What Types Of Care Do Nursing Homes Provide
There are two types of care provided by nursing homes:
- Basic care. This provides services that will help to maintain a person’s ability to carry out necessary daily functions, like personal care and getting around. They will also ensure that the person is supervised and safe.
- Skilled care. This is care that requires the services of a registered nurse for treatments and procedures on a regular basis. Skilled care also includes services provided by specially trained professionals, such as physical, occupational, and respiratory therapists.
A Plan For Parkinsons Patients
UConn Healths Parkinsons Disease and Movement Disorders Center now offers supportive care and planning services, enabling an early start on the long-term prognosis for patients as well as their family members and caregivers.
Parkinsons disease is the second most common neurodegenerative illness after Alzheimers disease, affecting more than one million Americans. Its a progressive condition that leads to loss of dopamine cells in the brain, and the main symptoms associated with it are tremors, stiffness, slowed movements and balance changes.
We Believe That The Secret For A Happy And Healthy Life Is Good Understanding Of The Challenges And Thoughtful Planning
Dr. Bernardo Rodrigues
Who are the best candidates for this service?
Rodrigues: We wish to end the idea that a patient should only learn about their conditions or planning for the future once the disease has advanced. We believe that the secret for a happy and healthy life is good understanding of the challenges and thoughtful planning. We are offering this program to all our Parkinsons disease and Related Disorders patients from the moment of diagnosis.
What are the challenges of living with and/or caring for someone who has Parkinsons disease that people should know before they find out for themselves?
Cournean: Another challenge is the emotional impact that a diagnosis of PD can carry. It is important to monitor how this diagnosis can affect self-esteem. It can cause social embarrassment and isolation or even affect relationships. It is well known that caring for a loved one with chronic diseases can lead to depression, social and financial difficulties. Our SCP program aims to look at each PD patient and his or her family, identifies needs, and helps them to explore an action plan for living their best life as is defined by them.
How does a typical visit or conversation go, and whos part of that conversation?
How do patients, families, or caregivers get connected to this program?
How likely would insurance cover this service?
Read Also: What Year Was Michael J Fox Diagnosed With Parkinson’s
Nursing Care Plan For Parkinsons Disease 4
Nursing Diagnosis: Disturbed Thought Process related to psychological causes, parkinsonian medications, chronic illness, and depression, secondary to Parkinsons disease as evidenced by memory impairment, distractibility, inability to perform activities, abnormal lab studies, and insomnia.
Desired Outcomes:
- The patient will be able to express understanding of the factors that may produce depressive reactions.
- The patient will use different techniques that will effectively decrease the amount and frequency of depressive reactions.
- The patient will show compliance to the different therapeutic regimens.
Theme 2care Partner Preferences For Specific Future Planning
Care partners also desired a comprehensive tool to help navigate future planning. In many cases, care partners were able to specifically describe their need for practical guidance to navigate the PD journey. A care partner from the palliative care arm described,
Knowledge is power, so you need to know how to prepare yourself if you can. One of the things that I would like to know more about is the caregiving later. I was talking to a social worker that said there are real problems down the road financially if you have to go into assisted living, and I need to know more about that to prepare financially.
Table 2 shows questions that both patients and care partners from both standard care and the palliative care arm had about the future. Common questions included what to expect, how to gauge PD-related severity, how to plan for future needs, and who to ask for support. In some cases, questions from care partners incorporated concrete options and related considerations or limitations because they were already thinking far down the road, while patients often felt like they were trying to adjust to current physical and cognitive changes due to PD. When patients were open to discussing future planning, they could identify the change or challenge that would need to be addressed but sometimes were not able to articulate multiple options and decisions.
Table 2
Read Also: Parkinsons Disease Brain Changes
Recommended Reading: Herbicide That Causes Parkinson’s
Q: Will Medicare And/or Private Insurance Cover The Costs Of Palliative Care
A: I can tell you that our Legacy Care Program is covered and does not affect any other payments made by Medicare and/or private insurances. For any other program, I would advise and strongly suggest that you check with the care-providing agency of choice to confirm coverage.
Tips and Takeaways
- Palliative care is a clinical approach that focuses on improving quality of life for people with complex diseases. It can begin at any point during disease progression and work in conjunction with a treatment plan.
- Palliative care programs for PD provide people with PD and their care partners additional resources and check-ins as the disease becomes more complex and difficult to manage. Multi-disciplinary care is provided with a focus on maximizing communication between the team members.
- Palliative care is different from hospice care. Palliative care refers to all treatments throughout the disease course focused on quality of life. Hospice care on the other hand, is provided to improve the quality of life only when end of life is near.
- Discuss the possibility of a palliative care referral with your movement disorders neurologist. A social worker may also be able to connect you with a palliative care program.
Do you have a question or issue that you would like Dr. Gilbert to explore? Suggest a Topic
Dr. Rebecca Gilbert
APDA Vice President and Chief Scientific Officer
Nursing Care Plan For Parkinsons Disease 3
Nursing Diagnosis: Fatigue related to disease process of Parkinsons disease as evidenced by generalized weakness, tremors, muscular rigidity, and verbalization of overwhelming tiredness
Desired Outcome: The patient will demonstration active participation in necessary and desired activities and demonstrate increase in activity levels.
Read Also: Who Gets Parkinson’s Disease
Why Does The Theracycle Cost More Than A Basic Exercise Bike
The Theracycle is not a simple or traditional exercise bike. The biggest difference is the unique motorized technology and the 15-speed variable gearbox, which allows you to attain and maintain a significantly faster cadence for a longer period than you can achieve using a traditional stationary or road bike. A Theracycle has been proven to reduce neurological symptoms and improve motor function and mobility.
Additionally, the bike is custom engineered for the specific needs of people with movement disorders, not only in its open walk-though design, but also when it comes to durability and, most importantly, stability. The Theracycle is built on a very sturdy, heavy structural steel frame. It has a low center of gravity by design, which is ideal for those with balance, dexterity or gait issues providing a safe and secure exercise option in the comfort of your own home. Also important is the motor-assisted handlebar which provides both core and upper body exercise with a repetitive rowing motion for a full-body workout. A Theracycle provides a meditative and relaxing option for both mental and physical therapy that is low impact to your joints and muscles.
Q: What Typically Prompts A Person Treated At Your Parkinsons Center To Be Referred To The Palliative Care Program
The main criterion is that the person with PD meets the Medicare definition of homebound status . We also consider the distance they live from the Muhammad Ali Parkinson Center the further away a patient lives from our center, the more likely they need additional help. Patients that have limited support from family members or need a multi-disciplinary team approach are also candidates for referral.
Read Also: Latest Developments In Parkinson’s Treatment
Nursing Care Plan For Parkinsons Disease 5
Nursing Diagnosis: Impaired Verbal Communication related to the rigidity of facial muscles, lack of stimuli, decreased circulation to the brain, and psychological barriers secondary to Parkinsons disease as evidenced by stuttering, inability to name words, inability to identify objects, inappropriate verbalization, and facial muscle rigidity.
Desired Outcomes:
- The patient will be able to use other methods to communicate and make his or her needs known.
- The patient will be able to use techniques and other assistive devices that will help him or her to improve the patients ability to communicate.
- The patient will be capable of speaking in an understandable way as much as possible.
- The patient will be able to comprehend communication and will be able to exhibit minimal frustration and anxiety with speech attempts.
Clinical Assessment And Outcome Measures
At baseline, t1, and t2, all patients will visit their own hospital for the study assessments, which are performed by a blinded researcher . The patients and their caregivers will also complete home questionnaires. In addition, every 3 months, patients will receive a questionnaire at home regarding healthcare utilization, costs, and productivity loss over the past 3 months. Caregivers will complete a cost questionnaire, including healthcare utilization, costs, and productivity loss, specifically related to caregiver burden. To improve adherence, patients and caregivers can choose whether they prefer to fill out digital or paper-based questionnaires. Participants will be contacted by telephone when they do not complete the questionnaires within 4 weeks. All the outcomes, including secondary outcome measures, can be found in Table .
Table 3 Outcome measures used at different time points
Recommended Reading: Tests For Parkinson’s Symptoms
Eating Drinking And Parkinsons Disease
- Dont rush your meals. Allow the extra time you need to finish your meal. Rest your elbows on the table to provide more motion at your wrist and hand.
- Sit with your knees and hips bent at a 90-degree angle in a straight-back chair.
- Use utensils with built-up, lightweight handles, or use a spork a spoon and fork in one. Use a rocker knife for cutting food.
- Use a non-skid mat to stabilize objects on the table.
- Use a plate guard or plate with a raised lip to prevent food from spilling.
- Use a long straw with a non-spill cup or use a plastic mug with a large handle.
Recommended Reading: Stem Cells For Parkinsons Disease Therapy
How To Talk To A Loved One About Parkinsons Disease
These are some strategies that can be helpful while talking to a loved one about Parkinsons disease:
- Check in regularly: Check in on the person regularly to ask them how theyre feeling and coping.
- Use empathetic language: Parkinsons disease can affect a persons ability to go about their daily life. The person might find it challenging to do things they once did easily. This can be difficult and frustrating for them. Try to be empathetic when you speak to them, so they feel supported.
- Offer assistance: As Parkinsons disease progresses, the person may not be able to drive, cook, clean, or care for themselves. Offer them your assistance and let them know they can count on you.
- Encourage them to settle their affairs: If your loved one is in a position to make important decisions, it can be helpful to encourage them to settle their affairs.
You May Like: What Age Does Parkinson’s Show Up
When Is It Time To Get Outside Help
Answering this question requires understanding and balancing the wants and needs of both the person with Parkinsons and the caregiver.Not everyone wants an extra hand, even when you really need it. It can be hard to accept this reality and deal with the emotions it brings up. However, as your loved ones care needs change, you must continually reevaluate your need for help.
Parkinsons progresses differently in every person. At first you might just need someone to help pick up groceries every now and then. As the disease advances, your needs might evolve to include a day care service, or a home health aide for a few hours at a time. Eventually full-time home care or a skilled nursing facility might be necessary.
How Is Parkinsons Treated
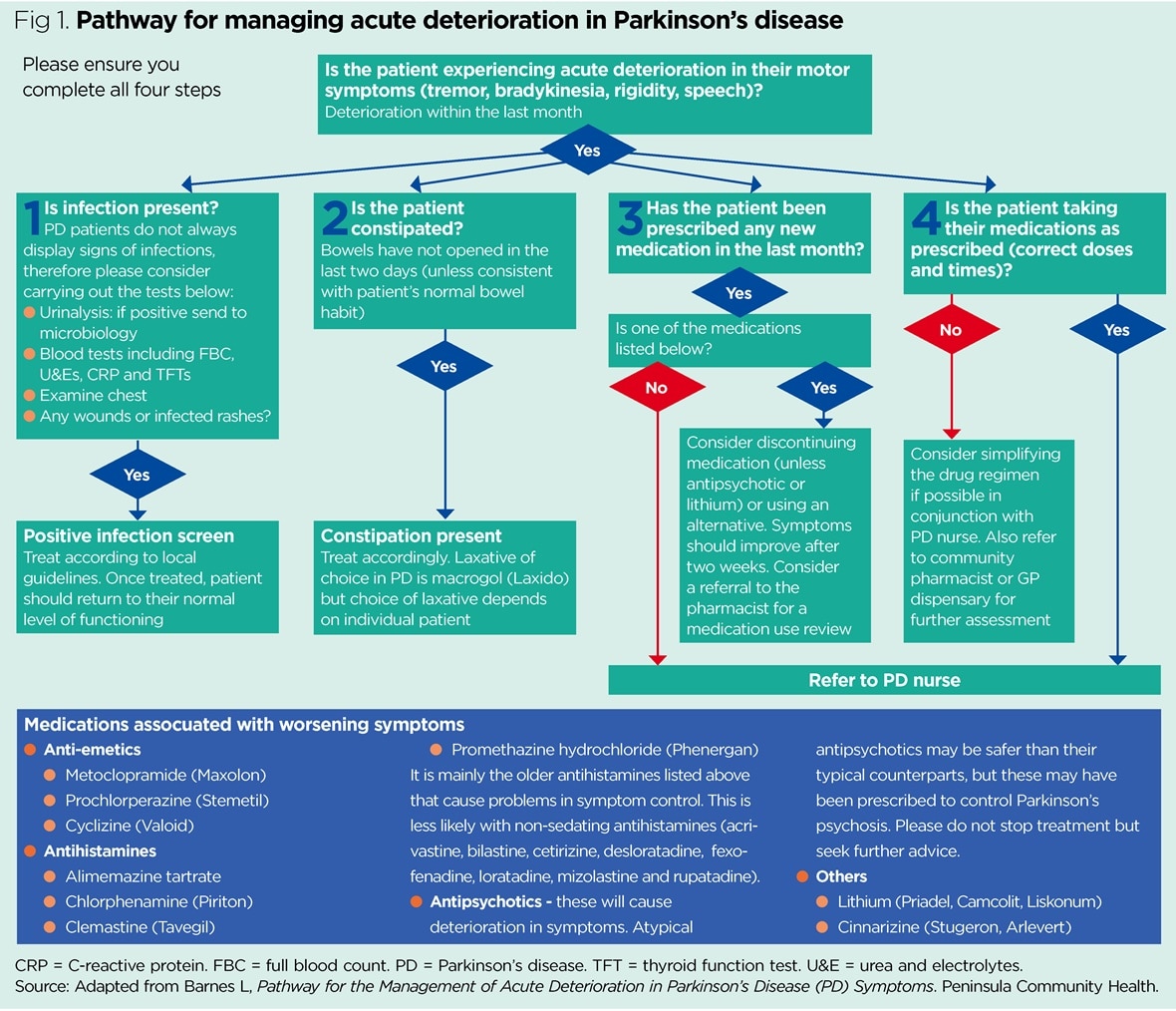
Parkinsons disease can also be broken down into four stages: diagnosis, maintenance, complex and palliative. In the early stages of Parkinsons disease, medication treatment can be very effective. However as the disease progresses into the complex and palliative stages, the individual may become more restricted despite an ideal medication therapy regime.
There is no ideal medicinal treatment for Parkinsons. Therapy will be tailored to the individual, their symptoms, disease progression, lifestyle and physical tolerance. However most medication prescribed to someone with Parkinsons will fit into one of these categories:
- Levodopa dopamine replacement therapy
- Dopamine agonists mimic the action of dopamine
- COMT inhibitors these are used in conjunction with Levodopa and blocks the COMT enzyme to prevent levodopa breaking down in the intestine so more of it will reach the brain
- Anticholinergic block the effect of acetylcholine to rebalance its levels with dopamine
- Amantadine has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors prevent the metabolism of dopamine within the brain
As the disease progresses, medication management for the individual will need to change. However one important factor which must be taken into consideration regarding medications is time. These medications need to be taken on time: if they are taken late, they can severely impair the movements of the person with Parkinsons.
Don’t Miss: Can Parkinson’s Cause Depression
Early Conversations About How Patients See Themselves Living With Parkinsons Disease Helps To Remove The Stigma Of Being Diagnosed With A Chronic Neuro
Elaine Cournean, movement disorders nurse practitioner
The treatment is complex and involves a combination of medications, rehabilitation and support. Medications for Parkinsons disease focus on increasing the dopamine levels in the brain. While new therapies have become available, including surgical options such as deep brain stimulation, there is no cure.
Dr. Bernardo Rodrigues is director of the Parkinsons Disease and Movement Disorders Center within the UConn Health Department of Neurology, and nurse practitioner Elaine Cournean oversees the centers new Supportive Care and Planning program. Here they explain how it can make a big difference in the care for patients and families.
Explain the importance of promoting early support and planning when treating Parkinsons disease?
Rodrigues: Parkinsons disease can negatively affect how patients function in their day-to-day activities, and this program helps guide patients toward a better quality of life. The impact of living with PD not only can affect patients, it can also cause distress in family members and caregivers. Symptoms such as anxiety, depression, cognitive decline, hallucinations and sleep disturbances can be challenging to handle without support.
When did you start offering the Supportive Care and Planning program, and how has it been received?
Developing A Parkinsons Disease Care Plan
If youre caring for a loved one who is living with Parkinsons disease, youre no stranger to the difficulties of this progressive neurodegenerative disorder. Symptoms can vary on a day-to-day basis, and on account of the on/off nature of the disease your loved one may appear fine one moment and need assistance the next.
When caring for a loved one with Parkinsons, youll be working alongside them to develop a Parkinsons disease care plan. This will help them stay accountable for their own health, take their medication regularly, and make strides toward increased independence.
As you work to create a Parkinsons care plan, here are some of the things youll want to keep in mind:
Don’t Miss: What Is Dyskinesia In Parkinson’s
Communication About The Uncertainty Of The Future Disease Burden
The second major theme that emerged from the interviews was the uncertainty of the patients about their future disease burden. The patients reported several concerns about the future that they had not been able to discuss with their HCP. They expressed concerns about ending up in a wheelchair or not being able to take care of themselves anymore and thus becoming a burden for their loved ones or having to live in a nursing home. Almost all patients were afraid to become demented.
Yeah, I find myself wondering: what will become of me? What if I will develop dementia My daughter volunteers at a nursing home for patients with dementia every Sunday. Should I write a euthanasia codicil? Will I remain kind, or will I become a really nasty patient? If that happens, I want it written down somewhere that I do not wish to continue to live.
Respondent 21, female, 56 years old, H& Y stage 2, 1 year since diagnosis
The patients suggested that these important uncertainties about their future disease burden should be addressed in ACP conversations. The patients also reported that ACP conversations should pertain not only to their symptoms but also to the impact of these symptoms on their daily lives. They expressed the wish to get support for activities of daily living, access to devices, or nursing care for personal hygiene. Other aspects which the patients reported that they wanted to address in ACP conversations were resuscitation, hastened death, and nursing care.
Identifying Issues With Current Care
The process begun with a face-to-face meeting to discuss the findings of recent qualitative work exploring the unmet needs of patients with PD , alongside personal experiences of delivering care to this group, in order to identify key issues with the current model of care. These were collated into a list of six main issues with current care and, for each one, an accompanying statement was written to describe the collective vision for what would constitute success in this area .
Don’t Miss: How Was Parkinson’s Disease Discovered
