What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinsons disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinsons disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinsons disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinsons disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinsons disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Dont Miss: Wolff Parkinson White Syndrome Drugs To Avoid
How Is Parkinson’s Disease Diagnosed
Diagnosis is difficult at every stage of the disease, but particularly in the early stages. No single test can provide a diagnosis. A diagnosis will likely involve physical and neurological examinations, conducted over time to assess changes in reflexes, coordination, muscle strength, and mental function. Your doctor might also see how you respond to medicine.
You may need to have brain imaging tests to rule out other conditions that might be causing your symptoms. Such tests could include MRI and CT scans and possibly some other types of scans. Blood tests may also be done to exclude other illnesses.
Rapid Eye Movement Sleep Behavior Disorder
Sleep disturbances are one of the main nonmotor symptoms in PD, including RBD, restless leg syndrome and sleep apnea. High percentages of people with sleep disorders are likely to develop PD, although RBD is found to be in the best correlation with PD progression. RBD is a type of parasomnia linked with repetitive dream enactment behavior and rapid eye movement sleep with the loss of atonia. It is often described as sleepwalking, although it is important to differentiate, as sleepwalking typically occurs in non-REM sleep, while there is rarely dreaming. RBD is identified by polysomnography, with subsequent muscle activity on the electromyogram channels. It has been associated with several types of synucleopathies, including multiple system atrophies, dementia with Lewy bodies and PD . The estimated risk is significantly higher for developing PD in patients with RBD compared to the general population, and once PD is initiated, the motor progression is faster than in patients with no RBD. Compared to other early symptoms, RBD has the highest specificity and predictive value in disease identification, although the need for a polysomnography hinders its clinical use due to the necessitated time and expenses.
You May Like: Prescription For Parkinson’s Disease
Lifestyle And Other Protective Factors
Cigarette smoking and caffeine consumption are the two most consistent protective factors associated with a reduced risk of PD. Other reported associations include higher serum urate, ibuprofen use and exercise, among others. The negative association between cigarette smoking and PD is most intriguing. This inverse relationship is not easily explained, but some have suggested that PD-related cautious personality predisposes some individuals to quitting neuroprotective smoking as the biological mechanism involved in PD. The other hypothesis links nicotine to dopaminergic neuronal protection since it has been shown to stimulate the release of dopamine in the striatum and preserve dopaminergic function in experimental models. It is also possible that there are other unidentified neuroprotective components in cigarette smoke.
The relative risk reduction of PD among caffeine drinkers is between 0.5 and 0.8 and, similar to smoking, a dose-dependent effect has been consistently demonstrated in most studies. Caffeine, an antagonist of adenosine A2a receptor, has been postulated to exert neuroprotective role by blocking this receptor. In addition to caffeine, it is possible that antioxidants present in some beverages may contribute to a protective effect among black tea drinkers, independent of caffeine.
Pharmacological Advances: Charcot And Gowers
Early treatment of Parkinson’s disease. Prescription dated 1877 from the College of Physicians of Philadelphia Library. In treating Parkinson’s disease, Charcot used belladonna alkaloids as well as rye-based products that had ergot activity, a feature of some currently available dopamine agonists. Charcots advice was empiric and preceded the recognition of the well-known dopaminergic/cholinergic balance that is implicit to normal striatal neurochemical activity .
Everything, or almost everything, has been tried against this disease. Among the medicinal substances that have been extolled and which I have myself administered to no avail, I need only enumerate a few .
Vibratory therapy. Charcot observed that patients with Parkinson’s disease experienced a reduction in their rest tremor after taking a carriage ride or after horseback riding. He developed a therapeutic vibratory chair that simulated the rhythmic shaking of a carriage . A vibratory helmet to shake the head and brain was later developed. Such therapies were not used widely but the availability of modern medical vibratory chairs offers an opportunity to confirm or refute Charcots observation.
Read Also: What Are The Stages Of Parkinsons
How Is Parkinson’s Disease Managed
Your doctors will tailor your treatment based on your individual circumstances. You will manage your condition best if you have the support of a team, which may include a general practitioner, neurologist, physiotherapist, occupational therapist, psychologist, specialist nurse and dietitian.
While there is no cure for Parkinson’s disease, symptoms can be treated with a combination of the following.
What Makes Pd Hard To Predict
Parkinsonâs comes with two main buckets of possible symptoms. One affects your ability to move and leads to motor issues like tremors and rigid muscles. The other bucket has non-motor symptoms, like pain, loss of smell, and dementia.
You may not get all the symptoms. And you canât predict how bad theyâll be, or how fast theyâll get worse. One person may have slight tremors but severe dementia. Another might have major tremors but no issues with thinking or memory. And someone else may have severe symptoms all around.
On top of that, the drugs that treat Parkinsonâs work better for some people than others. All that adds up to a disease thatâs very hard to predict.
Read Also: Does Parkinson’s Disease Cause Delusions
Other Ereaders Or Your Computer
To download this course to your computer, please follow these instructions:
If you are transferring to an eReader:
External Link
This link leads outside of the NetCE site to:
While we have selected sites that we believe offer good, reliable information, we are not responsible for the content provided. Furthermore, these links do not constitute an endorsement of these organizations or their programs by NetCE, and none should be inferred.
Disturbances In Autonomic Function
Autonomic dysfunction may present prior to the diagnosis or become apparent with disease progression or be induced by medication . All areas of autonomic function may be affected and this has been reported to affect daily life of over 50% of patients . The autonomic dysfunction is considered because of involvement of both the central and peripheral postganglionic autonomic nervous system . Orthostatic hypotension affects 30â40% of patients. This is defined as a fall in systolic blood pressure of > 20 mm Hg or in diastolic blood pressure > 10 mm Hg on either standing or head-up tilt to at least 60 degrees within 3 min . On assuming the upright posture, hypotension-induced hypoperfusion of the brain can result in dizziness, visual disturbances and impaired cognition that may precede loss of consciousness. In PD, the blood pressure drop may last several minutes . Duration of PD may be unrelated to the occurrence of orthostatic hypotension . In elderly PD patients, this may mainly occur after food intake .
Gastrointestinal symptoms are common. There is slowing of mobility of the gastrointestinal tract with symptoms such as postprandial fullness and gastric retention, but slow-transit constipation is by far the most common, occurring in 70â80% . Patients may also experience difficulties in rectal evacuation because of rectal sphincter dysfunction .
Recommended Reading: Can Botox Cause Parkinson’s
What Are The Symptoms Of Parkinson’s Disease
The main symptoms of Parkinson’s disease are:
- tremor or shaking, often when resting or tired. It usually begins in one arm or hand
- muscle rigidity or stiffness, which can limit movement and may be painful
- slowing of movement, which may lead to periods of freezing and small shuffling steps
- stooped posture and balance problems
The symptoms of Parkinson’s disease vary from person to person as well as over time. Some people also experience:
- loss of unconscious movements, such as blinking and smiling
- difficulties with handwriting
- drop in blood pressure leading to dizziness
- difficulty swallowing
Many of the symptoms of Parkinson’s disease could be caused by other conditions. For example, stooped posture could be caused by osteoporosis. But if you are worried by your symptoms, it is a good idea to see your doctor.
All Masterclass Attendees Carry Out A Workplace Project As A Key Part Of The Course This Will Be On An Issue They Choose In The Area That They Work
All two-module MasterClasses include an intermodule project. This is a workplace project that attendees complete as a key part of the course.
Attendees have free reign over this project. It might be service delivery, patient management or drug treatments, and it could take the form of a service description, an audit, or another form of research. It should meet a local need.
When complete, the project closes with a presentation to the other course members, faculty, and often their managers, commissioners or other people of influence in their area. The group chooses a winner and runner up who receive an award at an evening event, and all projects are shared in our resources section.
You May Like: Physical Therapy For Parkinson’s Gait
Stage Two Of Parkinsons Disease
Stage two is still considered early disease in PD, and it is characterized by symptoms on both sides of the body or at the midline without impairment to balance. Stage two may develop months or years after stage one.
Symptoms of PD in stage two may include the loss of facial expression on both sides of the face, decreased blinking, speech abnormalities, soft voice, monotone voice, fading volume after starting to speak loudly, slurring speech, stiffness or rigidity of the muscles in the trunk that may result in neck or back pain, stooped posture, and general slowness in all activities of daily living. However, at this stage the individual is still able to perform tasks of daily living.
Diagnosis may be easy at this stage if the patient has a tremor however, if stage one was missed and the only symptoms of stage two are slowness or lack of spontaneous movement, PD could be misinterpreted as only advancing age.
Also Check: Parkinsons Disease Side Effects Of Medication
A Review On Parkinsons Disease Treatment
Tori K. Lee Eva L. Yankee
Department of Biology, Angwin, CA 94508, USA .
Correspondence Address: Tori K. Lee, Department of Biology, Pacific Union College, 1 Angwin Ave, Angwin, CA 94508, USA. E-mail: tolee@puc.edu
Received:First Decision:Revised:Accepted:Available online:Academic Editors:Copy Editor:Production Editor:
© The Author 2021. Open Access This article is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, sharing, adaptation, distribution and reproduction in any medium or format, for any purpose, even commercially, as long as you give appropriate credit to the original author and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Also Check: What Are The Early Signs Of Parkinson’s Disease
Diagnosis And Management Of Parkinsons Disease
There are no diagnostic tests for Parkinsons. X-rays, scans and blood tests may be used to rule out other conditions. For this reason, getting a diagnosis of Parkinsons may take some time.
No two people with Parkinsons disease will have exactly the same symptoms or treatment. Your doctor or neurologist can help you decide which treatments to use.
People can manage their Parkinsons disease symptoms through:
- seeing a Doctor who specialises in Parkinsons
Stage Four Of Parkinsons Disease
In stage four, PD has progressed to a severely disabling disease. Patients with stage four PD may be able to walk and stand unassisted, but they are noticeably incapacitated. Many use a walker to help them.
At this stage, the patient is unable to live an independent life and needs assistance with some activities of daily living. The necessity for help with daily living defines this stage. If the patient is still able to live alone, it is still defined as stage three.
You May Like: How Long Does Parkinson’s Last
Can Parkinson’s Disease Be Cured
No, Parkinson’s disease is not curable. However, it is treatable, and many treatments are highly effective. It might also be possible to delay the progress and more severe symptoms of the disease.
A note from Cleveland Clinic
Parkinson’s disease is a very common condition, and it is more likely to happen to people as they get older. While Parkinson’s isn’t curable, there are many different ways to treat this condition. They include several different classes of medications, surgery to implant brain-stimulation devices and more. Thanks to advances in treatment and care, many can live for years or even decades with this condition and can adapt to or receive treatment for the effects and symptoms.
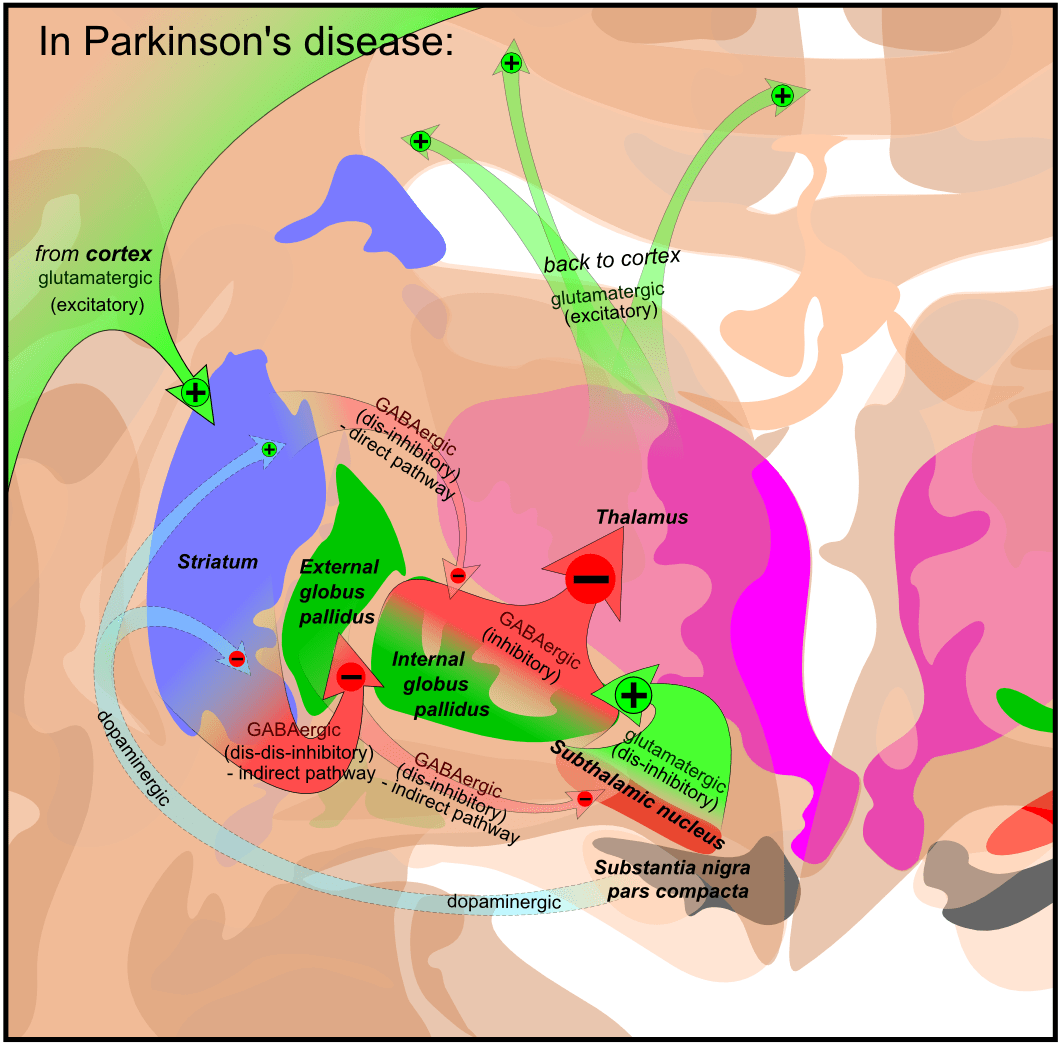
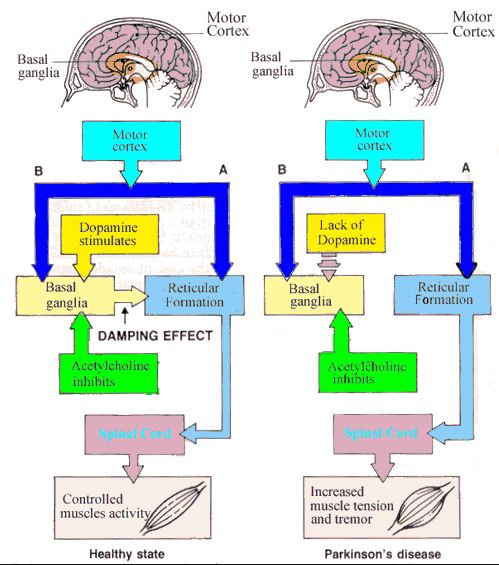
How Does This Condition Affect My Body
Parkinsons disease causes a specific area of your brain, the basal ganglia, to deteriorate. As this area deteriorates, you lose the abilities those areas once controlled. Researchers have uncovered that Parkinsons disease causes a major shift in your brain chemistry.
Under normal circumstances, your brain uses chemicals known as neurotransmitters to control how your brain cells communicate with each other. When you have Parkinsons disease, you dont have enough dopamine, one of the most important neurotransmitters.
When your brain sends activation signals that tell your muscles to move, it fine-tunes your movements using cells that require dopamine. Thats why lack of dopamine causes the slowed movements and tremors symptoms of Parkinson’s disease.
As Parkinson’s disease progresses, the symptoms expand and intensify. Later stages of the disease often affect how your brain functions, causing dementia-like symptoms and depression.
Also Check: How To Prevent Parkinson’s Disease
Theory Of Pd Progression: Braaks Hypothesis
Researchers believe a combination of genetic and environmental factors cause Parkinsons. In 2003, Heiko Braak, MD, hypothesized that an unknown pathogen in the gut could be the cause of PD.
This was followed by a more extensive hypothesis, stating that PD starts in two places: the neurons of the nasal cavity and the neurons in the gut. This is now known as Braaks hypothesis. In this theory, the pathogen enters the body via the nose and/or gets swallowed and reaches the gut. The pathogenic products thus come into contact with the olfactory and/or enteric neurons, triggering the aggregation of an abnormal protein called -Synuclein. The aggregated -Synuclein then spreads toward the central nervous system , and eventually arriving in and causing the degeneration of the dopaminergic neurons in the area of the brain called the substantia nigra.
This theory is supported by evidence that non-movement symptoms, such as a loss of sense of smell, sleep disorders and constipation, may appear several years ahead of movement symptoms. For this reason, researchers focus on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Jun Yu, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
When Should I See My Healthcare Provider Or When Should I Seek Care
You should see your healthcare provider as recommended, or if you notice changes in your symptoms or the effectiveness of your medication. Adjustments to medications and dosages can make a huge difference in how Parkinsons affects your life.
When should I go to ER?
Your healthcare provider can give you guidance and information on signs or symptoms that mean you should go to the hospital or seek medical care. In general, you should seek care if you fall, especially when you lose consciousness or might have an injury to your head, neck, chest, back or abdomen.
Recommended Reading: Diagnosing Parkinson’s Disease Mri
Parkinson Subtypes Progress Differently In Clinical Course And Imaging Pattern
-
Contributed equally to this work with: Carsten Eggers, David J. Pedrosa
Affiliation Department of Neurology, University of Cologne, Cologne, Germany
-
Contributed equally to this work with: Carsten Eggers, David J. Pedrosa
Affiliation Department of Neurology, University of Cologne, Cologne, Germany
-
Affiliation Department of Nuclear Medicine, University of Cologne, Cologne, Germany
-
Affiliation Department of Neurology, University of Cologne, Cologne, Germany
-
Affiliation Department of Neurology, University of Cologne, Cologne, Germany
-
Affiliations Department of Neurology, University of Cologne, Cologne, Germany, Cognitive Neurology Section, Institute of Neuroscience and Medicine , Research Centre Jülich, Jülich, Germany
-
Affiliation Department of Nuclear Medicine, University of Cologne, Cologne, Germany
-
Affiliation Department of Neurology, University of Cologne, Cologne, Germany
How Is Parkinsons Diagnosed
Doctors use your medical history and physical examination to diagnose Parkinson’s disease . No blood test, brain scan or other test can be used to make a definitive diagnosis of PD.
Researchers believe that in most people, Parkinson’s is caused by a combination of environmental and genetic factors. Certain environmental exposures, such as pesticides and head injury, are associated with an increased risk of PD. Still, most people have no clear exposure that doctors can point to as a straightforward cause. The same goes for genetics. Certain genetic mutations are linked to an increased risk of PD. But in the vast majority of people, Parkinsons is not directly related to a single genetic mutation. Learning more about the genetics of Parkinsons is one of our best chances to understand more about the disease and discover how to slow or stop its progression.
Aging is the greatest risk factor for Parkinsons, and the average age at diagnosis is 60. Still, some people get PD at 40 or younger.
Men are diagnosed with Parkinsons at a higher rate than women and whites more than other races. Researchers are studying these disparities to understand more about the disease and health care access and to improve inclusivity across care and research.
Aging is the greatest risk factor for Parkinsons, and the average age at diagnosis is 60. Still, some people get PD at 40 or younger.
The Michael J. Fox Foundation has made finding a test for Parkinsons disease one of our top priorities.
You May Like: Psoriatic Arthritis And Parkinson’s Disease
