Impact Of Falls And Parkinson’s Disease
This 8-minute video alternates between an interview with a man sharing his experience of falling due to Parkinson’s disease, with a doctor, physical therapist and occupational therapist explaining why people with PD fall, the benefit of physical therapy and exercise before a person has ever fallen to prevent falls and what an occupational therapist can do to prevent falling at home and in the broader environment.
Further Testing In Parkinsons
In other situations, where perhaps the diagnosis is not as clear, younger individuals are affected, or there are atypical symptoms such as tremor affecting both hands or perhaps no tremor at all, further testing may help. For example, imaging can play a role in differentiating between essential tremor and Parkinsons. It can also be important to confirm what is initially a clinical diagnosis of Parkinsons prior to an invasive treatment procedure such as surgical DBS
Recurrent Falls In Parkinsons Disease: A Systematic Review
Natalie E. Allen
1Clinical and Rehabilitation Sciences Research Group, Faculty of Health Sciences, The University of Sydney, P.O. Box 170, Lidcombe, NSW 1825, Australia
Abstract
Most people with Parkinsons disease fall and many experience recurrent falls. The aim of this review was to examine the scope of recurrent falls and to identify factors associated with recurrent fallers. A database search for journal articles which reported prospectively collected information concerning recurrent falls in people with PD identified 22 studies. In these studies, 60.5% of participants reported at least one fall, with 39% reporting recurrent falls. Recurrent fallers reported an average of 4.7 to 67.6 falls per person per year . Factors associated with recurrent falls include: a positive fall history, increased disease severity and duration, increased motor impairment, treatment with dopamine agonists, increased levodopa dosage, cognitive impairment, fear of falling, freezing of gait, impaired mobility and reduced physical activity. The wide range in the frequency of recurrent falls experienced by people with PD suggests that it would be beneficial to classify recurrent fallers into sub-groups based on fall frequency. Given that there are several factors particularly associated with recurrent falls, fall management and prevention strategies specifically targeting recurrent fallers require urgent evaluation in order to inform clinical practice.
1. Introduction
Recommended Reading: How Quickly Do Parkinson’s Symptoms Progression
Prospective Assessment Of Falls
A fall was defined as an unexpected event where the person inadvertently came to rest on the ground or other lower level not due to a major intrinsic or extrinsic event.
Following baseline screening, each subject was given a set of weekly prepaid postcards to return for one year. On each card subjects had to write a single number documenting the number of occasions that they had fallen in the previous week. Subjects were encouraged to include anything that might constitute a fall, including slips, trips, and stumbles. Assistance from carers in this respect was obtained where necessary.
A positive number recorded on a card was followed up by telephone to outline the exact circumstances of the fall event and to ensure that this event met the definition of the fall outlined above. If cards were not returned one week after expected, this would also prompt telephone contact to inquire about the number of falls in the week in question.
Problems With Blood Pressure
Problems with blood pressure can affect people generally as they get older, but some Parkinsons medication can cause side effects, including problems with blood pressure. This can lead to dizziness and falls. If youve felt dizzy, or fallen because of dizziness, ask your GP or practice nurse to check your blood pressure both when youre sitting and standing, to see if its too low.
Drugs used to treat other medical conditions, such as high blood pressure, can potentially make dizziness worse, especially if you are losing weight or not eating and drinking as well as you used to.
Postural hypotension is a sudden drop in blood pressure when changing position, for example getting up out of a chair. It can make you feel very light-headed, which will affect your balance. You may experience postural hypotension as a symptom of Parkinsons. But it can also be caused by the drugs used to treat Parkinsons.
You can avoid some dizzy spells by taking your time. For example, before you get out of bed, sit with your feet touching the floor for a few minutes to get your blood flowing. Then stand up slowly, but try not to walk away immediately stand for a while until you feel steady.
Also Check: Alan Alda Parkinsons Diagnosis
Read Also: Environmental Causes Of Parkinson’s Disease
It’s Not All Dopamine: Possible Mechanisms And Interventions For Falls In Pd
In this 1-hour talk Rober Albin, movement disorder specialist and researcher, describes the impact of dopamine and acetylcholine in Parkinson’s through some animal and human trials. Research has found a nicotine-like drug is very safe, well tolerated and seems to improve attention in those with PD.
Falls Prevention Conversation Guide For Caregivers
This 13-page toolkit walks caregivers through a 3-step process using worksheets to: 1. Recognize physical, behavioral and environmental factors that may lead to a fall, 2. Have a conversation about risk factors specific to your situation, and 3. Develop a 7-step action plan for minimizing those risk factors.
Read Also: Can Thyroid Problems Mimic Parkinson’s
Equipment And Walking Aids
You might find that equipment can help you to walk, such as a walking stick or a rollator .
Before you start using a walking aid, it’s very important to get advice from a physiotherapist. Some walking aids aren’t recommended for people with Parkinsons as they can affect your walking pattern and make you more likely to fall. But, the correct walking aid can increase your confidence and help you to lift your feet better.
Support For People Living With Parkinsons Disease
While the progression of Parkinsons is usually slow, eventually a persons daily routines may be affected. Activities such as working, taking care of a home, and participating in social activities with friends may become challenging. Experiencing these changes can be difficult, but support groups can help people cope. These groups can provide information, advice, and connections to resources for those living with Parkinsons disease, their families, and caregivers. The organizations listed below can help people find local support groups and other resources in their communities.
Also Check: Toxic Causes Of Parkinson Disease
Read Also: What To Expect Living With Parkinson’s
How Can Falls Be Prevented
In this 6:30-minute video Dr. John Nutt explains the three most common causes of falling in those with Parkinsons is postural change, freezing and low blood pressure. Your doctor may be able to reduce your risk. A physical therapist can teach you how to move in ways that lessen your risk of falling as well as help you prevent falling by making changes to your home, learn to use an assistive device or recommend how a wheelchair can be helpful.
Inclusion And Exclusion Criteria
Quantitative systematic reviews , mixed-methods systematic reviews , or pooled analyses and research syntheses investigating the effectiveness of non-pharmacological falls prevention interventions for people with MS, PD and stroke were considered for inclusion in this umbrella review. Reviews published in the English language were included and authors of potentially relevant reviews published in a different language were contacted to ascertain if a copy of the review was available in English. No restriction was placed on year of publication of the review. In instances where a systematic review was an update of a previous review, the most recent version was included and the older version excluded. For the purposes of this umbrella review, a review was classified as an update of a previous version if there were changes pertaining to new data, new methods, or new analyses, but the research question, objectives and inclusion criteria remained similar . In the case of new authors or a different research team updating an existing review, they had to clearly state that their review was an update and acknowledge the work of the authors on the previous edition .
The eligibility criteria based on population, intervention, comparator, outcome and study design are outlined below.
Population
Dont Miss: Who Has Parkinsons Disease
Read Also: How Did Michael J Fox Know He Had Parkinson’s
S For Preventing Falls Among Your Older Loved Ones
The six things caregivers can do to prevent falls starts with enlisting the help of the person at risk for falling. This webpage will tell you how and why you should ask about current health conditions, most recent eye checkup, medications, and notice if trouble standing or holding onto things or people while walking. Finally, it shares how to make a home a bit safer from falls.
Data Synthesis And Analysis
Given the heterogeneity in populations, outcomes and analyses, the findings of included reviews were primarily summarised using a narrative synthesis with the quantitative tabulation of results as appropriate. The primary analyses for this umbrella review were centred on type of neurological condition and type of intervention. Following this, cross-comparison of similarities and differences in the effect of different interventions between the three conditions were reported and discussed. The outcomes of each included systematic review were considered and discussed in the context of their methodological quality, as determined by the AMSTAR 2 and the GRADE algorithm.
Also Check: How Are You Tested For Parkinson’s
Shortcomings Of This Study
The authors recognise that there are shortcomings of this study.
It may be argued that subjects should have been assessed a certain time after taking their antiparkinsonian medication. This could not happen, largely for logistical reasons such as patient transportation and the need for patients to be assessed by a variety of professionals.
No controls were used. This was because the study was designed to be descriptive and to compare the differences between fallers and non-fallers with PD, rather than the healthy elderly population.
Despite the methods used for prospective assessment, some falls are still likely to have been missed. The high incidence of falls quoted is likely to be an underestimate of the number of falls that occurred. Perhaps only highly sophisticated long term mechanical monitoring methods would be able to give the true incidence, but these would be impractical.
The confidence intervals in the logistic regression model are wide probably due to the small numbers of subjects. All patients who were available to the authors were recruited, however, so this was unavoidable. Multicentre studies or perhaps meta-analysis would perhaps fully address these issues.
It should also be noted that 32 potential subjects did not participate. These patients were older with more severe disease of longer duration. If they had been included, the incidence of falls may have been even higher.
Parkinsons Disease And Movement Disorders Center
Our center provides compassionate and timely treatment to patients with movement disorders, such as dystonia, ataxia, essential tremor and similar conditions. But our mission goes beyond patient care excellence. By offering educational events and support groups, we empower patients and caregivers to become better partners in their health.
Don’t Miss: Is Cervical Dystonia Related To Parkinson’s
Parkinsons Disease: Preventing Falls & Maintaining Balance
This printable webpage recommends working with your doctor to ensure your medications and/or DBS are optimal and consulting with a physical therapist to assess your walking and balance. In addition it provides two lists of daily fall prevention: 1) How to prevent falls from common hazards around the home and 2) Tips for maintaining balance.
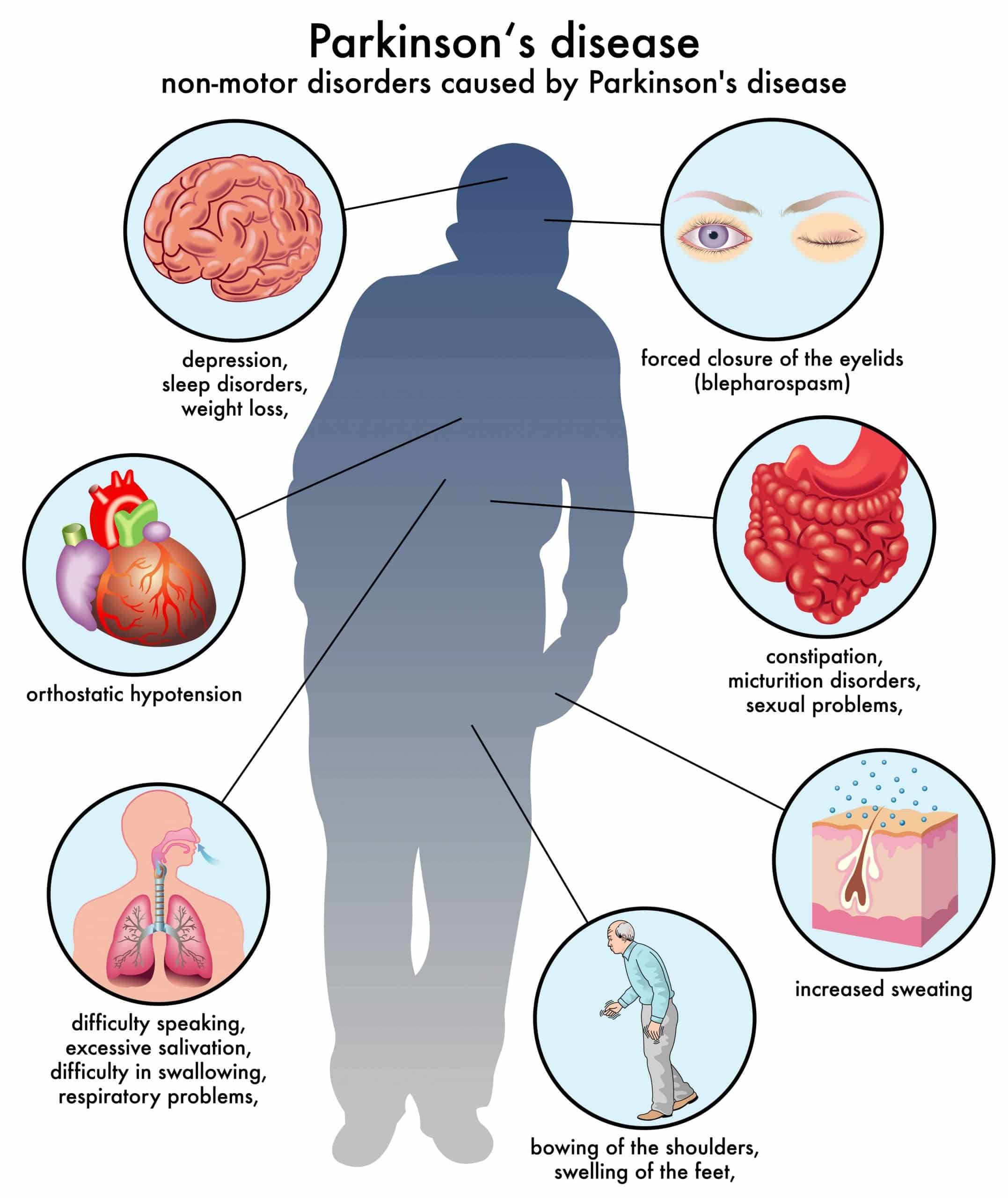
Potential Underlying Pathophysiological Mechanisms
Although falls are one of the key features of advanced PD, and dopaminergic medications can improve balance impairment in PD, postural instability in PD is comparatively less responsive to levodopa therapy than limb akinesia or tremor to levodopa therapy, and it is likely that other pathophysiological mechanisms are involved in gait disturbance in these patients., It has been postulated that noradrenergic deficits such as in the locus coeruleus and cholinergic pathways like the pedunculopontine have an important role. In support of the noradrenergic hypothesis, a large randomized controlled study using methylphenidate in advanced PD patients, improvements were observed for gait bradykinesia and freezing of gait. In animal models, in rats, dual cholinergic-dopaminergic lesions were found to result in falls more frequently than those with either cholinergic or dopaminergic lesions.
The findings of this study confirm from a clinical point of view that falls are associated with nonmotor features related to non-dopaminergic dysfunction, i.e., autonomic dysfunction, psychosis, sleep disorders, and cognitive impairment. All of these are thought to arise at least in part from deficits in the noradrenergic and cholinergic pathways with complex interaction of several neurotransmitter systems.,
Recommended Reading: Massage Therapy For Parkinson’s
Comparison Between Fallers And Non
Table 1 shows the differences in demographic and historical data between fallers and non-fallers. It should be noted that one subject reported 500 falls in the year before assessment otherwise, the range would have been 0100. Fallers had longer disease duration than non-fallers and were more likely to describe previous falls.
Table 1
Historical data and falls among 101 patients with Parkinsons disease
Table 2 shows the differences between fallers and non-fallers in disease severity and other rating scales. There is a strong association between disease severity and the risk of falling. This is particularly true with an MHY rating > 2.5 and with higher UPDRS subtotal II , subtotal III , or total UPDRS score. Cognitive impairment was also associated with increased GDS or PDQ = 8 and a risk of falls. One subject had an MMSE of 0 otherwise, the range would have been 1530.
Table 2
Disease severity and rating scales
Although there was no association between a worse shoulder pull and falling, there was an association between an increased number of falls and a positive shoulder pull, using the positive pull as the independent variable in a Mann-Whitney U test .
Table 3
Physiotherapy assessment and falls
Different sample sizes are quoted for the cardiovascular and autonomic assessments owing to different entry criteria and withdrawals. In these cases fractions and percentages are quoted . None of the cardiovascular or autonomic data were associated with falling.
Rates Of Falls And Recurrent Falls In Parkinsons Disease
Fourteen of the studies recorded fall rates using the gold-standard method of a falls diary, calendar or postcard . Several studies recorded falls via conducting telephone interviews at set intervals, ranging from monthly to three monthly or six monthly intervals. Other studies utilized responses to regular mail queries , monthly outpatient follow-up sessions , or medical record observation .
The proportion of participants who fell at least once during the reporting periods was highly variable , ranging from 35% to 90% , with an average of 60.5%. Recurrent fallers accounted for between 18% and 65% of participants and made up a large proportion of the fallers, ranging from 50% up to 86% of fallers .
The rate of falls per recurrent faller per year was found to be high, ranging from 4.7 to 67.6 falls per recurrent faller per year . An example of the very high rate of falls experienced by some individuals is reported by Goodwin et al. , where one participant fell 577 times in 20 weeks, which is approximately equivalent to 1500 falls in 1 year.
Read Also: Can Physical Therapy Help Parkinson’s Disease
Comparison Between Fallers And Nonfallers
Fallers were older and had longer disease duration and increased disease severity according to the UPDRS , Hoehn and Yahr and Schwab and England activities of daily living scores. In addition, fallers scored worse in the Mini-Mental State Examination and experienced a higher frequency of motor fluctuations, dyskinesia, and freezing of gait . Tremor as the initial predominant symptom was more frequent in nonfallers. Fallers were treated with higher doses of levodopa and more frequently received COMT inhibitors, central cholinesterase inhibitors, and atypical neuroleptics than nonfallers . Patients treated with central cholinesterase inhibitors had dementia associated with PD and those treated with quetiapine had hallucinations.
A Search For Sharpness
But it is the angles and sharpness of brain waves that could hold the key to detecting Parkinsons, according to the new studys findings, which appear in the journal eNeuro.
While working on his doctorate at the University of California, San Diego, fellow study author Scott Cole, Ph.D., realized a potential link between the disease and sharp brain waves.
Using EEG readings taken from 15 Parkinsons patients and 16 healthy individuals, the team honed in on the unfiltered waves.
The raw signals go up and down like sine waves but with more asymmetry, explains Swann, adding, The steepness the slant turns out to be important in Parkinsons patients.
Indeed, the team noticed that Parkinsons patients who were not taking medication had a sharper peak at the top of their brain wave, compared with the bottom.
Finding that a noninvasive method such as an EEG could be a promising diagnostic tool may have important consequences for the future of the disease. The team is hoping that doctors and researchers can use the test to track changes related to Parkinsons in the brain over the years.
We dont know yet whether this approach will be better, but it could provide easily obtained brain measurements that would be helpful and possibly used in tandem with clinical observations and other EEG measurements, notes Swann.
Read Also: Parkinsons Loss Of Taste
You May Like: What Is The Difference Between Parkinson’s And Huntington’s Disease
Factors That Increase The Risk Of Falling
To understand how to reduce the risk of falling, researchers have studied people with PD to determine the causes of their falls. By knowing why people fall, strategies can be developed to reduce the risk. Increased falls among people with PD are not associated with age or gender. People with PD who seem to be at an increased risk of falling include:
- Those with longer disease duration
- Those taking higher levodopa doses
- Those with stooped posture, balance problems, impaired gait, and freezing episodes
- Those experiencing greater on time with dyskinesia
- Those taking antidepressants or antipsychotic medications, due to their sedating effects
- Those who have cognitive impairment, such as difficulty with multitasking, switching tasks, or solving problems
- Those who experience sleep disturbances, particularly REM sleep disorder
- Those with vision impairments, such as blurry vision or the inability to recognize changes in depth perception1,2
