Clinical Manifestations Of Parkinson’s Disease
Parkinson’s disease remains one of the most common neurodegenerative diseases, affecting 1% of the population older than the age of 65. The last 5 years have been marked by rapid developments in the understanding of the pathophysiology of PD as well as the introduction of a number of new drugs for symptomatic treatment of the disease. The diagnosis of PD is still made on purely clinical grounds, based on the original description by Parkinson in 1817. As a result of continuing advances in therapy, it is increasingly important to recognize PD in its earliest stages. It is no less critical to distinguish PD from other causes of parkinsonism because both prognosis and response to treatment are different.
Changes In Cognition And Parkinsons Disease
Some people with Parkinsons may experience changes in their cognitive function, including problems with memory, attention, and the ability to plan and accomplish tasks. Stress, depression, and some medications may also contribute to these changes in cognition.
Over time, as the disease progresses, some people may develop dementia and be diagnosed with Parkinsons dementia, a type of Lewy body dementia. People with Parkinsons dementia may have severe memory and thinking problems that affect daily living.
Talk with your doctor if you or a loved one is diagnosed with Parkinsons disease and is experiencing problems with thinking or memory.
The Evolution Of Critical Symptoms Involved In Diagnostic Procedures Of Pd
PD is a progressive disorder with multiple symptoms manifesting throughout the years, although there is no definitive sign that could allow direct disease identification. This has resulted in the concept of producing guidelines in the last decades, mainly based on the presence or absence of certain symptoms and responses to therapy. The aims of the developed criteria were to provide a potential route through the set of complex symptoms in order to identify and classify affected patients, thus reducing their disabilities and improving their quality of life.
In 1988, the United Kingdom Parkinsons Disease Society Brain Bank provided the first form of clinical diagnostic criteria for PD by Gibb et al. . This guideline has differentiated three different levels of the classification process, including diagnostic, exclusion and supportive criteria, as described below.
UKPDSBB clinical diagnostic criteria for PD:
Don’t Miss: Can Parkinson’s Go Away
Support For People With Parkinsons Disease
Early access to a multidisciplinary support team is important. These teams may include doctors, physiotherapists, occupational therapists, speech therapists, dietitians, social workers and specialist nurses. Members of the team assess the person with Parkinsons disease and identify potential difficulties and possible solutions.There are a limited number of multidisciplinary teams in Victoria that specialise in Parkinsons disease management. But generalist teams are becoming more aware of how to help people with Parkinsons disease.
Dysfunctional Protein Clearance Systems
There are two central protein clearance systems within cells responsible for the removal of dysfunctional proteins: the ubiquitin-proteasome system and the autophagy-lysosome pathway. The UPS is primarily responsible for breaking down abnormal proteins, and it does so by tagging them with ubiquitin and transporting them to the proteasome for degradation. The autophagy-lysosome pathway is divided into three constituents: macroautophagy, microautophagy, and chaperone-mediated autophagy . Briefly, in macroautophagy, intracellular components, including cytosolic proteins, are engulfed by the autophagosome, which then fuses with the lysosome, leading to the breakdown of its contents. On the other hand, in microautophagy, the lysosome alone engulfs and destroys cytoplasmic components. CMA is a more selective process, whereby molecular chaperones target specific proteins and transport them to the lysosome for degradation . Monomeric -synuclein is generally cleared by both the UPS and the autophagy-lysosome pathway , and damage in either of their machineries is implicated in the pathogenesis of PD by contributing to the accumulation of defective proteins, in particular soluble misfolded -synuclein .
Read Also: Can Parkinson’s Symptoms Be Something Else
Molecular Markers For Pd Identification
One of the main future perspectives is the discovery of molecular alterations that can improve the identification of PD patients. Comprehensive meta-analysis of microarray datasets is a widely accepted strategy to provide information on the altered gene expression levels in pathological conditions. Using this technique, with the combination of the feature selection procedure and classification model, Jiang and colleagues have found 1229 genes with altered expressions in PD patients compared to healthy controls. Nine of the identified alterations were mainly related to the circadian cycle, sleep and gonadotropin-releasing hormone signaling pathway and showed excellent diagnostic values, suggesting potential novel biomarkers of PD . Sakharkar et al. applied a systems biology approach to identify gene expression alterations in PD comparing brain gene expression profiles and peripheral blood cells . They identified 316 genes down- and 98 upregulated in the brain, and 20 of these were differentially expressed in the blood as well. The top three interacting genes with altered expressions were APP, EGFR and PARK2, suggesting the potential cause of dopaminergic neuronal cell death.
How Is Parkinsons Diagnosed
Doctors use your medical history and physical examination to diagnose Parkinson’s disease . No blood test, brain scan or other test can be used to make a definitive diagnosis of PD.
Researchers believe that in most people, Parkinson’s is caused by a combination of environmental and genetic factors. Certain environmental exposures, such as pesticides and head injury, are associated with an increased risk of PD. Still, most people have no clear exposure that doctors can point to as a straightforward cause. The same goes for genetics. Certain genetic mutations are linked to an increased risk of PD. But in the vast majority of people, Parkinsons is not directly related to a single genetic mutation. Learning more about the genetics of Parkinsons is one of our best chances to understand more about the disease and discover how to slow or stop its progression.
Aging is the greatest risk factor for Parkinsons, and the average age at diagnosis is 60. Still, some people get PD at 40 or younger.
Men are diagnosed with Parkinsons at a higher rate than women and whites more than other races. Researchers are studying these disparities to understand more about the disease and health care access and to improve inclusivity across care and research.
Aging is the greatest risk factor for Parkinsons, and the average age at diagnosis is 60. Still, some people get PD at 40 or younger.
The Michael J. Fox Foundation has made finding a test for Parkinsons disease one of our top priorities.
Read Also: Where Is Parkinson Disease Most Common In The World
The Clinical Symptoms Of Parkinsons Disease
Department of Neurology, Broomfield Hospital, Chelmsford, Essex, CM1 7ET UK
Queen Mary School of Medicine and Dentistry, University of London, London, UK
Department of Neurology, Broomfield Hospital, Chelmsford, Essex, CM1 7ET UK
Queen Mary School of Medicine and Dentistry, University of London, London, UK
Read Also: Parkinsons Disease And Sleep
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinsons disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinsons disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinsons disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinsons disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinsons disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Dont Miss: Wolff Parkinson White Syndrome Drugs To Avoid
Read Also: What Is The Sign Of Parkinson Disease
Medications For People With Parkinsons Disease
Symptoms of Parkinsons disease result from the progressive degeneration of nerve cells in the brain and other organs such as the gut, which produce a neurotransmitter called dopamine. This causes a deficiency in the availability of dopamine, which is necessary for smooth and controlled movements. Medication therapy focuses on maximising the availability of dopamine in the brain. Medication regimes are individually tailored to your specific need. Parkinsons medications fit into one of the following broad categories:
- levodopa dopamine replacement therapy
- dopamine agonists mimic the action of dopamine
- COMT inhibitors used along with levodopa. This medication blocks an enzyme known as COMT to prevent levodopa breaking down in the intestine, allowing more of it to reach the brain
- anticholinergics block the effect of another brain chemical to rebalance its levels with dopamine
- amantadine has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors prevent the metabolism of dopamine within the brain.
Stage Two Of Parkinsons Disease
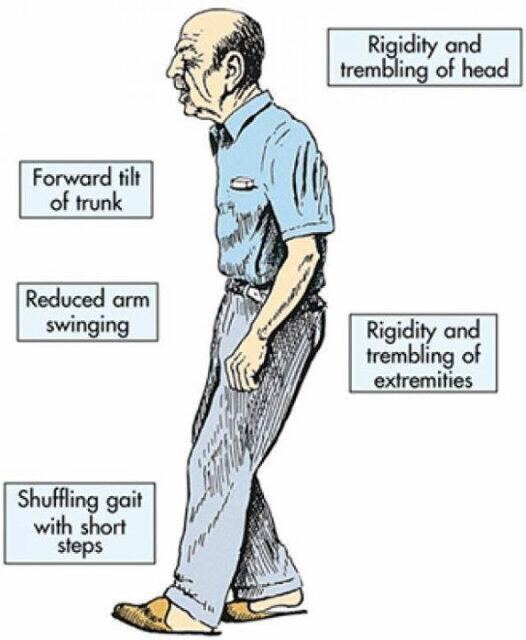
Stage two is still considered early disease in PD, and it is characterized by symptoms on both sides of the body or at the midline without impairment to balance. Stage two may develop months or years after stage one.
Symptoms of PD in stage two may include the loss of facial expression on both sides of the face, decreased blinking, speech abnormalities, soft voice, monotone voice, fading volume after starting to speak loudly, slurring speech, stiffness or rigidity of the muscles in the trunk that may result in neck or back pain, stooped posture, and general slowness in all activities of daily living. However, at this stage the individual is still able to perform tasks of daily living.
Diagnosis may be easy at this stage if the patient has a tremor however, if stage one was missed and the only symptoms of stage two are slowness or lack of spontaneous movement, PD could be misinterpreted as only advancing age.
Also Check: Parkinsons Disease Side Effects Of Medication
You May Like: Has Anyone Been Cured From Parkinson’s
What Causes The Condition
Although there are several recognized risk factors for Parkinsons disease, such as exposure to pesticides, for now, the only confirmed causes of Parkinsons disease are genetic. When Parkinsons disease isnt genetic, experts classify it as idiopathic . That means they dont know exactly why it happens.
Many conditions look like Parkinson’s disease but are instead parkinsonism from a specific cause like some psychiatric medications.
Familial Parkinsons disease
Parkinsons disease can have a familial cause, which means you can inherit it from one or both of your parents. However, this only makes up about 10% of all cases.
Experts have linked at least seven different genes to Parkinson’s disease. They’ve linked three of those to early-onset of the condition . Some genetic mutations also cause unique, distinguishing features.
Idiopathic Parkinsons disease
Experts believe idiopathic Parkinsons disease happens because of problems with how your body uses a protein called -synuclein . Proteins are chemical molecules that have a very specific shape. When some proteins dont have the correct shape a problem known as protein misfolding your body cant use them and can’t break them down.
With nowhere to go, the proteins build up in various places or in certain cells . The buildup of these Lewy bodies causes toxic effects and cell damage.
Induced Parkinsonism
The possible causes are:
Pathogenesis Of Parkinsons Disease
A number of mechanisms have been implicated in PD pathogenesis, with -synuclein aggregation central to the development of the disease. Multiple other processes are thought to be involved, with several studies suggesting that abnormal protein clearance, mitochondrial dysfunction, and neuroinflammation play a role in the onset and progression of PD. However, the relationship between these pathways remains unclear.
Don’t Miss: Does Parkinson’s Affect Breathing
What Can I Expect If I Have This Condition
Parkinsons disease is a degenerative condition, meaning the effects on your brain get worse over time. However, this condition usually takes time to get worse. Most people have a normal life span with this condition.
You’ll need little to no help in the earlier stages and can keep living independently. As the effects worsen, youll need medication to limit how the symptoms affect you. Most medications, especially levodopa, are moderately or even very effective once your provider finds the minimum dose you need to treat your symptoms.
Most of the effects and symptoms are manageable with treatment, but the treatments become less effective and more complicated over time. Living independently will also become more and more difficult as the disease worsens.
How long does Parkinsons disease last?
Parkinsons disease isnt curable, which means its a permanent, life-long condition.
Whats the outlook for Parkinsons disease?
Parkinson’s disease isn’t fatal, but the symptoms and effects are often contributing factors to death. The average life expectancy for Parkinson’s disease in 1967 was a little under 10 years. Since then, the average life expectancy has increased by about 55%, rising to more than 14.5 years. That, combined with the fact that Parkinson’s diagnosis is much more likely after age 60, means this condition doesn’t often affect your life expectancy by more than a few years .
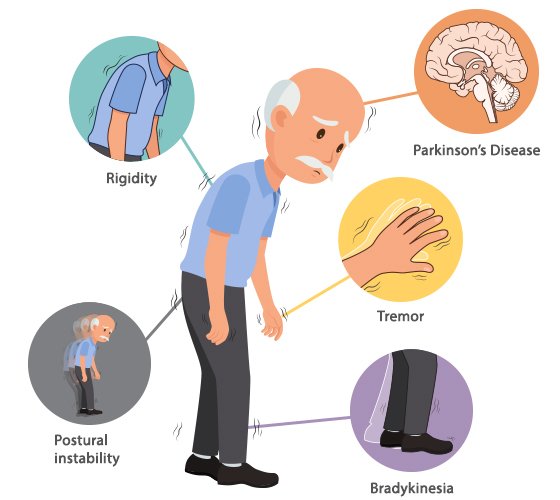
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinsons disease:
- postural instability
Observing two or more of these symptoms is the main way that physicians diagnose Parkinsons.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinsons disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinsons disease has a tremor, nor is a tremor proof of Parkinsons. If you suspect Parkinsons, see a neurologist or movement disorders specialist.
Introducing an easier way to track your symptoms and manage care.
Don’t Miss: Can Parkinson Disease Cause High Blood Pressure
Hereditary Forms Of Parkinson’s Disease And Their Clinical Features
A small but significant number of PD patients have a family history compatible with Mendelian autosomal inheritance , either dominant or recessive. Many of these are classified as young-onset or juvenile-onset PD . A number of levodopa-responsive parkinsonian syndromes have been described and linked to a specific locus or gene in the last few years, and some of them have been classified as PARK syndromes . Some of these denote true PD, whereas others represent more complex phenotypes and dissimilar diseases. Only the former group will be briefly approached here, as the clinical phenotype may be a useful pointer for the diagnosis in daily practice, guiding subsequent molecular testing. For more details on the genetics of PD please refer to Klein and Westenberger .
General Approach To Management
The primary goal in the management of PD is to treat the symptomatic motor and nonmotor features of the disorder, with the objective of improving the patients overall quality of life. Appropriate management requires an initial evaluation and diagnosis by a multidisciplinary team consisting of neurologists, primary care practitioners, nurses, physical therapists, social workers, and pharmacists., It is also important that the patient and his or her family have input into management decisions.
Effective management should include a combination of nonpharmacological and pharmacological strategies to maximize clinical outcomes. To date, therapies that slow the progression of PD or provide a neuroprotective effect have not been identified., Current research has focused on identifying biomarkers that may be useful in the diagnosis of early disease and on developing future disease-modifying interventions.,
You May Like: What Happens If Parkinsons Is Left Untreated
Also Check: Parkinson’s Sleep Disorder Treatment
The Motor Symptoms Of Parkinsons Disease
| Step 1: Diagnosis of Parkinsonian syndrome |
| Bradykinesia |
| Levodopa response for 5 years or more |
| Clinical course of 10 years or more |
- Source: Hughes et al. .
Postural stability may be affected either early or later in the disease process and this may lead to falls and injuries. Early falls are atypical for those who are younger at onset but age is an independent risk factor for falls in PD and, in the elderly, the disease is sometimes first diagnosed in hospitals after a fall. A study by Wood et al. showed that falls occurred in 68% of 109 patients with PD with a mean age of 75 years and mean disease duration of 3 years. Another study reported falls in 62% of patients with PD . Predictors of falls other than older age include duration of disease, dementia, symmetrical onset, postural and autonomic instability .
Oral motor disorders are common. Speech disturbances such as very quiet and hurried speech occur in more than half of the patients , swallowing problems have been reported in 40â80% and a quarter of the patients report dribbling of saliva .
You May Like: Keto Diet And Parkinsons Disease With William Curtis
