Impact On Families And Carers
Informal carers spendmany hours dailyproviding care for people living with PD.This can be overwhelming. Physical, emotional and financial pressures can cause great stress to families and carers, and support is required from the health, social, financial and legal systems. Useful support resources from other conditions can be drawn upon, such as WHOs iSupport programme for dementia.
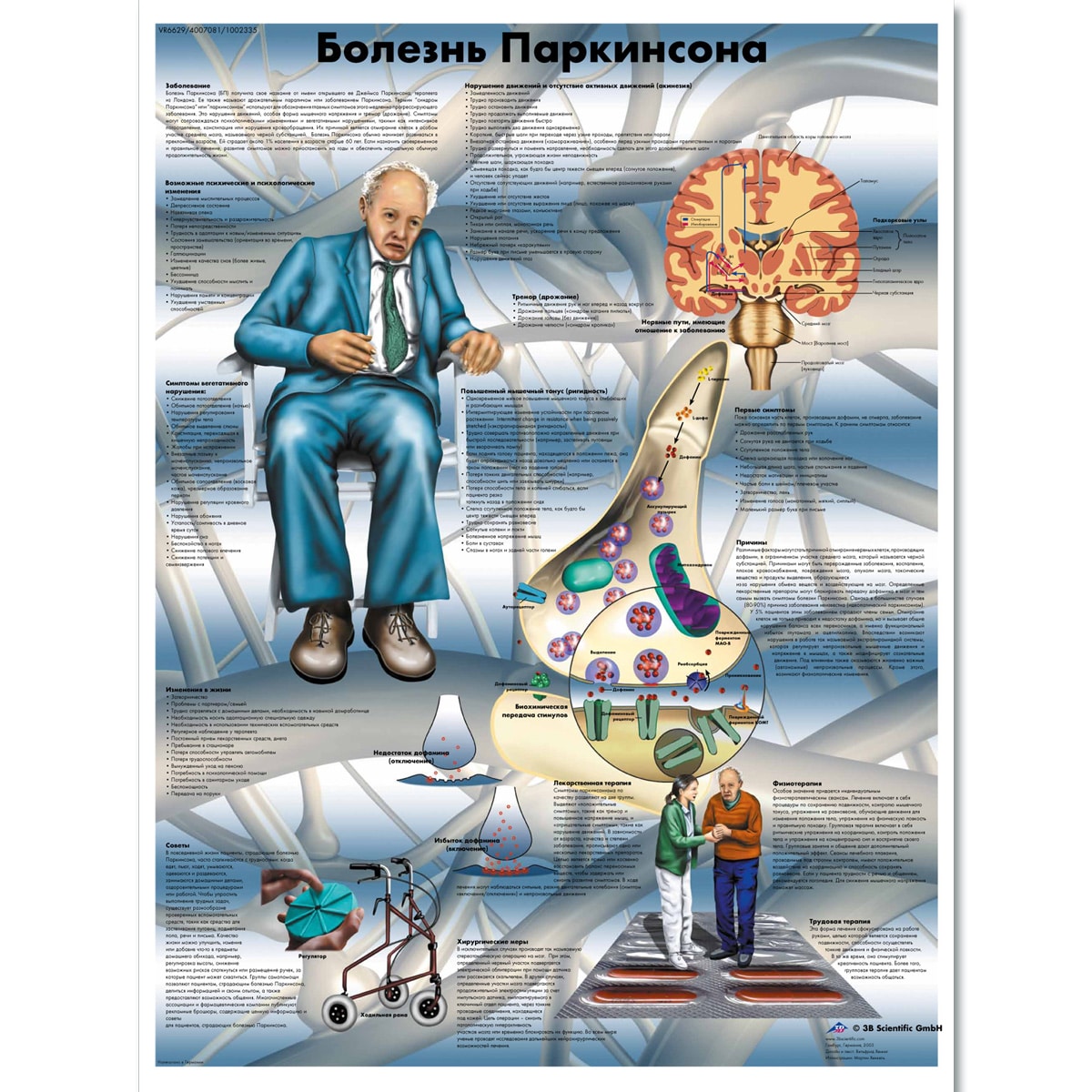
Symptoms Of Other Types Of Parkinsonism
Parkinsons disease and other types of parkinsonism share some common symptoms, such as stiffness, tremors, and slow movement. However, other types of parkinsonism tend to progress more quickly than Parkinsons, and people with other types generally start experiencing balance issues sooner. Additionally, people with other types of parkinsonism show only a short-term response if any to levodopa, a common medication for Parkinsons.
Is Rls More Common In Pd
But what about the other possibility? Do patients with PD have an increased risk of RLS over the general population? Is it the same RLS as the person without PD has, or is it different? These questions have been difficult to answer. Of course, since PD affects about 1.5% of the elderly, and RLS in about 4-10% of the population, there will be some coincidental overlap. In addition to this however, patients with PD can have sensations that feel like RLS when their dose of dopamine medication is wearing off. These sensations are not truly RLS since they do not have the key features of RLS described above and fluctuate with medication timing, but they can be easily confused with RLS by the person with PD.
Studies of people with PD that assess for RLS and compare to a control group are hindered by the fact that the majority of patients with significant PD are under treatment with medications that affect RLS. Over the years, there have been multiple studies investigating whether RLS is more common in PD than in the general population. Different studies come to different conclusions. Studies conducted in which a group of people with PD are directly compared to a group of people without PD typically show that RLS is more common in PD than the general population.
Read Also: What Do Parkinson’s Tremors Look Like
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Whats The Difference Between Lewy Body Dementia Parkinsons Disease And Alzheimers Disease
Lewy body dementia is an umbrella term for two related clinical diagnoses: dementia with Lewy bodies and Parkinsons disease dementia. These disorders share the same underlying changes in the brain and very similar symptoms, but the symptoms appear in a different order depending on where the Lewy bodies first form.
Dementia with Lewy bodies is a type of dementia that causes problems with memory and thinking abilities that are severe enough to interfere with everyday activities. It specifically affects a persons ability to plan and solve problems, called executive function, and their ability to understand visual information. Dementia always appears first in DLB. The motor symptoms of Parkinsons such as tremor, slowness, stiffness and walking/balance/gait problems usually become more evident as the disease progresses. Visual hallucinations, REM sleep behavior disorder, fluctuating levels of alertness and attention, mood changes and autonomic dysfunction are also characteristic of DLB.
Finally, Alzheimers is characterized by different abnormal clumps called amyloid plaques, and jumbled fiber bundles called tau tangles. These microscopic structural changes in the brain were discovered by Dr. Alois Alzheimer in 1906. These plaques and tangles, together with loss of connections between nerve cells, contribute to loss of coherence and memory, as well as a progressive impairment in conducting normal activities of daily living.
Recommended Reading: How Long Has Michael J Fox Had Parkinson’s Disease
Characteristic Clinical Features Of Pd
PD can be diagnosed with considerable accuracy, particularly by neurologists specializing in diagnosis and management of movement disorders , when robust clinical criteria are used such as those of the Queen Square Parkinson Disease Brain Bank, which have inclusion criteria and exclusion criteria as well as presence of supportive features . Asymmetry is an important supportive feature in that the other major degenerative parkinsonian disorders MSA and PSP are usually symmetrical. Response to dopamine replacement therapy is typical of PD, whereas MSA and PSP have limited response to such therapy. The exclusion criteria also include absence of family history of movement disorder, but this is criterion is often ignored today given increasing evidence of genetic determinants of PD .
Braak Pd Staging Scheme
Although the staging scheme of Braak and co-workers should be considered tentative, it nevertheless, has prompted considerable debate in the field and reawakened recognition of early nonmotor clinical features of PD . Subsequent iterations of the Braak scheme proposed that autonomic neurons in peripheral nervous system may be affected before involvement of the central nervous system and this has prompted recognition that PD is a multiorgan disease process, not merely a disorder of central nervous system . Moreover, it has fed the debate on cell-to-cell transmission of unknown putative disease factors , especially given the fact that fetal mesencephalic intrastriatal transplants to treat PD have been shown to develop Lewy body pathology , possibly by cell-to-cell transmission .
Recommended Reading: Do Parkinsons Tremors Stop When Sleeping
You May Like: Is Parkinson Disease Genetically Transmitted
Jellinger Staging Scheme For Msa
It has been more challenging to stage pathology in MSA and PSP because of the rarity of these disorders and because of their inherent variability. Nevertheless, Jellinger has proposed a staging scheme for MSA that scores severity of striatonigral degeneration and olivopontocerebellar atrophy , each on a three-point scale. The final classification is indicated by an OPCA + SND score . Halliday and co-workers proposed a similar scheme and graphically illustrated the two major MSA types, as well as the overlap in OPCA and SND system degenerations. Ozawa and colleagues used a semiquantitative scoring scheme for lesion density and found differences in the proportion of MSA types in Japanese compared to European autopsy cohorts, with far more OPCA in Japanese . Detection of MSA in neurologically normal individuals is extremely uncommon , and large numbers of such cases would be needed to determine the earliest sites of involvement to develop a staging scheme for MSA analogous to the Braak staging scheme for PD.
Parkinsons Disease: Symptoms Stages And Treatment
Parkinson’s disease usually begins after age 60, gradually progressing over the years. Some people can have early-onset Parkinson’s disease, starting in their 30s or 40s. It is primarily a movement disorder characterized by resting tremors and slowness and stiffness of movement.
In the late stages of the disease, Parkinson’s dementia can develop. But most people who have Parkinson’s disease do not develop dementia as a part of the condition.
Don’t Miss: Can You Live A Normal Life With Parkinson’s
What Happens In Parkinsons Disease
Substantia nigra is a small part of the brain. These parts secrets a chemical- dopamine. Dopamine is a hormone and neurotransmitter. It is responsible for many activities in the brain and body. This is also synthesized in kidneys along with the brain and other tissues. But external dopamine, other than produced in the brain, cannot cross the blood-brain barrier. Therefore external source is of least use.
When this neurotransmitter is not efficient in working. It leads to the problem of Parkinsons disease.
This happens in two ways.
Firstly, when dopamine is not able to communicate with the neural cells. And secondly, when production of the dopamine is not good. In both conditions, dopamine is not able to work efficiently. This causes problems with the activities of the brain which control through dopamine.
Here we need to know a bit more about dopamine. So that we can understand activities of the dopamine in a better way. This will help us to find about the Ayurveda treatment for Parkinsons disease.
Parkinsonism And Parkinsons Disease Not The Same Thing
Dear Doctor: I was treated for pelvic cancer earlier this year, and ever since finishing chemo, Ive had problems with balance and movement. My doctor thinks it could be parkinsonism. Is that the same as Parkinsons disease? Did the chemo cause it?
Dear Reader: Although the two conditions share a similar name and similar symptoms, parkinsonism is not the same thing as Parkinsons disease. Rather, its a term that refers to any neurological condition that can cause the symptoms associated with Parkinsons disease.
For those of you who arent familiar with Parkinsons disease, its a progressive disorder of the nervous system that affects and interferes with movement. Symptoms arise due to disruption in a region of the brain that produces dopamine, a neurotransmitter that plays a big role in smooth and continuous muscle movement. When someone has Parkinsons disease, the cells in the brain that produce dopamine have either stopped working or have died. The cause of this disruption is not yet known.
There is no single test for Parkinsons disease. Diagnosis relies on a detailed medical history, a review of symptoms and various movement and neurological tests. The symptoms of Parkinsons disease, which tend to appear gradually, can be similar to several other neurological disorders. All of this makes diagnosis a challenge.
Read Also: Are Als And Parkinson’s Related
Glial Cytoplasmic Inclusions In Msa
Lantos and co-workers first described glial cytoplasmic inclusions in MSA . Glial cytoplasmic inclusions can be detected with silver stains, in particular, the Gallyas silver stain, but are best seen with antibodies to -synuclein and ubiquitin, in which they appear as flame- or sickle-shaped inclusions in oligodendrocytes. At the ultrastructural level, glial cytoplasmic inclusions are nonmembrane-bound cytoplasmic inclusions composed of 10 to 20nm diameter coated filament similar to the filaments in Lewy bodies .
Although most -synuclein inclusions in MSA are in oligodendroglial cells, certain neuronal populations are vulnerable to neuronal cytoplasmic and intranuclear inclusions, particularly those in the pontine base , inferior olive , and putamen. A few of the neuronal inclusions in MSA resemble Lewy bodies, but their anatomical distribution is distinct from neuronal populations vulnerable to Lewy bodies. Intranuclear -synuclein-immunoreactive inclusions are not found in PD.
Differential Diagnosis Of Parkinson Disease
Perhaps expression analysis of genes in brains of patients with various neurodegenerative and recognizing disease-specific patterns will in the future assist in differentiating PD from other parkinsonian disorders. For example, using microarray technology in SN samples from six patients with PD, two with PSP, one with FTDP, and five controls, Hauser and colleagues found 142 genes that were differentially expressed in PD cases and controls, 96 in the combination of PSP-FTDP, and 12 that were common to all three disorders. Further studies are needed to confirm this intriguing finding.
Claudia Trenkwalder, in, 2005
You May Like: Who’s At Risk For Parkinson’s Disease
Selection Of Regions Of Interest
18F-DMFP has a high binding affinity for dopamine transporters in the striatal region of the brain. For this reason, neuroimaging studies based on it usually focuses on that region. However, 18F-DMFP PET neuroimages contain a substantial part of the total intensity in regions other than the striatum. In order to reveal the most important regions to separate idiopathic PD from APS we carried out an univariate analysis. Specifically we performed a two-sample t-test comparing both populations under the hypothesis of data corresponding to idiopathic PD patients have lower intensity than those from APS patients. The test was carried out using the SPM software and a smoothed version of the neuroimaging data. The full-width at half maximum of the Gaussian smoothing kernel was fixed at 8 mm. The resulting map, thresholded at p< 0.001 , is shown in Figure 1.
Figure 1. t-test comparing patients with idiopathic PD and atypical parkinsonian syndromes. Regions in orange/yellow are significantly lower in idiopathic PD patients. Observe that most part of the thalamus, anterior cingulate gyrus and pars opercularis are covered by highlighted areas.
Finally, the t-test map was matched with the Automated Anatomical Labeling atlas and the regions of the atlas with the highest proportion of highlighted voxels in the t-test map were selected.
Also Check: Do People Die From Parkinsons Disease
About Cheryl Waters Md
Cheryl Waters MD FRCP, holds bachelors and masters degrees in Pharmacology from the University of Toronto, where she studied dopamine receptor function with Philip Seeman. She completed medical school at University of Toronto, an internship at University of Chicago, and returned to Toronto for Internal Medicine, Neurology and a fellowship in Clinical Pharmacology. She moved to California and developed the Movement Disorder Program at the University of Southern California. Dr. Waters then moved to New York to take on her current position as Chief of Clinical Practice and Services in the Division of Movement Disorders. She has been involved in research on the genetics of Parkinson’s disease and the treatment of this disorder. She has authored numerous articles and book chapters and a book in its seventh edition: Diagnosis and Management of Parkinson’s Disease. She has been an investigator in numerous studies involving a variety of new medical and surgical treatments. She is the first to hold the Albert B. and Judith L. Glickman Chair in Neurology.
Read Also: How Does A Person With Parkinson’s Feel
Macroscopic Pathologypd Msa Psp
PD is often unremarkable, with mild frontal atrophy in some cases. There is no significant atrophy of brainstem, and this can be useful in the differential diagnosis of PSP and MSA, in which there is midbrain atrophy in PSP and pontine atrophy in MSA. Sections of the brainstem usually reveal loss of the normally dark black pigment in the substantia nigra and locus ceruleus, but pigment loss in the substantia nigra is also characteristic of PSP and MSA. The loss of pigmentation correlates with neuronal loss of dopaminergic neurons in the substantia nigra and noradrenergic neurons in the locus ceruleus. Pigment loss in the locus ceruleus is consistent in PD, but less predictable in PSP and MSA.
MSA-P has atrophy and brownish discoloration of the posterolateral putamen , the brown color correlating with increased iron pigment. In cases with significant cerebellar signs, there is also atrophy of the pontine base and atrophy and gray discoloration of the cerebellar white matter. More subtle atrophy is noted in the medulla and the cerebellar cortex.
What Can I Expect If I Have This Condition
All cases of parkinsonism regardless of the specific condition involved slowed movements plus other related symptoms. What you can expect depends on the specific condition you have and what treatments if any that you receive. Your healthcare provider is the best person to tell you more about what you can expect if you have parkinsonism.
How long does parkinsonism last?
How long parkinsonism lasts depends on the specific condition. Nearly all conditions that fall under parkinsonism are life-long conditions. One condition that isn’t always a life-long problem is drug-induced parkinsonism.
Because parkinsonism includes so many different conditions, it’s best to talk to your healthcare provider about how long your condition will last. They can best explain what you can expect, including the likely timeline for how this condition will affect you.
Whats the outlook for this condition?
The outlook for parkinsonism depends on your condition, how severe it is, and whether or not it’s treatable. Many forms of parkinsonism aren’t deadly on their own but can contribute to deadly complications. An example of this is trouble swallowing, a common symptom of Parkinsons disease and other forms of parkinsonism, and how this increases your risk of developing pneumonia.
You May Like: Big Exercise Program For Parkinson’s
Multiple System Atrophy Formerly Called Shy
As predicted by the name of this parkinsonism, multiple system atrophy affects multiple systems of the body. It affects both the motor skills movement system and the involuntary system of the body. Though the symptoms can often be treated with medications, there is no cure. In addition, there are no drugs that are able to slow the progress of MSA.
When Should I See My Healthcare Provider
You should see your healthcare provider as recommended or if you notice changes in your symptoms, especially if the symptoms start to interfere with your life and routine. You should also see your provider if you notice any changes in the effectiveness of your medication.
When should I go to ER?
Your healthcare provider can give you guidance and information on signs or symptoms that mean you need to go to the hospital or get medical attention. In general, you should get medical attention if you fall, especially when you lose consciousness or might have an injury to your head, neck, chest, back or abdomen.
A note from Cleveland Clinic
Parkinsonism is a term that covers a wide range of conditions that affect your ability to move and live independently. While these conditions all share certain similarities, they also can have major differences from each other. If youre diagnosed with parkinsonism, its important to talk to your healthcare provider about what condition you have , and what that diagnosis means for you. Not all parkinsonism conditions are the same, so understanding your specific case can make a big difference in managing it and how it affects your life.
Also Check: Tango For Parkinson’s Disease
