costs. There exists an association between nocturia and the risk for falls and hip fractures. This becomes particularly relevant to PD where patients are at risk for falls, and a prevalence of 54% in PD patients compared to 18% in age-matched healthy participants was reported in one study.
Evaluating And Treating Urinary Issues In Parkinsons Disease Multiple System Atrophy And The Other Atypical Parkinsonism Disorders
In this hour-long webinar, neuro-urologist Ekene Enemchukwu, MD focuses on urinary incontinence, overactive bladder, urinary retention, and other urinary issues in PD, MSA, and the atypical parkinsonism disorders. Following the presentation, moderator Candy Welch, Brain Support Networks MSA caregiver support group leader, asks Dr. Enemchukwu many questions submitted by webinar participants.
You May Like: What Foods Should Be Avoided When Taking Levodopa
Recommended Reading: Diagnosis And Treatment Of Parkinson Disease
What Increases The Risk For Incontinence
Certain factors can also increase a persons risk for incontinence. These factors include:
- being overweight, as weight puts pressure on the bladder
- age, as older adults tend to have weaker bladder muscles
- pregnancy and childbirth, which can affect the pelvic floor and bladder muscles
- menopause, as hormones affect the bladder
- enlarged prostate or prostate surgery
- certain medications
Eligibility Criteria And Study Selection
Studies were eligible if they met the following criteria: published in peer-reviewed English journals participants were diagnosed according to UK Parkinson’s Disease Society Brain Bank Diagnostic Criteria or MDS clinical diagnostic criteria for Parkinson’s disease reporting the prevalence of LUTS or LUTS subtypes LUTS or LUTS subtypes assessed by validated scales administered by experienced clinicians, self-report questionnaire, or published criteria from classification codes/definition prospective cohort study or cross-sectional study.
The studies were excluded if they: did not provide full text included insufficient or unclear fragmented data for analysis enrolled patients who have been diagnosed with prostate carcinoma, uncontrolled diabetes, as well as any other diseases that cause urinary problems, or taken drugs such as diuretics with small sample size . duplicated publications systematic reviews, meta-analyses, letters, protocols. When results on the same dataset were reported in several publications, only the most complete publication was included in the analysis. Two independent observers evaluated the results and resolved any disagreement by discussion or with recourse to a third arbitrator .
Don’t Miss: What Are The Signs Of Parkinson’s Symptoms
Helping Someone With Pd
While not everyone with PD will have related bladder issues, recent studies show that up to 40% of people will. Only about 15% of individuals will have severe Parkinsons-related incontinence. Whether or not someone is dealing with severe incontinence, as a professional or family caregiver many steps can be taken to improve the quality of life for those with bladder issues.
Learning more about urinary incontinence and PD is the first step to helping someone struggling with both. With research, you can learn the current treatments for frequent urination and suggestions to improve managing incontinence and heighten the quality of life. Understanding the problem can help everyone, including you, so simply being an advocate is a great place to start.
Recommended Reading: Protein And Parkinsons Medication
How Might Parkinsons Affect Bladder Problems
Bladder difficulties can be common in Parkinsons, particularly in the later stages of the condition. The loss of dopamine and the resulting interruption of signals from the brain can mean that messages telling the bladder to retain or expel urine are disrupted.
However, it is important to stress that bladder problems are not inevitable in Parkinsons. If difficulties do arise, especially in older people, they may be caused by factors totally unrelated to the condition, so a thorough medical evaluation should be carried out with any appropriate tests.
Bladder problems associated with Parkinsons include:
Also Check: Parkinsonâs Disease Research Paper
Read Also: Can Acupuncture Help Parkinson’s
Urinary Dysfunction And Parkinsons
This one-page fact sheet explains that urinary dysfunction is one of several non-motor symptoms of Parkinsons disease that are the result of Parkinsons impairing proper function of the autonomic nervous system, especially in later stages of the disease process. Several types of urinary dysfunction and treatment options are outlined.
Assignment Of Interventions: Allocation
Sequence generation
Participants who provide written informed consent will be randomised using a computer generated system to either TTNS intervention or non-active stimulation arm and will be minimised on two factors: severity of urinary symptoms, as reported at study baseline by the IPSS in the Clinical Assessment Form, that is, mild, moderate or severe and status on antimuscarinic medication, that is, treatment naïve, failed or continuing such treatment.
Concealment mechanism
A web-based randomisation system will be used.
Implementation
Implementation will be by staff at the Centre for Healthcare Randomised Controlled trials Clinical Trials Unit at Aberdeen.
You May Like: Is Dementia Part Of Parkinson’s
Prevalence Of Luts In Pd
The pooled prevalence of LUTS was 61% .
Figure 2. Forest plot showing the prevalence of LUTS , urinary incontinence , urinary retention , and post-void residual volume 100 ml in PD patients.
Figure 3. Frequency of LUTS or its subtypes in PD patients. The x-axis shows different kinds of LUTS while the y-axis shows the percentage.
For subgroup analyses, we found that H& Y stage, gender, and different diagnostic tools may be cause of heterogeneity related to the prevalence of LUTS . The pooled prevalence of LUTS was 59% in PD with H& Y stage < 3, whereas 70% in PD with H& Y stage 3. The pooled prevalence of LUTS was 62% in male PD patients, whereas 54% in female PD patients.
Table 2. Prevalence of LUTS or subtypes: results of the subgroup analysis.
No significant publication bias was found by Begg’s funnel plot .
What Kind Of Incontinence Does Parkinsons Disease Cause
Incontinence is considered a non-motor symptom of Parkinsons Disease, which is mainly considered to be a movement disorder. This means that much more research and emphasis has gone into the more noticeable motor issues that define the disease and not the prominent non-motor problems that accompany the disease.
This also means that the medication prescribed already to control a persons motor functions doesnt necessarily have any effect on non-motor-related symptoms, such as incontinence, which need to be addressed separately and discussed with your doctor. Identifying and treating incontinence issues arent just about increasing personal comfort. Its about dignity. Its about confidence. Its about quality care.
Also Check: Gadget For Parkinson’s Tremors