Diagnosis Of Excessive Daytime Sleepiness In Pd
In patients describing the symptoms of EDS, it is very important to determine the level of sleepiness. The Epworth Sleepiness Scale is widely used in the evaluation of EDS. Thus, ESS is a useful scale for the subjective assessment of sleepiness in patients with EDS .The ESS contains eight items, and each item is rated as maximum three points. A higher score means more sleepiness level. In addition, there are objective tests such as multiple sleep latency test and maintenance of wakefulness test for assessment EDS. The MWT is evaluation used as a polysomnographic measurement of EDS. The MSLT is measured after a PSG performed in the night to assess nighttime sleep quality and quantity . One study found that the risk of traffic accidents increased in PD patients with an ESS score greater than 7 .
Treatment Of Excessive Daytime Sleepiness In Pd
The first step in the treatment of EDS should be the correction of underlying conditions . For example, it may be useful to treat the conditions that disturb sleep quality at night or to arrange medications that cause daytime sleep episodes. After that, pharmacological treatment options for EDS should be considered. Nonpharmacological treatment approaches can be performed in the treatment of mild to moderate EDS cases . Modafinil is widely used for the symptomatic treatment of EDS, which appears to stimulate catecholamine production . Common side effects of modafinil are insomnia, headache, dry mouth, dizziness, nausea, nervousness, and depression . A review has reported that sodium oxybate and methylphenidate have inadequate evidence that they are effective in the treatment of EDS in PD . Amantadine and selegiline are reported to have an alerting effect . Thus, amantadine and selegiline may be preferentially used in PD patients with EDS.
Signs It Could Be More Than Parkinsons Disease
Feb 9, 2020 | MSA-Blog |
Close to one million people in the US have a diagnosis of Parkinsons disease .Unfortunately, for a small percentage of these people the diagnosis just doesnt seem right. They feel like something more is wrong.Their medicines may not be very effective. They might have severe dizziness and even be prone to fainting.They just sense the disease is progressing faster than expected.
Read Also: Can Parkinson’s Run In The Family
Dyskinesia Cause #: A High
Knowing when, and how, to take medication food can help reduce dyskinesia, says Thomas.
First, youll need to know how levodopa works in the body and how the medication interacts with food: The amino acids found in protein are used in the body and the brain, but first, these acids must pass through the blood-brain barrier the same pathway thats used by levodopa, says Dr. Poston. Because of this so-called traffic congestion, a high-protein meal can interfere with the way the medication is absorbed, worsening the on-off fluctuations that can come with levodopa therapy.
Symptoms Of Parkinson’s Disease
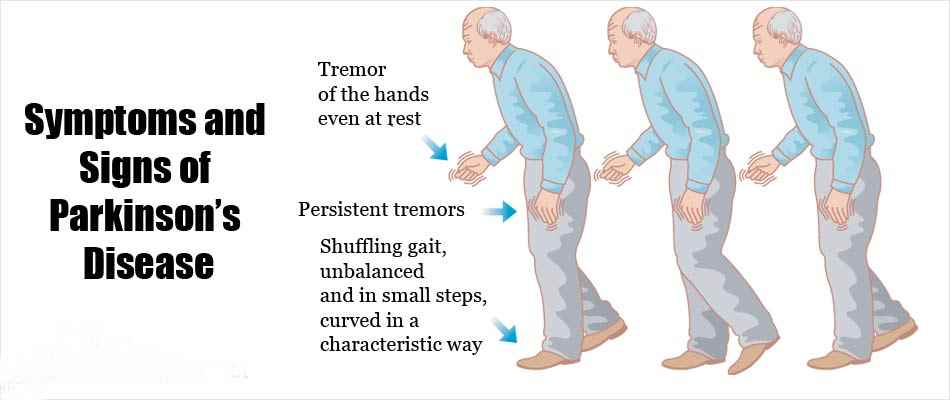
The symptoms of Parkinson’s disease usually develop gradually and are mild at first.
There are many different symptoms associated with Parkinson’s disease. Some of the more common symptoms are described below.
However, the order in which these develop and their severity is different for each individual. It’s unlikely that a person with Parkinson’s disease would experience all or most of these.
Read Also: Stage 4 Parkinson’s Disease Life Expectancy
A Day In The Life Of A Parkinsons Disease Sufferer
A Typical Morning
What is Parkinsons disease?
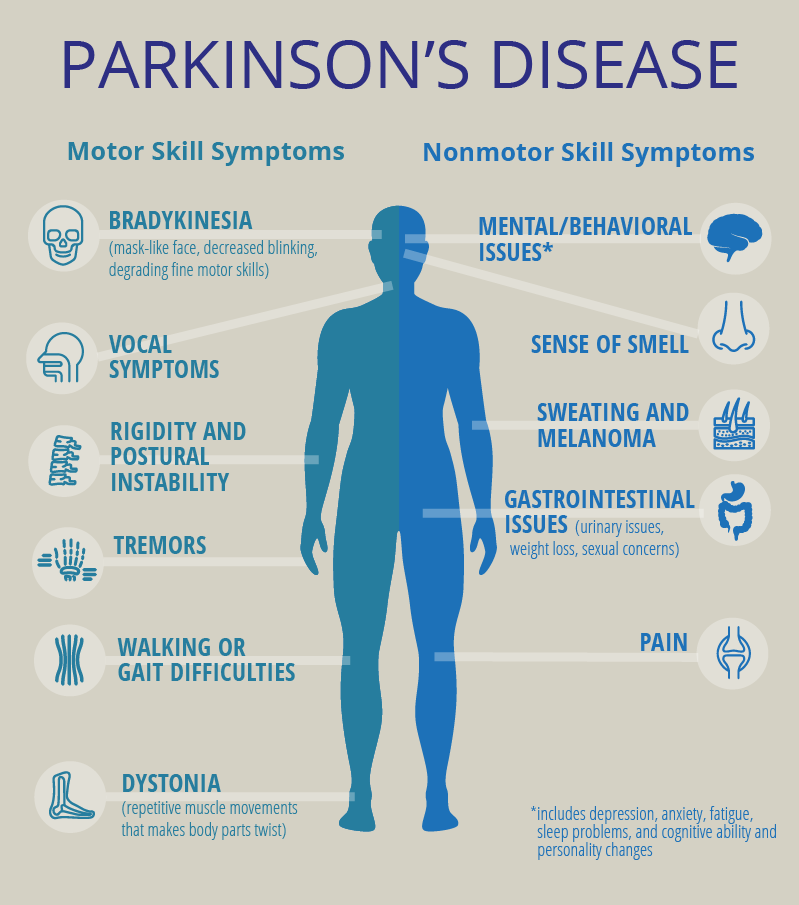
Parkinsons disease is largely thought of as a condition of affecting motor control. James Beck, PhD, vice president of scientific affairs for the Parkinsons Disease Foundation , says that while every case is different, the four cardinal signs of the disease are tremor, muscle rigidity, bradykinesia or akinesia , and problems with walking and balance. These symptoms occur as cells in a part of the brain known as the substantia nigra begin to die off, for reasons that remain unknown. These cells produce an important chemical neurotransmitter known as dopamine. Without dopamine, the brain is unable to control muscle movement. But dopamine is so much more than that. You may have heard it referred to as the happiness neurotransmitter, so its no surprise that two of the non-motor symptoms of Parkinsons disease are depression and apathy. Add to that pain from rigid muscles, blood pressure instability, drooling, sweating, constipation, impaired cognition, and absolutely crushing fatigue, and youve got yourself a disease that affects just about every facet of life. A person with mid-stage Parkinsons disease walking around may look like they are drunk, says Dr. Beck. They commonly have slurred speech, and swallowing is another problem, which can contribute to drooling. This constellation of motor effects looks like drunkenness, but their minds are clear.
Treatment for Parkinsons
Getting Help
Parasomnias In Parkinsons Disease
In PD, parasomnias are quite common, and REM parasomnias are more common than those in NREM . As REM parasomnia in PD, RBD can be seen in near two-thirds of patients . In PD, non-NREM parasomnias can include sleepwalking, confusional arousals, and sleep terrors. However, NREM parasomnias are not a frequent cause of sleep disorders in PD .
Don’t Miss: How Do You Die From Parkinson’s Disease
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinsons disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinsons.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinsons disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinsons disease has a tremor, nor is a tremor proof of Parkinsons. If you suspect Parkinsons, see a neurologist or movement disorders specialist.
Tremors
Rigidity
Bradykinesia
Postural Instability
Walking or Gait Difficulties
Dystonia
Vocal Symptoms
Nighttime Hallucinations Psychosis & Confusion
Nighttime hallucinations and confusion may result from any combination of cognitive impairment, dopaminergic medications, age and PD-related vision changes and lack of sleep. Psychosis may first appear after infection, trauma, surgery or prolonged hospitalization. Symptoms may range from a sensation that someone or something is standing at the side of or behind the person, to very detailed and often frightening visions. Delusions may occur as well.
Treating Parkinsons Psychosis
The first-line approach to treatment of PD psychosis involves simplification of the anti-PD medication regimen and adjusting dose timing , treating other sleep disturbances, providing a consistent and familiar sleep environment , and in more severe cases, the use of atypical antipsychotic drugs.
Most of the available anti-psychotics are always avoided in PD psychosis because they block dopamine receptors and can cause significant problems with movement. However, two anti-psychotic medications, quetiapine and clozapine, are sometimes used as they have less of an ability to worsen motor symptoms. However, data for the use of quetiapine is limited and clozapine requires the patient to undergo frequent blood draws to monitor blood counts. A newer medication pimavanserin, was approved by the FDA to treat PD psychosis. It has a different mechanism of action, and does not block the dopamine system, but rather the serotonin system, and therefore does not increase motor symptoms.
Read Also: How Young Can Parkinson’s Start
What A Survey Of Parkinson’s Patients Shows
De León is not alone in having the pandemic and the virus wreak havoc on her physical and emotional well-being. A survey by the Michael J. Fox Foundation of more than 7,209 patients in spring 2020 found that, among other things, those with PD who contracted COVID-19 experienced new or worsening motor and non-motor symptoms at rates of 63 and 75 percent, respectively. The study also showed that patients with PD who didn’t get COVID-19 but were exposed to the effects of lockdown and not able to participate in their normal activities experienced exacerbated motor and non-motor symptoms by 43 to 52 percent.
Caroline Tanner, a neurologist and coauthor of the survey, which was published in the Journal of Parkinson’s Disease in October, says, It is not surprising there was a worsening of motor problems. We know that when people with PD have anything happen to them, like a , fever or the common cold, that it is not unusual to have a worsening of their Parkinson’s symptoms.”
Labor Day Membership Sale
Join AARP for just $9 per year when you sign up for a 5-year term. Limited time offer.
The worsening of non-motor symptoms, including mood changes, is a bit trickier to explain. Tanner, who is also a professor at the University of California, San Francisco, says this could be due to the social isolation of the pandemic, coupled with the fact that depression is more common in people with PD than in other people of the same age and sex.
Why Do Parkinsons Patients Have Trouble Sleeping
Despite having daytime tremors, Parkinsons patients do not shake in their sleep. However, both Parkinsons disease itself and the medications used to treat it can give rise to a number of sleep problems that lead to insomnia and excessive daytime sleepiness.
Patients with motor symptoms may have trouble adjusting sleeping positions to get comfortable. Others may experience distressing nocturnal hallucinations when trying to fall asleep. These may be a result of medications or cognitive impairment.
In turn, excessive daytime sleepiness may occur as a consequence of sleeping poorly at night. It may also be triggered by medications. Parkinsons patients who suffer from EDS may be at a higher risk of accidents and unable to safely carry out activities such as operating a motor vehicle.
Since insomnia frequently goes hand-in-hand with anxiety and depression, it may be a contributing factor to sleep problems in people with Parkinsons disease. For that reason, doctors often look for mental health disorders in people with Parkinsons disease who have sleep problems.
Also Check: Is Parkinson’s Genetically Inherited
Depression And Other Mood Disorders
Depression and mood disorders from Parkinsons disease are common. Why? PD causes a decline in the neurotransmitter dopamine .
Dopamine plays a key role in controlling and coordinating movement, but its also involved in regulating your mood. Its decline may cause mood changes, but the link between PD and depression is not entirely understood, though it affects an estimated 35% of people with the disease.
Mood disorders also may occur because you are living with a disease for which theres no cure an estimated one-third of people with chronic diseases develop depression, according to the Cleveland Clinic. If you notice such changes, tell your doctor. Treatment can help. Mood changes may also be caused by certain PD medications. If this is happening to you, talk to your doctor, who might be able to alter your regimen.
Sleep Disorders Parkinson’s Foundatio
It didn’t appear again for two years and now it is back worse than ever! I would like to know if Parkinson’s symptoms can present as sensory issues and if Parkinson’s symptoms tend to disappear for long periods of time and then come back unannounced in the early stages? in initiation of movement. Another one that came and went was sleep. Going to the bathroom at night will likely get worse- 60% of folks with PD will develop nocturia- the urge to urinate many times a night. Often caregiver spouses are telling us they were getting up 5-10 times a night to help their partner- there is no way fro them to survive lack of quality sleep The term sundowning refers to a state of confusion occurring in the late afternoon and spanning into the night. Sundowning can cause a variety of behaviors, such as confusion, anxiety, aggression or ignoring directions. Sundowning can also lead to pacing or wandering. Sundowning isn’t a disease, but a group of symptoms that occur at a.
Read Also: How To Take Mannitol For Parkinson’s
How Common Is Parkinson’s Disease Psychosis
Between 20-40% of people with Parkinsons report the experience of hallucinations or delusions. When followed as the disease progresses over the years, this number increases. The increase does not mean that the hallucinations are persistent across the majority of patients. However, it is important to note that these statistics sometimes include delirium, in which the symptoms are temporary due to medication that needs to be adjusted or infection that needs to be treated, and isolated minor symptoms or minor hallucinations, including illusions, where instead of seeing things that are not there , people misinterpret things that are really there. These are the most common types of psychosis in people with PD, with different studies placing the occurrence between 25-70% of people with Parkinsons. Typically, if the person with PD only has these minor hallucinations, their doctor will not prescribe an antipsychotic medication, though more significant psychosis that requires medication may develop over time. In one study, 10% of those with minor hallucinations had their symptoms resolved within a few years, while 52% saw their symptoms remain the same and 38% saw their psychosis symptoms get worse.
We recommend that people with Parkinsons not use a single percentage to represent the prevalence of hallucinations and PDP. Parkinsons is a complex disease and as it progresses the percentages and risk of symptoms will change.
Clinical Features Of Insomnia
Insomnia is defined as difficulties initiating sleep , sleep maintenance problem or early awakening . In studies, it has been reported that the frequency of insomnia in patients with PD varies from 27 to 80% . It has been reported that the most common types of insomnia in PD patients are sleep fragmentation , and early awakenings . It has been reported that insomnia may occur alone or accompany comorbid mental or systemic illnesses, and it is associated with disease duration and female gender . Sleep fragmentation is defined as a deterioration of sleep integrity , and it leads to a lighter sleep or wakefulness . In studies, it has been reported that sleep fragmentation is the most common sleep disorder in patients with PD .
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
What Is Pap Therapy For Osa
PAP therapy involves the use of a nasal interface to mechanically deliver pressurized air to the upper airway while the user sleeps. This delivery system essentially splints the airway open, preventing its collapse and keeping the airway unobstructed. The different kinds of PAP include:
- CPAP = Continuous positive airway pressure
- BiLevel PAP = BiLevel positive airway pressure
- AutoPAP = Autotitrating positive airway pressure
- ASV = Adaptive servoventilation
How Does Parkinsons Disease Cause Sleep Problems
Researchers have yet to uncover every nuance of the Parkinsons and sleep connection. So far, medical experts believe several causes may contribute:
- Chemical changes in the brain: Ongoing research shows that Parkinsons disease may disrupt sleep-wake cycles. Changes to certain brain chemicals may cause people with Parkinsons to get less sleep.
- Medication: Some drugs that treat Parkinsons disease may make it harder to fall or stay asleep. A medication may also disrupt your sleep patterns by making you drowsy during the day .
- Mental health challenges: People with Parkinsons commonly deal with mood disorders, such as anxiety or depression. Any mood disorder may keep you up at night or make you sleep less soundly.
- Parkinsons symptoms: Pain, waking up at night to pee or other Parkinsons symptoms can make restful sleep harder to come by. Sleep apnea can also disrupt sleep.
Also Check: What Are Early Warning Signs Of Parkinson’s Disease
What Does Osa Look Like
OSA is a sleep breathing disorder with several identifiable risk factors. Sleeping partners may have witnessed their loved ones choking or gasping for air in their sleep. Also, snoringthough not proof alone of OSAis still suspect if its loud and frequent.
OSA is identified as pauses of breathing during sleep which last at least 10 seconds each and which occur five times or more per hour, on average, during a full nights sleep. By comparison, healthy people without OSA experience less than three episodes of breathing pauses per hour per night.
When these pauses occur, a flurry of other processes within the body take flight: higher blood pressure and pulse, the release of stress hormones, and shifts in insulin-glucose ratios.
When experienced repeatedly over the long-term, but left untreated, OSA is a leading cause for many chronic health issues, including cardiovascular disease, hypertension, type 2 diabetes, major depression, and anxiety disorder. Untreated OSA is also a significant cause of motor vehicle accidents and dangerous mistakes and errors that occur during the day as a result of lingering daytime sleepiness.
Other classic symptoms include frequent nocturnal awakenings, and a variety of sensations upon awakening, such as shortness of breath, sore throat, dry mouth, and headache.
Parkinsons Disease Sexuality And Practical Suggestions
Every couple affected by Parkinsons has a different experience. Generally speaking, you could try to:
- Learn about the effects Parkinsons and its treatment can have on sexuality.
- Appreciate and recognise the emotional stress you are both going through, even if you are going through it differently. Make every effort to show love, respect, warmth and togetherness in non-sexual ways.
- Talk frankly and openly about sexual needs. Communication is the best remedy for all types of relationship problems.
- Experiment with different routines for example, switch lovemaking to the morning when Parkinsons symptoms tend to be less pronounced or when you have better mobility .
- Place the emphasis on different physical expressions of lovemaking for example, foreplay, touching and kissing rather than penetration.
- Explore and practice different, comfortable positions for successful and pleasurable penetration.
- Adopt new sexual roles according to your and your partners abilities.
- Find new solutions for physical stimulation .
- Work together with medical staff to reduce the effects of medications on sexual function.
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
